Chapter 109
Long-Term Acute Care in the Spectrum of Critical Care Medicine
Evolution of Long-Term Acute Care and the LTAC Hospital
In the 1980s and early 1990s, “weaning hospitals,” which were based on an extension of principles derived from facilities caring for individuals with tuberculosis, focused on patients who required significantly longer stays than those for which the IPPS was designed—namely, patients requiring respiratory care and ventilator weaning. These typically freestanding LTACs were large enough to support small hospital operations, including meal service, physical therapy, and administrative and financial systems. Many were built and operated by a limited number of for-profit companies using private or investment equity. Designed as regional centers aimed at drawing patients from several acute-care hospitals, these early “weaning hospitals” were located in proximity to acute-care referral sources. These facilities also spawned growth of for-profit, specialty hospital chains.
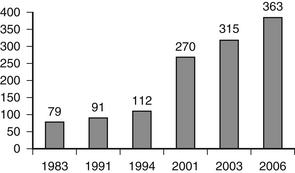
After nearly 20 years of continuously escalating costs, in 2003 Medicare initiated a prospective payment system for LTAC facilities. Based on “long-term care diagnosis-related groups” (LTC-DRGs), payment to an LTAC is now tied to the patient’s principal diagnosis. Currently, more than 975 LTC-DRGs exist. Despite the implementation of LTC-DRGs attempting to manage escalating costs, the number of LTACs has increased further to nearly 400 (Figure 109.1). Medicare expenditures to LTACs have also ballooned to an estimated $5.27 billion in 2007. In 2008, CMS froze payments at the 2007 rate, and the agency is presently considering other cost containment measures, including a 3-year moratorium on new LTAC hospital beds.
Geographic Distribution of LTACs
For unclear reasons, a unique geographic distribution of LTACs has evolved. Unlike the case for post-acute facilities, characterized by a fairly homogeneous distribution of inpatient rehabilitation or skilled nursing facilities across the country, LTACs appear highly concentrated in certain regions. In particular, LTAC facilities predominate in the northeastern and southern parts of the United States, with 35% of all facilities in three states (Massachusetts, Louisiana, and Texas). Northern states have the majority of the older hospitals; most of the newer, respiratory-based facilities are in southern states. A variety of factors related to the origins of these hospitals, state-specific legislation relating to certification of need, and unique demographics may account for this significant variability in distribution.
< div class='tao-gold-member'>