INTRODUCTION
Before the availability of local anesthetics, local pain control for lacerations, fractures, and minor surgery was achieved by minimizing the pain response centrally, typically with opiates or alcohol. Procaine, which entered clinical use in 1904, was the only local anesthetic available for almost 40 years, but the short duration of action and high rate of allergic reactions limited its effectiveness. Lidocaine was introduced in 1943 and continues to be the local anesthetic most commonly used in the ED.1,2 Additional local anesthetics are available for both topical and injectable use (Tables 36-1 and 36-2). Emergency physicians commonly use local and regional anesthetic techniques for potentially painful procedures performed in the ED.3 Regional anesthesia can also be used to control the pain of acute injuries and reduce the utilization of systemic analgesics.4,5
| Agent | Active Ingredients | Application | Time to Effectiveness | |
|---|---|---|---|---|
| Intact Dermis | ||||
| Eutectic mixture of local anesthetic agents (EMLA®) | Lidocaine 2.5% Prilocaine 2.5% | Apply thick layer, 5–10 grams (maximum 20 grams), to area to be anesthetized; cover with semiocclusive dressing. | 60 min | |
| Tetracaine (amethocaine) gel (Ametop®) | Tetracaine 4% | Apply 1 gram (one tube) to area to be anesthetized; cover with occlusive dressing. | 30 min | |
| Liposome encapsulated tetracaine | Tetracaine 5% | Apply 0.5 gram to area to be anesthetized. | 60 min | |
| Liposome encapsulated lidocaine (LMX4® and LMX5®) | Lidocaine 4% or 5% | Apply 2.5 grams to area to be anesthetized. | 30–60 min | |
| Open Dermis | ||||
| Lidocaine, epinephrine, tetracaine (LET) | Lidocaine 4% Epinephrine 0.1% Tetracaine 0.5% | Apply 5 mL to gauze pad placed into wound; cover with semiocclusive dressing. | 20–30 min | |
| Mucosa | ||||
| Topical anesthetic gel (ZAP®) | Benzocaine 18% Tetracaine 2% | Apply 0.2 mL (one dispenser application) with cotton swab to area to be anesthetized. | 5 min | |
| Benzocaine spray (Hurricaine®) | Benzocaine 20% | Apply 1-s spray to area to be anesthetized; volume delivered is highly dependent on canister orientation and residual volume. | 15–30 s | |
| Viscous lidocaine | Lidocaine 2% | Apply 10–15 mL to area (e.g., topical anesthesia before upper airway procedures). | 2–5 min | |
| Agent | Lipid Solubility* | Protein Binding | Duration† (min) | Onset‡ (min) | Maximum Dose (milligrams/kg, with epinephrine) | Concentration (subdermal use) | Concentration (regional anesthesia use) |
|---|---|---|---|---|---|---|---|
| Amides | |||||||
| Bupivacaine | High | High | 200+ | 10–15 | 3 (5) | 0.50%–0.75% | 0.25%–0.50% |
| Lidocaine | Medium | Medium | 30–60 | 5 | 4 (7) | 0.5%–1.0% | 1%–2% |
| Levobupivacaine | High | High | 200+ | 10–15 | 2 | 0.25% | 0.50% |
| Mepivacaine | Low | Low | 45–90 | 3 | 4 | 0.5%–1.0% | 1%–2% |
| Prilocaine | Medium | Medium | 30–90 | 5 | 5 | 4% | NA |
| Ropivacaine | Medium | Medium | 200+ | 5–15 | 3 | 0.5% | 0.5% |
| Esters | |||||||
| Procaine | Low | Low | 40 | 15–20 | 7 | 0.25%–0.5% | 0.5%–2.0% |
| Chloroprocaine | Low | Low | 45 | 5 | 8 | 1%–2% | 1%–2% |
| Tetracaine (amethocaine) | High | High | 200 | 15 | 1.5 | NA | 0.2%–0.3% |
| Alternatives for patients with reactions to amides and esters | |||||||
| Diphenhydramine# | 25 | 1% | NA | ||||
| Benzyl alcohol with epinephrine f | 15–25 | 0.9% | NA | ||||
LOCAL ANESTHESIA
Local anesthetics are divided into two classes: esters and amides.1,2 Both classes work by reversibly blocking sodium channels and inhibiting the propagation of nerve impulses.1,2 Sodium channel blockade first affects the smaller nerve fibers, causing a reduction in pain and temperature sensation, followed by loss of touch, deep pressure sensation, and, finally, motor function. Esters are hydrolyzed by cholinesterase enzymes in plasma, whereas amides are metabolized by hepatic microsomal enzymes. Onset of action, duration of anesthesia, and potential for systemic toxicity are the three primary factors in selecting a local anesthetic.
The onset of action of a local anesthetic is dependent on the pKa (the pH at which 50% of the drug is ionized and 50% of the drug is nonionized). If the ambient pH is higher than the pKa of the agent, a greater percentage of the drug will be in the nonionized form, which diffuses more rapidly across lipid membranes, and the onset of action is shorter. Thus, drugs with a lower pKa have a more rapid onset of action. The pH of available local anesthetic solutions is acidic, varying from 3.3 to 6.8, depending on the agent, additives, and buffers. The duration of action of the local anesthetics is a function of receptor affinity. Agents with a higher receptor affinity (e.g., bupivacaine, ropivacaine, levobupivacaine) have a longer duration of action than those with lower receptor affinity (e.g., lidocaine, prilocaine).6 Selecting agents with a longer duration of action provides superior results for long procedures or for those in which postprocedure analgesia is desired. Longer-acting agents also offer continued analgesia when providers are pulled away from the procedure. The downside of long-acting agents is the greater risk of systemic toxicity.7 Levobupivacaine8 and ropivacaine9 appear to have a lower risk of systemic toxicity than bupivacaine.
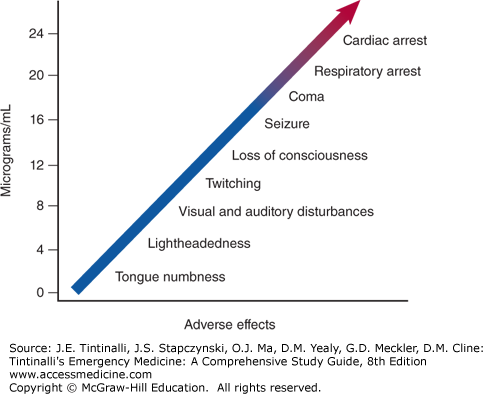
The systemic toxicity of local anesthetics occurs with dose-related clinical progression of sodium channel blockade in nontarget tissues, primarily the brain and heart.10,11 Toxicity can range from subtle neurologic symptoms to refractory seizures and, ultimately, cardiovascular collapse (Figure 36-1).12,13,14 The risk of systemic toxicity can be reduced by adherence to dose limitation and techniques to minimize systemic absorption.15,16,17,18 Seizures due to neurologic toxicity should be treated with benzodiazepines.19 Typical agents used to treat cardiac arrest (e.g., vasopressin) and tachyarrhythmias (e.g., β-blockers and calcium channel antagonists) should be avoided in the setting of local anesthetic systemic toxicity.19 IV 20% lipid emulsion is an effective treatment for systemic toxicity from local anesthetics, especially if due to bupivacaine with its high lipid solubility.19, 20, 21, 22, 23, 24, 25, 26, 27 Published reports have utilized different dosing protocols, but one consensus guideline recommends an initial dose of 20% lipid emulsion, 1.5 mL/kg infused over 1 minute with continuous infusion or repeat doses according to the clinical condition.19 The recommended maximum dose is about 10 mL/kg over the initial 30 minutes.19
Prilocaine and benzocaine can cause the oxidation of the ferric form of hemoglobin to the ferrous form, creating methemoglobin that becomes visible as cyanosis when methemoglobin concentration exceeds 1.5 grams/dL.
When using any local anesthetic, calculate the volume and concentration of drug used, especially when treating smaller patients or tending to large wounds (Table 36-2). Aspiration before injection helps to avoid inadvertent deposit of local anesthetic in a vein or artery. When the use of a large quantity of local anesthetic seems unavoidable, procedural sedation or alternative regional blocking techniques and supplementation with systemic analgesics or anxiolytics should be considered (see chapter 37, Procedural Sedation).
The addition of epinephrine to the injected local anesthetic solution increases the duration of anesthesia, helps to control wound bleeding, and slows the systemic absorption.28 The use of local anesthetic with epinephrine is safe for use in end-arterial fields (fingers, toes, etc.) in selected healthy patients,29, 30, 31, 32, 33, 34 but probably should be avoided in suspected digital vascular injury; patients with vascular disease, such as Raynaud’s or Berger’s disease; or other conditions in which end-arterial vascular supply is problematic. An alternative to epinephrine is clonidine (U.S. Food and Drug Administration unlabeled use), an α-adrenergic agonist, which can also be used in combination with a local anesthetic to prolong the duration of anesthesia.35,36,37 A dose of 0.5 micrograms/kg of clonidine (maximal dose 150 micrograms) can be mixed with the anesthetic to prolong the duration of anesthesia by >50%. Do not exceed a maximal dose of 150 micrograms because sedation, hypotension, and bradycardia can result.36,37
Adverse reactions to local anesthetics are most often local reactions to preservatives or the epinephrine in the solution, and true allergic reactions are extremely rare.38,39 In patients with true allergies to local anesthetics, two nontraditional agents can be used for wound repair via local injection—diphenhydramine and benzyl alcohol (Table 36-2).40,41,42
The addition of sodium bicarbonate to local anesthetics shortens the onset of action by raising tissue pH and reduces the pain of injection.3,43,44,45 Lidocaine can be buffered by adding 1 mL of sodium bicarbonate 8.4% (1 mEq/mL) to 9 mL of 1% lidocaine. Bupivacaine can be buffered by adding 1 mL of sodium bicarbonate 8.4% (1 mEq/mL) to 29 mL of bupivacaine 0.25%. However, the addition of bicarbonate can cause precipitation of the anesthetic agent (most prominently bupivacaine) and accelerate the degradation of epinephrine in the solution, so bicarbonate should not be added to the anesthetic unless it can be used immediately. Additional means of reducing the pain of infiltration include the use of a 27- to 30-gauge needle, slow injection, warming the solution to body temperature, and injecting through the margins of a wound rather than through intact skin surrounding the wound.3,43, 44, 45, 46, 47, 48
Local anesthetics can be administered topically, intradermally, subdermally, or infiltrated near peripheral nerves. When considering which approach best meets the patient’s needs, many factors should be considered. In the setting of wound management, these include patient factors (age, anticipated pain tolerance, comorbidities), wound factors (location, depth, presence or absence of contamination, and/or neurovascular injury), and technical factors (time required, clinician experience). Clinical judgment combined with individual patient needs should dictate the best approach.
TOPICAL ANESTHESIA
Topical anesthetics are used in three major situations: on intact skin before dermal instrumentation, applied to intact mucosa, and placed on open skin for pain control or before wound repair.49,50,51 Topical anesthetics are probably as effective as local anesthetic infiltration for suturing of many dermal lacerations, although the comparison studies are of modest quality.52
An alkaline (pH approximately 9) cream mixture of lidocaine and prilocaine [eutectic mixture of local anesthetics (EMLA®)] was the first topical anesthetic formulated to penetrate intact skin. When applied for at least 60 minutes under a semiocclusive dressing before dermal instrumentation, this lidocaine/prilocaine mixture is as efficacious as the infiltration of local anesthetic and is ideal for venous catheter insertion and lumbar puncture. Liposome-encapsulated tetracaine, liposome-encapsulated lidocaine, and tetracaine gel have all been compared to the lidocaine/prilocaine mixture and found to be equally efficacious (Table 36-1).53,54,55,56,57
The tetracaine, epinephrine, and cocaine mixture is a topical anesthetic used on open dermis. Due to the potential for CNS and cardiovascular toxicity, the cocaine component of this combination has been replaced with lidocaine. This mixture—lidocaine, epinephrine, and tetracaine—has a variety of formulations and is usually compounded by the hospital pharmacy in accordance with the concentration preferences of local clinicians. A common version is 4% lidocaine, 0.1% epinephrine, and 0.5% tetracaine prepared in 5-mL vials.
INTRADERMAL AND SUBDERMAL ANESTHESIA
Intradermal injection produces a visible wheal, whereas subdermal injection does not. Intradermal injection produces more immediate pain upon injection due to stretching of the compact dermal structure, but can enhance the anesthetic effect by applying pressure to and numbing the cutaneous pain sensors. Intradermal injection raises the skin surface and is useful when shaving off a cutaneous lesion. Subdermal injections have a slower onset of action, are less painful, and are the most commonly used method of achieving local anesthesia in the ED and for office-based surgery.3,58 Local anesthetics may be delivered directly into the subdermal space in most clean lacerations or as a field block for contaminated wounds.
In addition to modifying the injected solution, a variety of techniques are used to reduce the pain of needle puncture and local anesthetic injection43,44,45,59: application of a topical anesthetic prior to injection,60,61 warming the local anesthetic agent,46,47,48 stretching the skin at the puncture site, vibrating the skin adjacent to the area,62,63 talking during the process to distract the patient, inserting the needle through enlarged pores or hair follicles, inserting the needle with bevel up position,64 or numbing the skin with an aerosol refrigerant.65,66,67,68,69
REGIONAL ANESTHESIA
Regional anesthesia is a technique that infiltrates local anesthetic agents adjacent to peripheral nerves (“nerve blocks”) and is typically used for complicated lacerations, abscesses, fractures, and dislocations.70,71,72 Providing adequate anesthesia quells patient anxiety, provides greater patient satisfaction, and increases the likelihood of an optimal result when treating complex injuries. With careful technique, serious complications from peripheral nerve blocks are uncommon.73,74,75 Assess and document distal neurovascular status before application of a regional nerve block to prevent masking a primary traumatic neurovascular injury. Distal vascular function is assessed by noting skin color and temperature, measuring capillary refill time, and palpating pulses. Distal neurologic function is assessed by noting cutaneous sensation (pain, touch) and motor function (active movement, strength). For digital injuries, assess digital nerves by determining two-point discrimination on the volar pad before anesthetic injection. Normal two-point discrimination is <6 mm at the fingertips and is often <2 mm. Compare the injured digit with the contralateral normal digit.
Regional anesthesia for laceration repair eliminates wound distortion caused by large-volume subdermal injection. Regional anesthesia on the extremities provides superior pain control when compared with subdermal infiltration of anesthetic.70 Topical anesthetic before peripheral nerve blocks can minimize the pain associated with the block.53,54,55,56,57,60,61
When selecting a local anesthetic for regional anesthesia, consider the onset of clinical effects, duration of analgesia, and risk of toxicity.70 Although lidocaine continues to be the most popular agent, bupivacaine, levobupivacaine, and ropivacaine offer a longer duration of action, with levobupivacaine and ropivacaine being significantly less cardiotoxic.6,8,9 Peripheral nerve blocks require time to achieve optimal analgesia, approximately 10 to 20 minutes for lidocaine and 15 to 30 minutes for bupivacaine. Pain and temperature sensation are affected first, followed by loss of touch, deep pressure, and then motor function. Intraneural injection of anesthetic causes significant pain.76 Thus, if excessive pain upon injection is noted, withdraw the needle a few millimeters, and after pain abates, resume the injection.
The regional nerve blocks commonly performed by emergency physicians are often done using the “landmark” technique to identify the site of local anesthetic injection.70 The major disadvantage of the landmark approach is anatomic variation. Large volumes of anesthetic are typically administered, in case the needle tip is not close to the desired nerve. Two devices in common use help localize and direct the needle to maximize the rate of successful anesthesia: a peripheral nerve stimulator using electrically insulated needles and US guidance to localize the nerve.77,78,79,80,81 US guidance shortens the block performance time, reduces the number of needle passes, and enables blocks to be performed using lower anesthetic doses.82,83,84 Training to use US-guided regional anesthesia in the ED typically involves a didactic session, supervised practice in ultrasonographic identification of the relevant structures, and procedural practice on simulation mannequin.85,86 The use of US is recommended when performing more complex nerve blocks.
The performance of peripheral nerve blocks requires an element of hand–eye coordination that is difficult to display in words and photographs.
Purpose A digital nerve block provides anesthesia to the entire digit and is an excellent block when tending to lacerations of the fingers or toes, drainage of paronychia, finger or toenail removal or repair, and reduction of fractured or dislocated fingers or toes.87 Use of topical anesthesia before instrumentation can quell anxiety about the procedure and minimize pain. Assess distal capillary refill and two-point discrimination (normal <6 mm) on the volar pad before application of the block. For digital blocks, there is less pain with injection using lidocaine 1% with epinephrine compared to bupivacaine 0.5%, but the duration of anesthesia is only about half as long.88
Patient Positioning and Anatomy The hand and wrist are placed in a prone (palm down) position. The common digital nerves are derived from the median and ulnar nerves. In the distal palm, the common digital nerve divides into paired palmar branches that travel on both sides of the flexor tendon sheath and innervate the lateral and palmar aspect of each digit. The dorsal digital nerves are smaller, derived from the radial and ulnar nerves, and travel on the dorsal lateral aspect of each finger to provide sensation to the back of the finger.
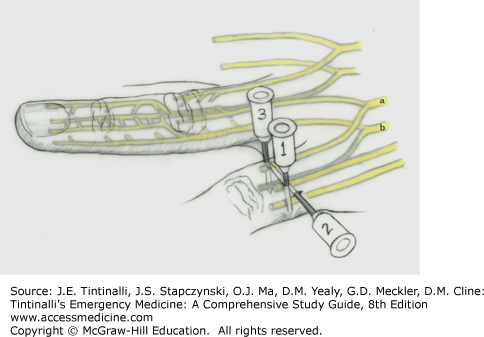
Technique Insert the needle on the dorsal surface of the proximal phalanx, advance toward the volar surface staying tangential to the phalanx, aspirate to ensure no inadvertent vascular puncture has occurred, deposit 1 mL of anesthetic solution, and inject an additional 1 mL while withdrawing the needle back to the skin surface (Figure 36-2). Reinsert the needle in the same location, but direct it across the dorsum of the digit to the other side, and inject a 1-mL band of anesthetic solution into the subcutaneous space across the dorsum of the digit. Repeat the initial injection process on the other side of the digit.
FIGURE 36-2.
Digital nerve block. Anesthetic placed as shown blocks both the dorsal (a) and palmar (b) digital nerves, ensuring circumferential anesthesia of the finger. By using the sequence shown, the prior injection provides relief from the injection to follow. See Digital Nerve Block section for further details. [Illustration used with permission of Timothy Sweeney, MD.]
Purpose A transthecal or flexor tendon sheath digital nerve block provides anesthesia to the entire digit by utilizing the flexor tendon sheath to apply anesthetic to the digital nerves.89 This procedure can be performed in addition or as an alternative to a digital nerve block. However, flexor tendon sheath block may not fully anesthetize the distal fingertip.
Patient Positioning and Anatomy The hand and wrist are placed in a supine (palm up) position. The flexor tendon sheath surrounds the flexor tendon on the palmar side of the digit.
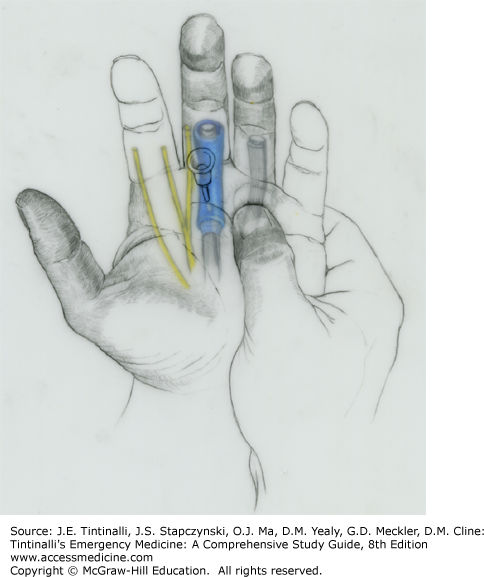
Technique Identify the distal palmar crease on the palmar aspect of the hand. Have the patient flex the finger against resistance to improve visualization of the flexor tendon. Identify the distal palmar crease of the digit to be blocked, and insert the needle at a 45-degree angle to the palmar plane with the tip pointed distally (Figure 36-3). Advance the needle until a “pop” is felt, indicating penetration of the flexor tendon sheath. Inject 2 to 3 mL of anesthetic solution. If bone is struck before the “pop” is felt, withdraw the needle 2 to 3 mm and inject the solution.
FIGURE 36-3.
Transthecal (flexor tendon sheath) digital nerve block. The point of injection is in the middle of the flexor tendon sheath at the level of the distal palmar crease. A 25-gauge needle is advanced at 45 degrees, with tip directed distally until it enters the flexor tendon sheath (shown in blue) or until bone is encountered. When the needle is properly placed within the flexor tendon sheath, the anesthetic solution is injected. Diffusion out of the tendon sheath blocks adjacent palmar digital nerves. See Transthecal or Flexor Tendon Sheath Digital Nerve Block section for further details. [Illustration used with permission of Timothy Sweeney, MD.]
A modification of the transthecal approach is to inject into the flexor tendon sheath at the base of the digit in the metacarpal crease90,91 or into the midportion of the proximal phalanx.92
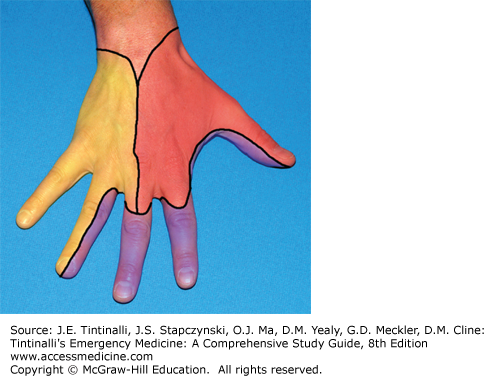
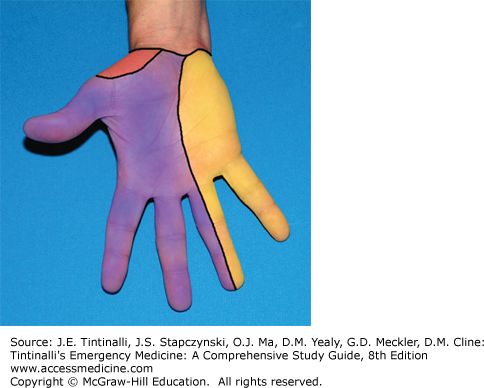
The median, radial, and ulnar nerves supply the sensory innervation to the hand and can be used in part or in combination to provide anesthesia for lacerations, puncture wounds, or fracture/dislocation reductions (Figures 36-4 and 36-5).
Purpose A median nerve block provides anesthesia to the thumb, index, long, and half of the ring finger distal to the proximal interphalangeal joint, but not the dorsum of the thumb (Figures 36-4 and 36-5).
Patient Positioning and Anatomy The hand and wrist are placed in a supine (palm up) position. The median nerve traverses between the flexor carpi radialis and the palmaris longus tendon at the proximal wrist crease. With the hand and wrist in a supine position, the flexor carpi radialis is lateral (radial direction) and the palmaris longus is medial (ulnar direction) to the nerve. When the patient makes a fist and flexes the wrist, the palmaris longus tendon is usually the more prominent of the two tendons (Figure 36-6, top left).
FIGURE 36-6.
Median and radial nerve block. Top left: Technique for identification of the palmaris longus tendon (p.l.) through wrist flexion using finger and thumb opposition. Right: The median nerve (m.) is blocked by inserting the needle between the palmaris longus and flexor carpi radialis (f.c.r.) tendons. The radial nerve (r.) block begins with an injection over the lateral aspect of the radial styloid. Lower left:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree