(1)
Chennai Breast Centre, Chennai, India
Mastitis is inflammation of the breast. Lactation-associated infections are the commonest infections in the breast. A cracked nipple allows the normal skin bacteria, usually staph aureus, to ascend into the ducts and the lobule. Poorly draining ducts or blind-ending ducts result in engorgement and collection of milk. This collection can get infected and cause mastitis and with progressive tissue necrosis can result in breast abscess. It occurs normally within 6–8 weeks following delivery. Patients often present with pain, swelling, and redness along with fever and chills. There may be a tender, palpable lump with stretched, discolored, shiny skin. The abscess starts to point and with skin necrosis the pus is discharged. Staph aureus is the commonest organism. Occasionally, methicillin-resistant staphylococcus may be the cause for the infection.
The infection is usually peripheral or central, and may initially involve only one lobar segment. As the infection progresses, the entire breast may get involved. The peripheral infections are usually unilocular and with a well-defined abscess cavity in contrast to the central ones where there might be infection spreading to multiple ducts and therefore multiple collections.
Mammography and breast MRI are not indicated. Breast ultrasound is more effective in the diagnosis of breast abscess and is useful to guide aspirations and for follow-up.
Ultrasound Findings
Edema may be the only feature, early in the course of infection. Mastitis appears as an ill-defined area of altered echotexture. The skin and subcutaneous tissue becomes thickened and the fat lobules appear echogenic due to edema. The glandular tissue becomes thickened and edematous with loss of normal tissue planes and sometimes shows hypoechoic areas. The edema is usually restricted to the affected lobe in the early stage. If untreated at this stage, it may progress to involve the entire breast. Inflammatory reactive axillary lymph nodes may also be seen (Fig. 21.1).
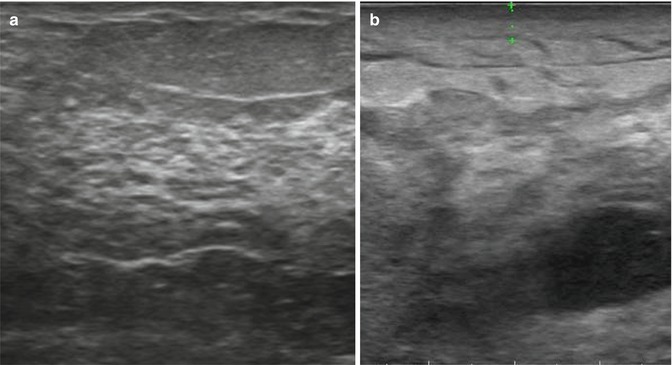
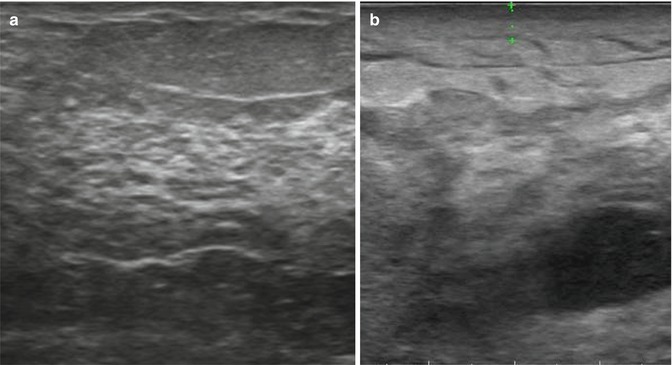
Fig. 21.1
The ultrasound image on the left (a) shows normal glandular pattern with the normal-appearing fat and skin. The image on the right (b) shows skin thickening (shown in calipers), and fat appears echogenic with loss of normal glandular architecture. Small pocket of fluid collection is noted deep in the parenchyma
Early recognition and administration of antibiotics before tissue necrosis occur, usually arrests progress. Persistent infection progresses to abscess formation. On ultrasound, abscess cavity appears as ill-defined hypoechoic collection, which can sometimes be multiloculated. The wall of the abscess cavity is often thick, irregular, and echogenic with increased vascular flow. Acoustic enhancement is present due to fluid content (Fig. 21.2a–c).
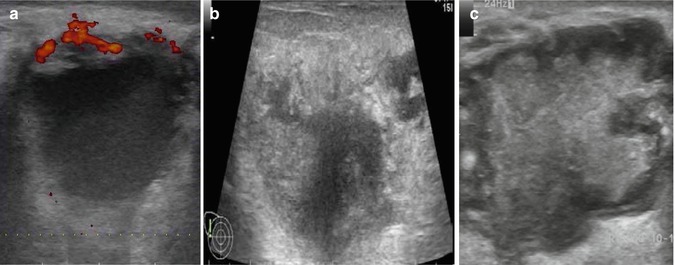
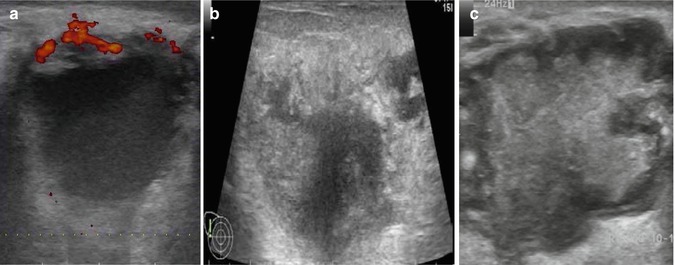
Fig. 21.2
(a–c) Ultrasound image showing ill-defined hypoechoic fluid collection
Flucloxacillin or Augmentin is usually the antibiotic of choice. In patients with penicillin sensitivity, Erythromycin or Clarithromycin can be given. MRSA infections will require linezolid or vancomycin.
Once abscess formation has occurred, pus should be removed. Traditionally, incision and drainage has been done under general anesthesia to remove the pus, but this leaves an open wound which requires dressings for a very prolonged period. Besides, it may also result in a puckered scar. For pointing abscesses, a mini incision and drainage can be done after application of local anesthetic cream in the most fluctuant area.
Majority of lactation-associated breast abscesses can be drained by ultrasound-guided aspiration and this is the preferred method of treatment. After injecting local anesthetic, using a large bore needle (16 or 18 G needle) pus can be aspirated. Repeated aspirations can be done until the infection resolves (Fig. 21.3).
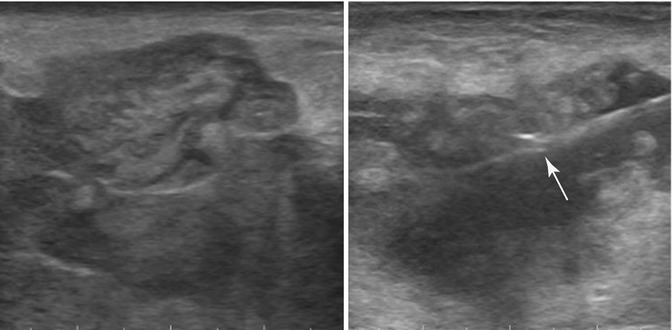
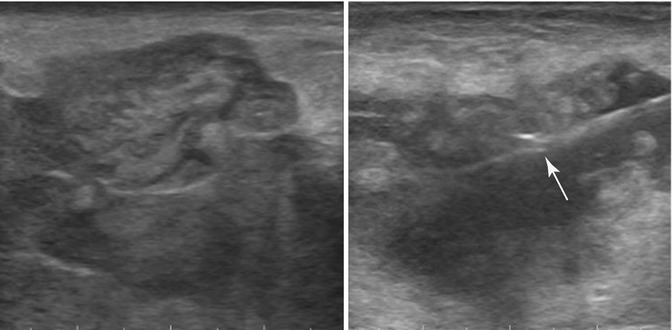
Fig. 21.3
Lactating breast abscess: ultrasound image showing mixed echogenic fluid collection with ill-defined margins in a woman who is lactating. The image on the right shows fluid being aspirated. Needle is seen within the abscess cavity (arrow)
Pus should be sent for culture and sensitivity, and appropriate antibiotics should be administered. Flucloxacillin and Amoxicillin with clavulanic acid combination are safe for administration during lactation. It is usually possible to continue breast-feeding in localized peripheral abscesses, but in more central location close to the nipple areolar complex, it may not be possible to breast-feed. Suppression of breast-feeding with Cabogolin 0.5 mg twice a day for 2 days may be considered.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







