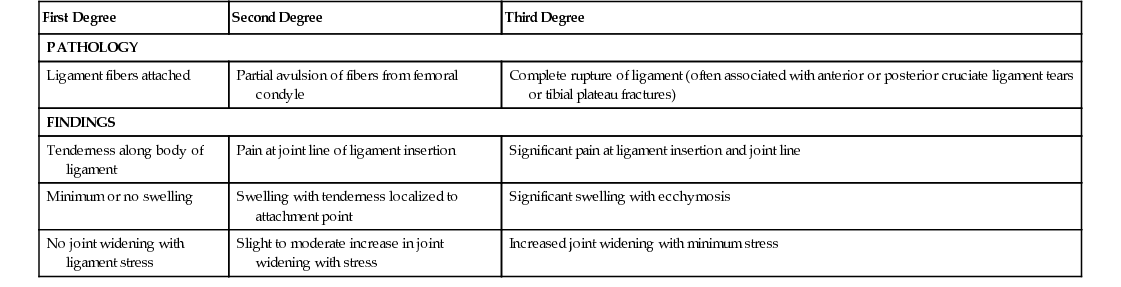
Wendy L. Halm Knee pain is a common problem that can originate in any of the bony structures of the knee joint (femur, tibia, fibula), the kneecap (patella), or the ligaments and cartilage (meniscus) of the knee. In addition, soft tissue structure surrounding the knee joint (muscle, tendons, bursae) surrounding the knee can also be a source of pain. Knee pain can affect people of all ages and can be attributed many causes. The multiple structures within the knee make it vulnerable to various types of injuries and degenerative change. Many injuries can be treated conservatively; others require surgery. There also are many extra-articular structures that can become inflamed or injured, causing knee pain. Knee pain is often classified according to cause and longevity of symptoms. Knee pain can also be a result of an acute injury, trauma, or a particular athletic move. Knee pain related to chronic and or inflammatory disease, such as bursitis, osteoarthritis, rheumatoid arthritis, or gout, is discussed in other chapters. The knee is a modified hinge joint that flexes and extends and has some rotational mobility. The knee joint contains three bones, three articulations, five major tendons, four major ligaments, two menisci, and 12 bursae. The lateral and medial articulations are between the femoral and tibial condyles. The intermediate articulation is between the patella and the femur. A relatively weak joint, the knee gains its strength from the strong ligaments that attach the femur to the tibia. Five intrinsic ligaments assist in strengthening the articular capsule. The cruciate ligaments connect the femur and tibia within the articular capsule, crossing each other in the form of an X.1 As a major weight-bearing joint, the knee is susceptible to many injuries. Torsion is limited in the joint, and any motion that extends beyond the defined range results in a ligamentous injury. Because the knee depends on the integrity of the ligaments to provide its stability, a knee injury can be a calamitous event. The approach to knee pain begins with a careful history and review of symptoms, focusing particularly on the presence of trauma, mechanism of injury, and limitations. Patients with any penetrating injury, especially if there is joint involvement, should be referred to the emergency department. Patients with a history of a traumatic event with presence of effusion or swelling, fever or other systemic illness, erythematous and swollen knees, knee pain in conjunction with sexually transmitted infections, or cellulitis over or adjacent to the affected knee or who have a history of bleeding disorders or anticoagulation are particularly concerning and should be managed with same-day orthopedic consultation.2 Physical examination of the knee can be frustrating to novice providers and requires both practice and patience. Ideally, the provider’s physical examination skills are honed under the guidance and critique of an experienced colleague. A systematic approach that includes elements of inspection, range of motion, palpation, sensation, and special tests to evaluate stability is critical to correct diagnosis of knee pain.2,3 There are two collateral ligaments: the medial collateral ligament (MCL) and the lateral collateral ligament (LCL). The MCL attaches to the medial condyle of the femur and the tibia. The LCL attaches to the lateral femoral condyle and extends to the lateral tibial plateau.2 The purpose of the collateral ligaments is to provide support to the inner and the lateral portions of the knee. The MCL and the LCL are injured when valgus or varus stress to the joint extends beyond the normal range of motion. MCL injuries are more common in athletic males and often include an injury to the medial meniscus.4 Football players and skiers are more prone to ligamentous injuries, but they can occur just as easily on the dance floor or in the bathroom. An external rotational wrenching motion of the knee or a blow to the lateral side of the knee with a firmly planted foot causes injury to the MCL. LCL injuries occur with an internal rotation or a blow to the medial side of the knee with a firmly planted foot.2,5 The injuries are graded as first-, second-, or third-degree sprains (Table 180-1). Patients with an MCL injury will typically have medial knee pain. Swelling and instability are uncommon and may signify more serious injury, such as a tear of the medial meniscus. LCL injuries manifest with acute lateral knee pain and may have associated instability and peroneal nerve palsy (commonly manifesting as a drop foot).2 An examination immediately after the injury is more accurate and helps ascertain the severity of the injury.2 Examination of the knee is more difficult in the presence of edema and muscle spasm. The examination should include observation; palpation; assessment of range of motion, motor strength, sensation, and vascular structures; ligamentous testing and stability assessment; and provocative maneuvers. The normal knee should be tested first to establish a baseline. Both knees should be observed for swelling, deformity, muscle atrophy, and patella placement. Fluctuance should be determined with the patient first standing and then supine. Tenderness and bone landmarks should be ascertained as well. In the suspected collateral ligament sprain, there is tenderness along the body of the ligament, and point tenderness at the attachment site is commonly present. With MCL injury, there may be tenderness at the medial joint line because the MCL attaches to the medial meniscus. Pain at the lateral joint line can be indicative of an internal joint injury. Valgus stress on the knee joint determines MCL laxity (Fig. 180-1). If the clinician identifies significant valgus laxity with the knee in full extension, an injury involving the entire MCL complex or the anterior cruciate ligament (ACL) should be suspected.5 Varus stress on the knee joint determines LCL laxity (see Fig. 180-1). Laxity at 30 degrees of flexion indicates injury to the LCL.2 Active range of motion in extension and flexion should be assessed. If active range of motion is not possible, passive extension and flexion should be determined. Initial diagnostics should include plain radiographs to exclude fractures and dislocations. More extensive radiologic examinations, such as magnetic resonance imaging (MRI), should be considered in consultation with an orthopedist. As with any joint injury, a fracture or dislocation must be considered. In the knee, injury to the ACL, posterior cruciate ligament (PCL), or articular cartilage or patellar dislocation should be considered. Conservative treatment of isolated first- and second-degree sprains is recommended.4 If the knee is unstable on examination, an MCL-stabilizing brace is worn at all times. Pain and inflammation can be treated with nonsteroidal anti-inflammatory drugs (NSAIDs) or acetaminophen. The patient should avoid bearing weight on the affected knee. Simple straight leg raises and quadriceps-tightening exercises as well as simple hamstring-strengthening exercises can be done easily right in the brace. Once pain and swelling have subsided, the patient should be referred to physical therapy for more progressive rehabilitation.5 Adjunctive therapy may include ultrasound or electrical muscle stimulation.5 Surgical repair may be indicated for certain grade III injuries.4,5 When considering medication treatment for the older adult, clinicians should consider potentially inappropriate medications. The use of NSAIDs in the older adult has been associated with increased risk of gastrointestinal (GI) bleeding and peptic ulcer disease in high-risk groups, including those older than 75 years, or in patients who are taking oral or parenteral corticosteroids, anticoagulants, or antiplatelet agents.6 Without accurate diagnosis and treatment, the injury can extend, jeopardizing the joint’s stability and other structures. The incompletely rehabilitated knee will be weak and potentially unstable. Traumatic arthritis can be a sequela of any joint injury. Explanation of the importance of adherence to the rehabilitative process is imperative. In some instances, a knee support for sports is necessary. Pain and swelling are indicators that the knee is being overstressed or has been reinjured. Resembling an X, the cruciate ligaments crisscross within the joint capsule but are extrasynovial. There are two cruciate ligaments: the ACL and the PCL. The ACL attaches to the anterior part of the intercondylar area of the tibia, posterior to the medial meniscus, and rises superiorly, posteriorly, and laterally to attach to the posterior section of the medial side of the lateral condyle of the femur.1 The ACL restrains the anterior to posterior alignment of the knee, keeping the proper relationship of the femur to the tibia. It is loose with the knee in flexion and tight when the knee is fully extended. It is the weaker of the two cruciate ligaments. The PCL originates at the posterior part of the intercondylar area of the tibia. It crosses superiorly and anteriorly on the medial side of the ACL and attaches to the anterior part of the lateral surface of the medial femoral condyle. The PCL is tight with the knee in flexion. The PCL restrains the posterior to anterior alignment of the knee. A cruciate ligament injury can be a sprain, a partial tear, or a complete disruption of the ligament. Physical examination and radiologic tests as indicated are used to determine the degree of the injury. The ACL is the most commonly involved structure in severe knee injuries. Female gender and intensity of play increase the risk of ACL tear.7 The PCL is less often injured. The PCL is the stronger ligament and is usually injured through trauma to the anterior surface of the proximal tibia (as in hitting the dashboard) or falling onto the tibial tubercle with the knee flexed.2,4 The ACL is typically injured in sports during rapid deceleration or on quickly changing directions. The ACL can also be torn with a direct blow to the lateral portion of the knee.7 The ACL injury often occurs in combination with ruptures of the MCL and the medial meniscus. Once the ligament is torn, the knee is unstable. Swelling occurs rapidly in an ACL or PCL injury because of bleeding from the ligament tear.7
Knee Pain
Definition and Epidemiology
Knee Pain
Collateral Ligament Sprains
Pathophysiology
Clinical Presentation
Physical Examination
Diagnostics
Differential Diagnosis
Management
![]() Orthopedic physician consultation is indicated for chronic MCL tears, acute MCL tears with other ligamentous injuries, and LCL or posterolateral corner injuries.
Orthopedic physician consultation is indicated for chronic MCL tears, acute MCL tears with other ligamentous injuries, and LCL or posterolateral corner injuries.
![]() Immediate emergency department referral is indicated for severe sprains, tears, or suspected fractures.
Immediate emergency department referral is indicated for severe sprains, tears, or suspected fractures.
Life Span Considerations
Complications
Patient and Family Education
Cruciate Ligament Injuries
Definition and Epidemiology
Pathophysiology
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Knee Pain
Chapter 180