Knee Injuries
Christine B. Irish and Christopher T. Bowe
Knee trauma accounts for more than one million emergency department (ED) visits each year (1). The knee joint is made up of bones, ligaments, muscles, and cartilage (Fig. 44.1). The three bones that make up the knee are the distal femur, patella, and proximal tibia. The femoral condyles articulate with the proximal tibia (tibial plateau) to form the weight-bearing portion of the knee joint. The patella does not function in weight bearing, but rather provides protection to the distal femur, in addition to improving stability and strength of the extensor mechanism.
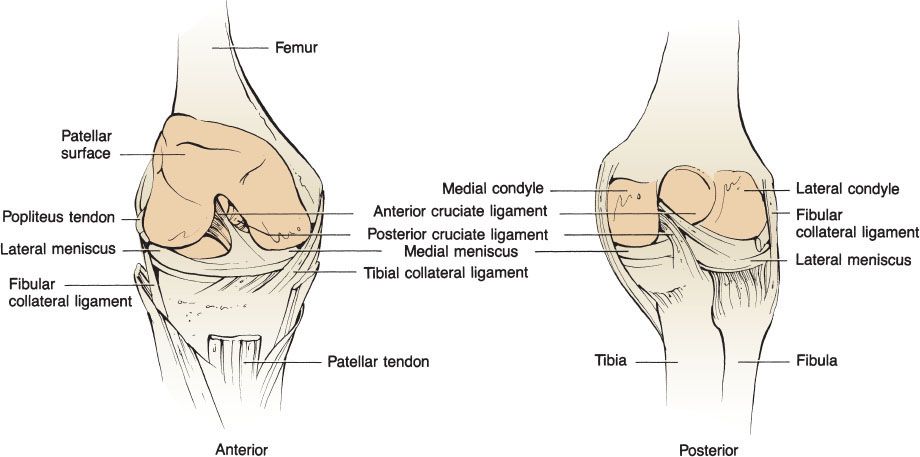
FIGURE 44.1 Anatomy of the knee.
The knee relies on four major ligaments: the medial collateral ligament (MCL), the lateral collateral ligament (LCL), the anterior cruciate ligament (ACL), and the posterior cruciate ligament (PCL) for stability and proper function (2). The MCL provides most of the resistance to valgus stress, while the LCL protects from varus stress. The cruciate ligaments are located within the intercondylar notch. The ACL prevents anterior displacement of the tibia relative to the femur while the PCL prevents posterior displacement (2). The anatomy of the posterior lateral corner of the knee is complex; its major structures consist of the LCL, the arcuate complex, the popliteal tendon, and the popliteal-fibular ligament (3). The posterolateral corner primarily resists posterior lateral rotation of the tibia relative to the femur but also contributes to resisting posterior tibial translation. The posteromedial corner of the knee consists primarily of the posterior oblique portion of the MCL and the associated joint capsule. These structures provide resistance to valgus stress and posterior medial tibial translation. The menisci are cartilage positioned on the articulating surface of the tibia. The menisci function to provide a contact surface between the tibia and femur and distribute and dissipate forces within the knee (4).
The muscles involved with normal knee function are divided into extensors and flexors. Extension is primarily provided by the quadriceps muscles, composed of the vastus medialis, vastus intermedius, vastus lateralis, and rectus femoris. The tendons of these muscles combine to form the quadriceps tendon, which inserts into the superior patella and the medial and lateral retinaculum of the joint capsule. This tendon then becomes the patellar tendon, which connects to the tibial tubercle (5). The primary flexors of the knee are the hamstring muscles, consisting of the semimembranosus, semitendinosus, and the two heads of the biceps femoris of the posterior thigh.
The major vascular structures around the knee are located posteriorly. The popliteal artery is fixed proximally. This tethering makes the popliteal artery susceptible to injury by traction forces, as seen with dislocations. The popliteal artery is also at risk of disruption by fractures or penetrating wounds (6). There is limited collateral circulation, so damage to the popliteal artery places the viability of the lower limb in jeopardy. The sciatic nerve separates into the tibial and peroneal nerves proximal to the knee. The tibial nerve passes posteriorly and is therefore susceptible to the same mechanisms of injury as the popliteal artery, while the peroneal nerve courses superficially around the lateral aspect of the knee to the proximal fibula (6).
CLINICAL PRESENTATION
Fractures
Distal femoral fractures are typically described relative to the femoral condyles and are separated into supracondylar or intercondylar (eFig. 44.1) (7). The proximity of the femoral artery and peroneal nerves to the bone requires that the neurovascular status of the extremity be evaluated and documented in the setting of a fracture.
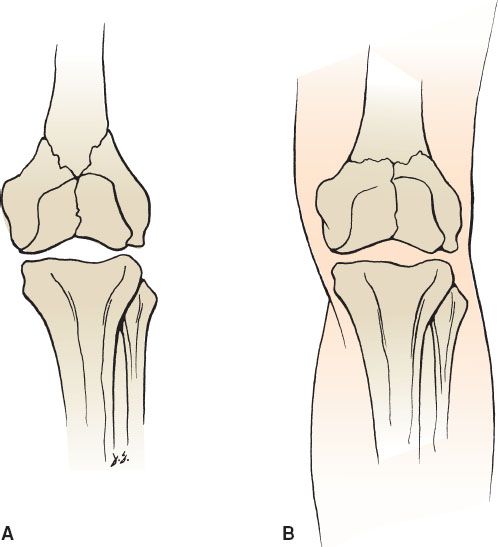
eFIGURE 44.1 Distal femur fractures. A: Y-shaped intercondylar and B: T-shaped intercondylar.
Tibial plateau fractures occur as a result of varus–valgus forces, axial loads, or both. Fractures of the tibial plateau may cause a major impairment in stability and function of the knee (8). The potential for neurovascular injuries is much higher in patients with proximal tibial fractures than in distal femoral fractures. The potential for the development of a compartment syndrome is also significant. Paresthesias and paralysis from compartment syndromes may be mistaken for a primary nerve injury. Injuries to the menisci, as well as to the collateral and cruciate ligaments, should be suspected as well.
A fracture of the tibial tuberosity often represents an avulsion injury caused by the patellar tendon. This is an uncommon fracture. It occurs with either strong flexion or extension against resistance. Fractures of the tibial tuberosity most commonly occur before closure of the epiphysis. The differential diagnosis of pain over the tibial tuberosity should also include Osgood–Schlatter disease, which is a traction injury to the apophysis of the tibial tuberosity. Although it is most common in boys aged 10 to 13 years, it may be seen in girls, usually aged 8 to 13 years. It is thought that repetitive trauma to the epiphysis results in incomplete separation of parts of the cartilaginous and osseous portions of the tibial tuberosity. Diagnosis is based on the history and physical examination. The tubercle is painful, tender, and usually enlarged. Pain is exacerbated by extension of the knee, particularly against resistance.
Patellar fractures result most commonly from direct forces. Less common are fractures resulting from severe tension placed on the patella by strong contraction of the quadriceps; the usual result is a transverse fracture, which may disrupt the extensor mechanism (5).
Knee Dislocation
Knee dislocations are orthopedic emergencies and require immediate attention. Knee dislocations are generally associated with high-energy trauma. The dislocation is described as anterior, posterior, medial, lateral, or rotary based on the position of the tibia relative to the femur. For a dislocation to occur, significant trauma to the surrounding soft tissue is generally seen, including the collateral ligaments, cruciate ligaments, menisci, joint capsule, and neurovascular structures. Physical examination may be difficult, and a dislocation may spontaneously reduce before the patient arrives at the ED. The patient may describe a history of abnormal position of the joint before reduction. Because of the concern for peroneal nerve and popliteal artery injury, specific attention should be devoted to this aspect of the physical examination. The absence of distal pulses is highly correlated with significant vascular injury; the presence of pulses, however, does not eliminate the possibility of vascular damage (9). Considering the significant mechanisms of injury and the potential for vascular damage, compartment syndrome is also a potential complication.
Patellar Dislocation
The patella may be completely dislocated or subluxed from the intercondylar groove as a result of a direct blow or by hyperflexion of the knee joint. The patella almost always displaces laterally. Diagnosis is usually made by careful physical examination. If the patella has spontaneously reduced, plain films will confirm proper placement and identify any bony injury (9).
Ligamentous Injuries
LCL injuries are more commonly seen after falls and motor vehicle collisions (MVCs). MCL and LCL tears are associated with cruciate ligament injuries, with the LCL injury less likely to occur as an isolated event (2). The patient generally presents with tenderness along the distribution of the ligament. There may be a history of “popping” and abnormal bending of the knee. The physical examination should include the diagnostic tests discussed below, with varus and valgus forces applied to the knee at extension and 30 degrees of flexion.
Injuries to the cruciate ligaments are common with low-velocity trauma as well as with high-energy forces. The ACL is weaker than the PCL and is more commonly injured. Tests for ACL injuries include the Lachman, anterior drawer, and pivot shift tests. The Lachman test is the most sensitive. PCL stability is evaluated by the posterior drawer and posterior sag tests (2).
Meniscal Tears
Meniscal injuries generally occur with a twisting force applied to the knee. Patients frequently complain of hearing a “pop,” which is common but not specific to meniscal injuries. Often, the patient reports locking of the knee, usually a result of a “bucket-handle” tear, with a free central portion of the cartilage becoming lodged in the intercondylar notch. The medial meniscus is most commonly affected. The patient usually presents with a joint effusion.
Tendon Injuries
The extensor mechanism includes the quadriceps tendon, the patella, and the patellar tendon. Injuries to these structures, or avulsion of the tibial tubercle, can disrupt the extension of the knee. Disruption may result from high-energy or penetrating trauma but is also seen with low-energy forces (9). The quadriceps tendon is more commonly ruptured and usually ruptures just proximal to the patella (10). The patellar tendon frequently ruptures at the insertion into the patella. The physical examination generally reveals a swollen, tender knee, and a palpable deficit may be present. Tenderness is usually identified at the site of injury. To evaluate the tendons properly, the patient’s ability to extend the knee fully against resistance must be tested. The diagnosis is usually suspected clinically. Partial injuries may be difficult, if not impossible, to detect in the ED.
DIFFERENTIAL DIAGNOSIS
Common important bony injuries to the knee include fractures, dislocations, and subluxations. Of further concern are tendon and cartilage injuries, as well as injury to the vasculature and nerves surrounding the knee.
ED EVALUATION
The history is extremely useful in guiding the evaluation of the injured knee. The chief complaint, mechanism of injury, and the exact nature and timing of symptoms will help to differentiate acute trauma from chronic injuries. The traumatic mechanism should be fully explored, as well as the position of the knee at the time of injury. The history should also assess for additional injuries, particularly to the hip and ankle.
The physical examination begins with visual inspection of the knee, followed by the remainder of the lower extremity. The examiner should note any obvious deformity, ecchymosis, erythema, edema, or cutaneous lesions. Often, comparison with the uninjured knee will be helpful in assessing for joint effusion and local edema. Following gross inspection, palpation will elicit specific areas of tenderness, crepitus, abnormal skin temperature, or the presence of an effusion. Finally, the examiner should assess active and passive range of motion, alignment, and neurovascular status (2). The comprehensive examination will include evaluation of the knee in the standing, sitting, and supine positions, when not limited by pain or swelling.
After completion of a thorough physical examination, appropriate radiographic studies may be ordered when clinically indicated. Several clinical decision rules regarding the use of radiographs in the acutely injured knee have been proposed (Table 44.1). Prospective validation has shown excellent sensitivity of these rules (1). Adherence to these clinical decision rules can substantially reduce the incidence of unnecessary radiographs (11). Standard imaging includes the anteroposterior and lateral views and can be supplemented with sunrise (skyline) and tunnel views to evaluate the patellofemoral joint and intercondylar notch.
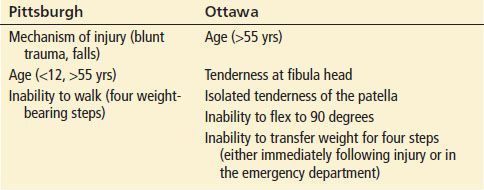
TABLE 44.1
Decision Rules for the Use of Radiographs in the Acutely Injured Knee