ANATOMY
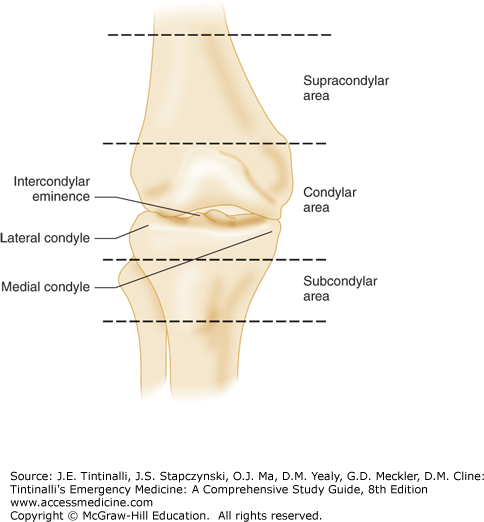
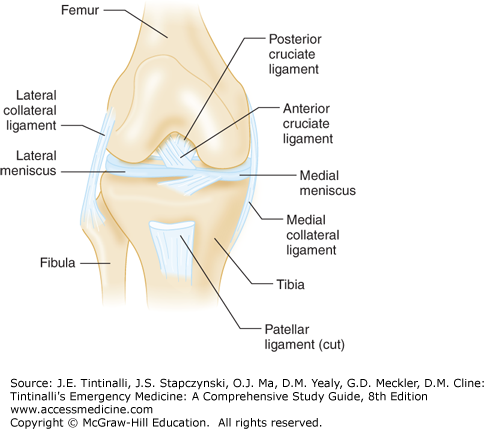
The knee consists of two joints, the tibiofemoral joint and the patellofemoral joint. Within the tibiofemoral joint, the distal femur (comprised of the medial and lateral femoral condyles) articulates with the proximal tibia (comprised of the medial and lateral tibial condyles) (Figure 274-1). The medial and lateral menisci are situated between the articular surfaces, and the menisci provide cushion, lubrication, and resistance to articular wear (Figure 274-2). In the patellofemoral joint, the patella articulates with the distal femur along the anterior depression called the patellofemoral groove during flexion and extension of the knee. The patella is stabilized by the patellar tendon and medial retinaculum.
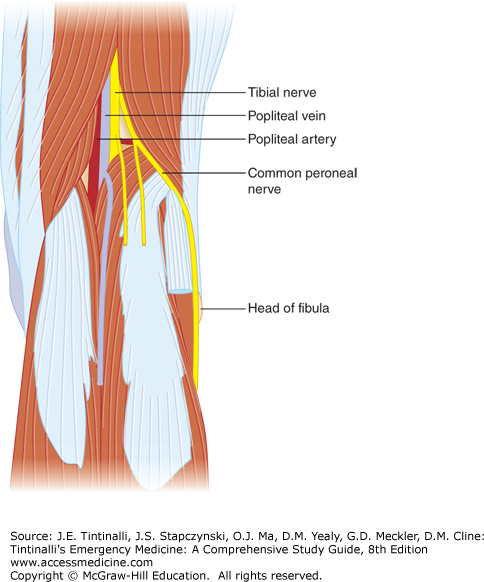
There are four ligaments in the knee: the anterior cruciate ligament, the posterior cruciate ligament, and the medial and lateral collateral ligaments (Figure 274-2). These ligaments provide strength and stability to the knee. The posterior aspect of the knee, the popliteal fossa, contains the popliteal artery and vein, the common peroneal nerve, and the tibial nerve (Figure 274-3).
CLINICAL FEATURES
Determine the mechanism of knee injury and review all prior orthopedic injuries or surgical procedures. As with all orthopedic examinations, compare the noninjured or normal joint with the injured joint during all aspects of the examination, but especially during palpation and stress testing.
The first examination is usually the easiest to perform and may be the most valid, because the patient does not anticipate pain and may not guard against the examination, and because inflammation and effusion limiting the examination may have not yet developed.
Assess gait (if possible), functional range of motion, and the ability to perform a straight leg raise (evaluates the extensor complex). Evaluate the knee for ecchymoses, swelling, effusion, masses, patella location and size, muscle mass, erythema, and evidence of local trauma. With the patient supine, determine whether leg lengths are equal or unequal. Ask the patient to demonstrate the best possible active range of motion. Assess distal neurovascular function. Palpate the nontender areas first and work toward the tender area to minimize patient apprehension. Palpate the patella, patellar facets, proximal fibula, and femoral and tibial condyles for pain and crepitus. Make note of joint effusion, tenderness, increased temperature, strength, sensation, and location of pulses.
Examine the patella for size, shape, and location with the knee in flexion. Check patellar mobility with the knee in extension, making sure it can move laterally and medially without apprehension. Palpate the popliteal space for masses, swelling, and pulses. With the knee in flexion, palpate both the medial and lateral joint lines and the medial and lateral collateral ligaments, because tenderness at those locations suggests the possibility of a meniscal or ligamentous injury, respectively. The final phase of the examination of the knee is stress testing (see “Ligamentous and Meniscal Injuries” below). This is the most difficult aspect of the examination, although potentially the most informative. The patient must be relaxed and made as comfortable as possible. Testing is often easier if the patient sits up with the leg hanging over the side of the bed and with the bed supporting the posterior thigh. Examine the uninjured, presumably normal, opposite knee first to determine the patient’s normal laxity.
Popliteal artery injury can occur from fractures about the knee, especially femoral condyle fractures or displaced tibial plateau fractures, and from ligamentous injuries such as isolated posterior cruciate ligament injuries, multiple ligamentous injuries, or knee dislocation.1,2 Popliteal artery circulation must be restored within 8 hours to avoid amputation, because collateral circulation is insufficient to maintain blood flow to the leg. Measure distal pulses on ED admission and after any manipulation, and compare pulses to those in the noninjured leg. A diminished pulse raises concern for vascular injury and should not be interpreted as vascular spasm. An abnormal finding on pulse examination is reported to have a sensitivity of only 79% and a specificity of 91% for arterial injuries that require surgical intervention,2 so it is important to remember that vascular injury can be present even in the presence of normal pulses. Ancillary studies include measurement of ankle-brachial index (<0.9 in a patient with peripheral vascular disease or vascular injury) and duplex US (reported to be 95% sensitive and 99% specific for arterial injury).1 Vascular surgery consultation is required for any potential popliteal arterial injury to determine the need for angiography, as well to monitor for the development of compartment syndrome, venous injury, and arterial thrombosis.
Peroneal nerve injuries can result from severe ligamentous knee injuries and knee dislocations. Nearly half of fibular head fractures or avulsions are associated with peroneal nerve injury. The deep peroneal nerve provides sensation to the first dorsal web space of the toes and allows dorsiflexion of the foot and extension of the toes. Injury results in foot drop and gait difficulty. Prognosis is variable, depending on the severity of injury.
DIAGNOSIS
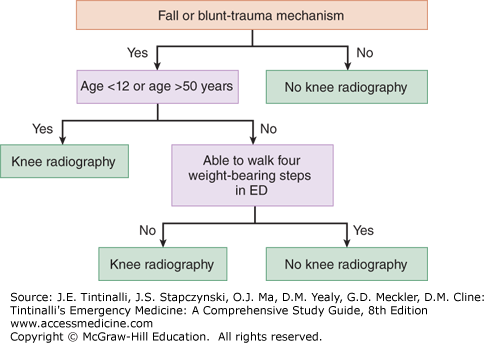
The Ottawa Knee Rules (Table 274-1) are sensitive in identifying fracture, and their use reduces ED waiting times and costs. The Pittsburgh Knee Rules (Figure 274-4) are similar and may have greater specificity.3,4
Patient age >55 y (rules have been validated for children 2–16 y of age) Tenderness at the head of the fibula Isolated tenderness of the patella Inability to flex knee to 90 degrees Inability to transfer weight for four steps both immediately after the injury and in the ED |
Both rules are applicable to children >2 years old and adults.4 It would be reasonable to order radiographs on a higher number of patients with knee pain who are multisystem trauma patients, and thus immobilized and unable to undergo gait testing.
Anteroposterior and lateral radiographs are typically obtained if radiographs are needed.5 Fat-fluid levels (lipohemarthrosis) suggest intra-articular fracture and may be identified on a lateral view of the knee.6 Consider weight-bearing radiographs when tolerated, which allows for a functional assessment. Additional radiograph views can be very useful. Oblique views are particularly helpful for detecting subtle tibial plateau fractures (internal oblique view is best for visualizing the lateral plateau, and external oblique view is best for visualizing the medial plateau).5,7 A tunnel or intercondylar view provides a clear image of the intercondylar region and is particularly useful in identifying tibial spine fractures. A sunrise (skyline, axial, or tangential) view is most useful in detecting nondisplaced vertical or marginal fractures of the patella, which may be missed with the conventional views. The sunrise view is indicated if patellar subluxation or fracture is suspected. CT may be necessary to fully delineate the extent of tibial plateau fractures. MRI is also helpful in this regard and has the added benefit of being able to assess soft tissue (i.e., ligamentous and meniscal) injury.5
SPECIFIC INJURIES
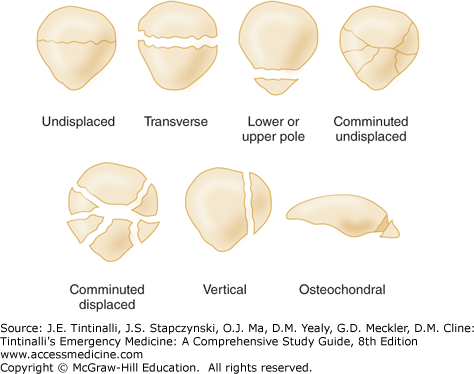
Table 274-2 reviews the mechanisms of injury and treatment of patellar fractures. Patellar fractures may be transverse, comminuted, or of the avulsion type when the quadriceps or patellar tendon pulls off a small portion of the patella (Figure 274-5).
| Fracture | Mechanism | Treatment |
|---|---|---|
| Patella | Direct blow (i.e., fall, motor vehicle crash) or forceful contraction of quadriceps muscle | Nondisplaced fracture with intact extensor mechanism: knee immobilizer, rest, ice, analgesia. Follow-up for serial radiographs. Displaced >3 mm, articular incongruity >2 mm, or with disruption of extensor mechanism: above treatment plus early referral for ORIF.8 Severely comminuted fracture: surgical debridement of small fragments and suturing of quadriceps and patellar tendons. Open fracture: irrigation and antistaphylococcal antibiotics in the ED; debridement and irrigation in the operating room. |
| Femoral condyles | Fall with axial load with valgus/varus/rotational forces, or a blow to the distal femur | Incomplete or nondisplaced fractures in any age group or stable impacted fractures in the elderly: long leg splinting and orthopedic referral. Displaced fractures or fractures with any degree of joint incongruity: splinting and orthopedic consult for ORIF.9,10 |
| Tibial spines and tuberosity | Force directed against flexed proximal tibia in an anterior or posterior direction (i.e., motor vehicle crash, sporting injury) | Incomplete or nondisplaced fractures: immobilization in full extension (knee immobilizer) and orthopedic referral in 2–7 d. Complete or displaced fracture: early orthopedic referral, often requires ORIF.11 |
| Tibial tuberosity | Sudden force to flexed knee with quadriceps contracted | Incomplete or small avulsion fracture: immobilization. Complete avulsion: ORIF.8 |
| Tibial plateau | Valgus or varus forces combined with axial load that drives the femoral condyle into the tibia (i.e., fall, leg hit by car bumper)12 | Nondisplaced, lateral fracture: knee immobilizer with non–weight bearing and orthopedic referral in 2–7 d. Depression of articular surface: early orthopedic consult for ORIF.12 |
Transverse fractures of the patella are most common, followed by stellate and comminuted fractures. Patients with nondisplaced fractures may be ambulatory. On examination, there is focal patellar tenderness, swelling, and effusion. Check the integrity of the extensor mechanism of the knee by having the patient perform a straight-leg raise against gravity. Nonoperative management is indicated for fractures with an intact extensor mechanism and <2 mm of step-off and <3 mm of fracture displacement.8,13 Transverse fractures are more likely to be displaced and to be associated with a disrupted extensor mechanism. Differential diagnosis of patellar fractures radiographically includes bipartite patella. This condition involves the superior lateral corner of the patella, is typically bilateral, and is differentiated from fracture by the smooth cortical margins.
Fractures of the femoral condyles account for 6% of femur fractures and include supracondylar, intercondylar, condylar, and distal femoral epiphyseal fractures (Figure 274-1). Table 274-2 reviews the mechanisms of injury and treatment for femoral condyle fractures. Examination reveals pain, swelling, deformity, rotation, shortening, and an inability to ambulate. Although neurovascular injuries are uncommon, the potential for popliteal artery injury exists, so the status of distal sensation and pulses must be checked. Test the space between the first and second toes, innervated by the deep peroneal nerve, for sensation. In addition, search for associated injuries, including ipsilateral hip dislocation or fractures and damage to the quadriceps apparatus. The overall outcome of these injuries is fair. Complications include deep venous, fat embolus syndrome, delayed union or malunion, and the subsequent development of osteoarthritis.9
Although isolated injuries of the tibial spine are uncommon, they usually result in cruciate ligament insufficiency. Table 274-2 reviews the mechanism of injury and treatment for tibial spine and tuberosity fractures. Fracture of the anterior tibial spine is about 10-fold more common than fracture of the posterior spine. Examination shows a painful, swollen knee secondary to hemarthrosis, inability to extend fully, and a positive finding on the Lachman test (see “Ligamentous and Meniscal Injuries” below).11 The quadriceps mechanism inserts on the tibial tubercle. A sudden force to the flexed knee with the quadriceps muscle contracted may result in a complete or incomplete avulsion of the tibial tubercle. The fracture line may extend into the joint. Examination reveals pain and tenderness over the proximal anterior tibia with pain on passive or active extension.
Fractures of the tibial plateau are seen more commonly in the older population and can be very difficult to detect. Table 274-2 reviews the mechanism of injury and treatment for tibial plateau fractures. Both medial and lateral plateaus may be fractured simultaneously, although the lateral plateau is more often fractured.12
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree