![]() Clinical suspicion of knee dislocation with neurovascular compromise (FIGURE 63.1)
Clinical suspicion of knee dislocation with neurovascular compromise (FIGURE 63.1)
![]() Radiographic evidence of knee dislocation; anterior (associated with popliteal artery traction and intimal tears) more common than posterior (associated with popliteal artery compression and transection), lateral, medial, and rotary knee dislocations
Radiographic evidence of knee dislocation; anterior (associated with popliteal artery traction and intimal tears) more common than posterior (associated with popliteal artery compression and transection), lateral, medial, and rotary knee dislocations
CONTRAINDICATIONS
![]() Multiple failed reduction attempts with adequate sedation prompts urgent orthopedic consult
Multiple failed reduction attempts with adequate sedation prompts urgent orthopedic consult
RELATIVE CONTRAINDICATIONS
![]() Dimple or pucker sign of the skin of the anteromedial knee.
Dimple or pucker sign of the skin of the anteromedial knee.

FIGURE 63.1 Clinical suspicion of knee dislocation with neurovascular compromise. (From Silverberg M. Knee dislocations. In: Greenberg MI, ed. Greenberg’s Text-Atlas of Emergency Medicine. Philadelphia, PA: Lippincott Williams & Wilkins; 2005:522, with permission).
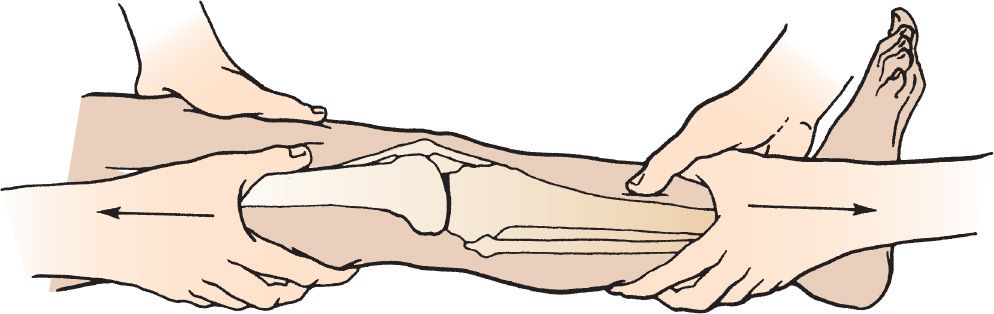
FIGURE 63.2 Gentle and persistent axial traction is applied by the second practitioner, while the first practitioner maintains countertraction. (From Irish CB, Bowe CT. Knee injuries. In: Wolfson AB, ed. Harwood-Nuss’ Clinical Practice of Emergency Medicine. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2015:289, with permission.)
RISKS/CONSENT ISSUES
![]() Knee reduction is a limb-saving procedure and as such it may be performed if informed consent cannot be obtained
Knee reduction is a limb-saving procedure and as such it may be performed if informed consent cannot be obtained
![]() Reduction attempts may result in connective tissue injury, neurovascular compromise, and iatrogenic fractures
Reduction attempts may result in connective tissue injury, neurovascular compromise, and iatrogenic fractures
![]() General Basic Steps
General Basic Steps
![]() Neurovascular examination
Neurovascular examination
![]() Analgesia
Analgesia
![]() Traction reduction
Traction reduction
![]() Confirmatory neurovascular examination
Confirmatory neurovascular examination
![]() Immobilization
Immobilization
![]() Confirmatory imaging test
Confirmatory imaging test
TECHNIQUE
![]() Neurovascular examination is critical!
Neurovascular examination is critical!
![]() Document the presence and character of tibialis posterior and dorsalis pedis pulses bilaterally
Document the presence and character of tibialis posterior and dorsalis pedis pulses bilaterally
![]() Document presence and character of popliteal pulse, bruit, thrill, and/or hematoma
Document presence and character of popliteal pulse, bruit, thrill, and/or hematoma
![]() Consider using Doppler acoustics to check pulses and ankle-brachial index (ABI). ABI is the systolic blood pressure of the injured extremity, divided by the systolic blood pressure of an uninjured upper extremity.
Consider using Doppler acoustics to check pulses and ankle-brachial index (ABI). ABI is the systolic blood pressure of the injured extremity, divided by the systolic blood pressure of an uninjured upper extremity.
![]() ABI ratio of <0.9 is concerning for arterial injury
ABI ratio of <0.9 is concerning for arterial injury
![]() Document sensorimotor function with emphasis on the condition of common peroneal and posterior tibial branches of the sciatic nerve
Document sensorimotor function with emphasis on the condition of common peroneal and posterior tibial branches of the sciatic nerve
![]() Consider additional management if neurovascular status is maintained
Consider additional management if neurovascular status is maintained
![]() Obtain anteroposterior and lateral knee x-rays
Obtain anteroposterior and lateral knee x-rays
KNEE REDUCTION
![]() An assistant stabilizes the distal femur and applies countertraction
An assistant stabilizes the distal femur and applies countertraction
![]() Practitioner applies gentle and persistent axial traction to the ankle/distal tibia (FIGURE 63.2)
Practitioner applies gentle and persistent axial traction to the ankle/distal tibia (FIGURE 63.2)
![]() If reduction is not achieved within 1 minute, apply an additional attempt while axial traction/countertraction is maintained (FIGURE 63.3)
If reduction is not achieved within 1 minute, apply an additional attempt while axial traction/countertraction is maintained (FIGURE 63.3)
![]() Anterior dislocation: A second assistant applies gentle anterior force to the distal femur
Anterior dislocation: A second assistant applies gentle anterior force to the distal femur
![]() Posterior dislocation: Operator applies gentle anterior force to the proximal tibia
Posterior dislocation: Operator applies gentle anterior force to the proximal tibia
![]() Medial, lateral, or rotatory dislocation: Operator applies gentle force to the proximal tibia in the opposite direction of the dislocation deformity
Medial, lateral, or rotatory dislocation: Operator applies gentle force to the proximal tibia in the opposite direction of the dislocation deformity
POSTREDUCTION
![]() Document a repeat neurovascular examination. Complete the examination for open injuries, associated fractures, or ligamentous laxity.
Document a repeat neurovascular examination. Complete the examination for open injuries, associated fractures, or ligamentous laxity.
![]() Immobilize the reduced knee
Immobilize the reduced knee
![]() Apply a long leg posterior splint with the knee in 15 to 20 degrees of flexion to prevent posterior subluxation of the tibia
Apply a long leg posterior splint with the knee in 15 to 20 degrees of flexion to prevent posterior subluxation of the tibia
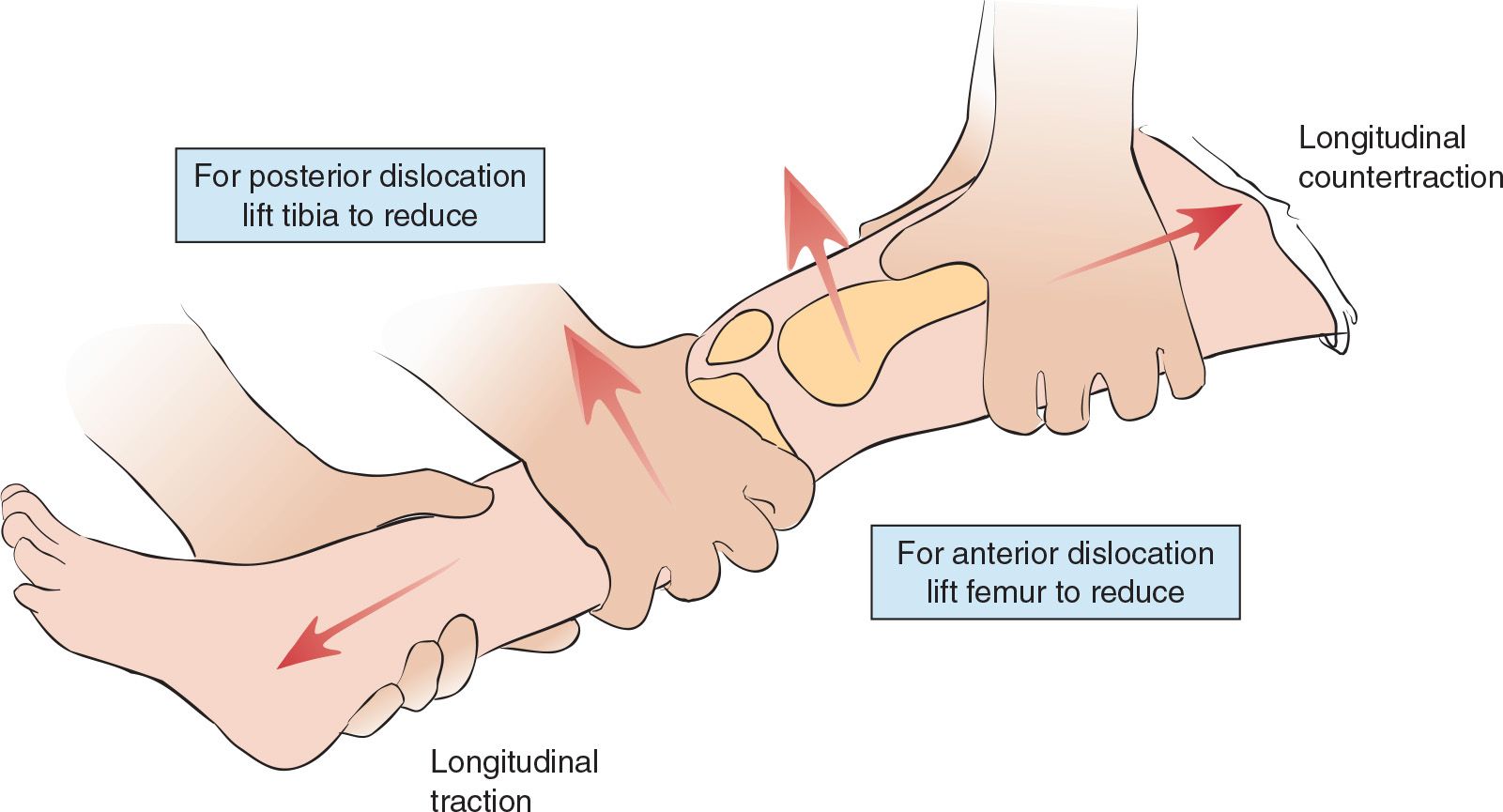
FIGURE 63.3 Technique for reduction of knee joint dislocation. (From Young GM. Reduction of common joint dislocations and subluxations. In: Henretig FM, King C, eds. Textbook of Pediatric Emergency Procedures. Philadelphia, PA: Williams & Wilkins; 1997:1098, with permission.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


