• Advance directive → instructions given by an individual specifying what should be done for his or her health should he or she no longer be able to make decisions
• Living will → addresses specific directives regarding treatment course to be taken by caregivers (may forbid certain interventions—e.g., intubation, CPR) if pt unable to give informed consent
• Health-care power of attorney → appoints an individual (a proxy) to make health-care decisions should pt become incapacitated
• Mental competency → legal term; pt’s ability to make rational informed decisions
• Adults are presumed to be competent
• Only a court can declare a person incompetent
• Physician opinion of incompetency = opinion only
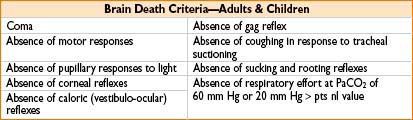
• Brain death
• Definition = permanent absence of brain & brainstem function
• Must rule out confounding factors (drug/toxins, hypothermia <32 degrees, metabolic derangements, Guillain–Barré syndrome, locked-in syndrome)
END-OF-LIFE ISSUES
• DNR/DNI is not automatically suspended during surgery
• In case of DNR/DNI, must clearly document that status & communicate with medical & nursing staff to avoid providing unwanted treatment
• Specific measures not to be performed should be clearly documented by a physician (e.g., intubation, chest compressions, defibrillation, invasive line placement, vasopressors)
• In cases of medical futility: Physician has duty to counsel medical decision maker (next of kin, legal guardian) & explain possibility of DNR/DNI status & potential for withdrawal of life-sustaining measures
• Medical decision maker should receive info about pt’s prognosis before making end-of-life decisions for the patient
PEDIATRIC/MINOR (<18 YRS) PATIENTS
• Physicians must obtain informed consent from a parent or surrogate before a child can undergo any medical intervention
• Consent for pregnancy termination procedure dependent on state laws
• Pediatric patients’ wishes should be included in decision-making process when appropriate
JEHOVAH’S WITNESSES (JW)
• JW patients usually will not accept blood or blood products (even under lifesaving circumstances)
• Obtain informed consent, discuss options, & document preoperative discussion with pt regarding products pt will/will not accept
• Special legal considerations may apply to minors, incompetent individuals, emergency procedures
• Physicians may opt out of providing care for a JW patient
• JW may agree to some blood conservation (special cell-saver) techniques
• Generally prohibited
• Allogenic transfusion of whole blood, red cells, white cells, platelets, plasma
• Autologous (preoperative donated) blood/blood products
• May be acceptable (discuss with JW)
• Cell-saver scavenging, cardiopulmonary bypass, dialysis, plasmapheresis
• If blood does not come out of a continuous circuit with pt
• Epidural blood patch
• Blood plasma fractions
• Albumin, globulins, clotting factors—factors VIII & IX
• Erythropoietin
• PolyHeme (blood substitute solution—chemically modified human Hgb)
• Hemopure (blood substitute solution—chemically stabilized bovine Hgb)
DISCLOSURE AND APOLOGY—COMMUNICATING ABOUT UNANTICIPATED EVENTS
Triggers for Disclosure
• Interception of a potential error (e.g., wrong site identified during time out)
• Error with no harm (e.g., drug dosing error)
• Adverse/unanticipated event (e.g., failed intubation)
• National Patient Safety Foundation guiding principle:
“When a health care injury occurs, the patient … is entitled to a prompt explanation of how the injury occurred and its short- and long-term effects. When an error contributed to the injury, the patient … should receive a truthful and compassionate explanation about the error and the remedies available to the patient. They should be informed that the factors … will be investigated so that steps can be taken to reduce the likelihood of similar injury to other[s].” (11/14/00)
• The Joint Commission accreditation standards: require the disclosure of sentinel events and other unanticipated outcomes of care
Quick Guide to Breaking Bad News
• Use a quiet, private area free from distractions
• Provide a brief review of the event/unanticipated outcome; Don’t speculate, stick to facts
• Be frank, but kind in your delivery of news
• Pause after your disclosure; silence is OK; Give the patient time to react
• Gauge readiness for more information
• Invite questions
• Assure that physician follow-up is available
• Apologies:
• Avoid these ineffective phrases: “I’m sorry, but…” or “I’m sorry you feel …” → does not show apology for the error, shows sorrow/indifference toward the feelings of the patient/family
• Avoid placing blame
• Be an active listener and signal general agreement when appropriate “yes, good point”, or “I hear what you are saying”
• Practice the 3R’s: Restate, Respect, Respond “Let me repeat, your point is …”
Note: If an adverse event occurs, but was NOT the result of an error or omission, there is no need to apologize; review facts, explain findings and let the pt know it is OK to disagree.
< div class='tao-gold-member'>









