Rapid sequence intubation (RSI) is the preferred method of emergency airway management. It involves the near simultaneous administration of fast-acting induction and neuromuscular blocking agents to achieve optimal intubating conditions without the need for bag-mask ventilation. The following discussion of orotracheal intubation refers to RSI. Techniques for gum-elastic bougie insertion and nasotracheal intubation are also discussed.
INDICATIONS
![]() Failure to protect the airway
Failure to protect the airway
![]() Failure to maintain the airway
Failure to maintain the airway
![]() Failure of ventilation
Failure of ventilation
![]() Failure of oxygenation
Failure of oxygenation
![]() Predicted deterioration or anticipated clinical course requiring intubation
Predicted deterioration or anticipated clinical course requiring intubation
CONTRAINDICATIONS
![]() Orotracheal and Nasotracheal Intubation
Orotracheal and Nasotracheal Intubation
![]() Total upper airway obstruction
Total upper airway obstruction
![]() Total loss of facial landmarks
Total loss of facial landmarks
![]() Nasotracheal Intubation
Nasotracheal Intubation
![]() Apnea
Apnea
![]() Basilar skull or facial fracture
Basilar skull or facial fracture
![]() Neck trauma or cervical spine injury
Neck trauma or cervical spine injury
![]() Head injury with suspected increased intracranial pressure (ICP)
Head injury with suspected increased intracranial pressure (ICP)
![]() Nasal or nasopharyngeal obstruction
Nasal or nasopharyngeal obstruction
![]() Combative patients or patients in extremis
Combative patients or patients in extremis
![]() Coagulopathy
Coagulopathy
![]() Pediatric patients
Pediatric patients
LANDMARKS
![]() Viewing the oropharynx from above, the tongue is the most anterior structure
Viewing the oropharynx from above, the tongue is the most anterior structure
![]() The pouchlike vallecula separates the tongue from the epiglottis, which sits above the larynx (FIGURE 1.1)
The pouchlike vallecula separates the tongue from the epiglottis, which sits above the larynx (FIGURE 1.1)
![]() The vocal cords sit as an inverted “V” within the larynx
The vocal cords sit as an inverted “V” within the larynx
![]() The larynx is anterior to the esophagus
The larynx is anterior to the esophagus
TECHNIQUE FOR OROTRACHEAL INTUBATION
![]() General Basic Steps
General Basic Steps
![]() Preparation
Preparation
![]() Preoxygenation
Preoxygenation
![]() Pretreatment
Pretreatment
![]() Paralysis and induction
Paralysis and induction
![]() Positioning
Positioning
![]() Placement of tube
Placement of tube
![]() Proof of placement
Proof of placement
![]() Postintubation management
Postintubation management
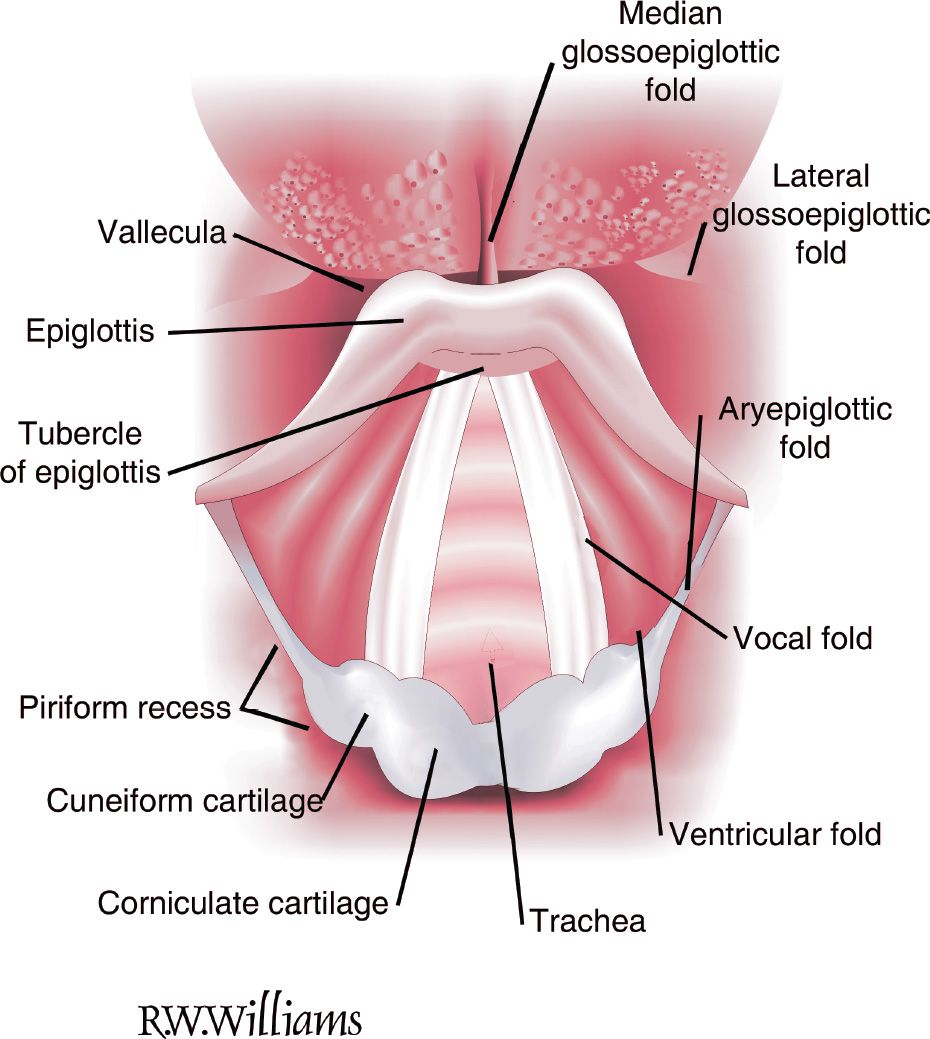
FIGURE 1.1 Larynx visualized from the oropharynx. Note the median glossoepiglottic fold. It is pressure on this structure by the tip of a curved blade that flips the epiglottis forward, exposing the glottis during laryngoscopy. Note that the valleculae and the pyriform recesses are different structures, a fact often confused in the anesthesia literature. The cuneiform and corniculate cartilages are called the arytenoid cartilages. The ridge between them posteriorly is called the posterior commissure. (Reused with permission from Redden RJ. Anatomic considerations in anesthesia. In: Hagberg CA, ed. Handbook of Difficult Airway Management. Philadelphia, PA: Churchill Livingstone; 2000:9.)
![]() Preparation
Preparation
![]() Assess airway: Use LEMON mnemonic to predict difficulty of airway
Assess airway: Use LEMON mnemonic to predict difficulty of airway
![]() Look externally: If you sense that an airway appears difficult, it likely is
Look externally: If you sense that an airway appears difficult, it likely is
![]() Evaluate anatomy: The “3-3-2 rule” (FIGURE 1.2)
Evaluate anatomy: The “3-3-2 rule” (FIGURE 1.2)
![]() Thyromental distance: Should be approximately 3 finger widths. Significantly more or less suggests a difficult airway.
Thyromental distance: Should be approximately 3 finger widths. Significantly more or less suggests a difficult airway.
![]() Mouth opening: Less than 3 finger widths predicts poor visualization on laryngoscopy and a difficult airway
Mouth opening: Less than 3 finger widths predicts poor visualization on laryngoscopy and a difficult airway
![]() Hyomental distance: More or less than 2 finger widths predicts a difficult airway
Hyomental distance: More or less than 2 finger widths predicts a difficult airway
![]() Mallampati score: Roughly correlates the view of internal oropharyngeal structures with intubation success. Graded as class I to IV (FIGURE 1.3).
Mallampati score: Roughly correlates the view of internal oropharyngeal structures with intubation success. Graded as class I to IV (FIGURE 1.3).
![]() Obstruction/Obesity: Any evidence of upper airway obstruction heralds a difficult airway. Obesity is also associated with difficult laryngoscopy.
Obstruction/Obesity: Any evidence of upper airway obstruction heralds a difficult airway. Obesity is also associated with difficult laryngoscopy.
![]() Neck mobility: Crucial to obtaining the optimum view of the larynx. Hindrance to neck extension, including cervical spine immobilization, predicts difficulty in intubation.
Neck mobility: Crucial to obtaining the optimum view of the larynx. Hindrance to neck extension, including cervical spine immobilization, predicts difficulty in intubation.
![]() Equipment
Equipment
![]() Endotracheal tube (ETT) and smaller backup (often 7.5 or 8.0 and 7.0)
Endotracheal tube (ETT) and smaller backup (often 7.5 or 8.0 and 7.0)
![]() 10-cc syringe
10-cc syringe
![]() Laryngoscope blade
Laryngoscope blade
![]() Laryngoscope handle
Laryngoscope handle
![]() Suction
Suction
![]() Rescue airway devices, including oral airway, gum-elastic bougie, and laryngeal mask airway
Rescue airway devices, including oral airway, gum-elastic bougie, and laryngeal mask airway
![]() RSI pharmacologic agents
RSI pharmacologic agents
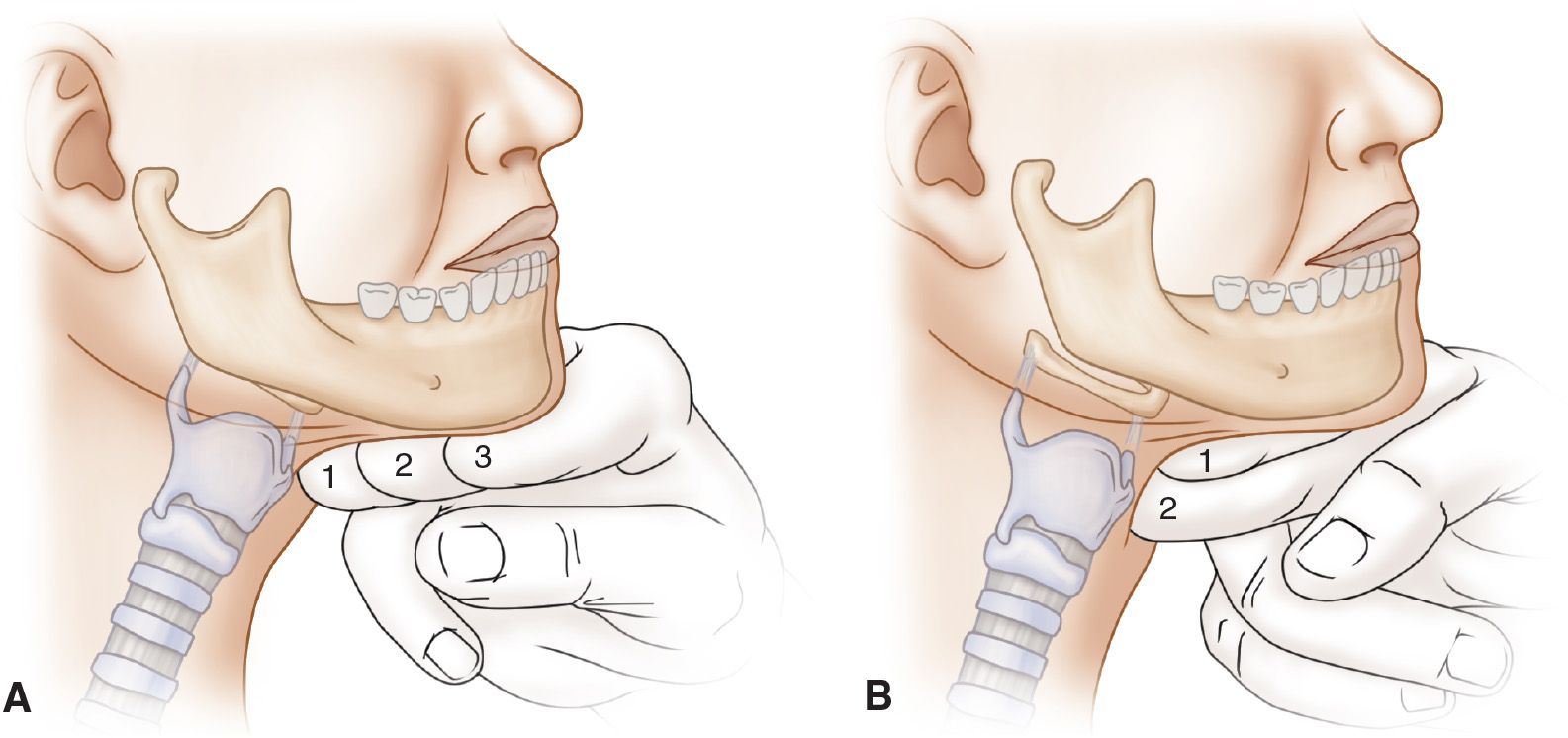
FIGURE 1.2 A: The second 3 of the 3-3-2 rule. B: The 2 of the 3-3-2 rule. (From Walls RM, Murphy MF. Manual of Emergency Airway Management. The 4th edition, 2012 version of the Walls Emergency Manual as well. Philadelphia, PA: Lippincott Williams & Wilkins; 2012:77, with permission.)
![]() Check integrity of ETT cuff
Check integrity of ETT cuff
![]() Ensure that laryngoscope light source is working properly
Ensure that laryngoscope light source is working properly
![]() Make sure IV is functioning
Make sure IV is functioning
![]() Ensure patient is appropriately monitored
Ensure patient is appropriately monitored
![]() Position patient and adjust bed height
Position patient and adjust bed height
![]() Assign team roles
Assign team roles
![]() Prepare for possible surgical airway
Prepare for possible surgical airway
![]() Preoxygenation
Preoxygenation
![]() Theoretically, deliver 100% oxygen for 3 minutes via nonrebreather mask. (In reality, it delivers approximately 70% oxygen.)
Theoretically, deliver 100% oxygen for 3 minutes via nonrebreather mask. (In reality, it delivers approximately 70% oxygen.)
![]() This fills the functional residual capacity with oxygen, replacing nitrogen and allowing for a longer apneic period before desaturation
This fills the functional residual capacity with oxygen, replacing nitrogen and allowing for a longer apneic period before desaturation
![]() When time is critical, preoxygenation can be achieved in eight vital capacity breaths
When time is critical, preoxygenation can be achieved in eight vital capacity breaths
![]() Nasal cannula should be placed to augment preoxygenation and facilitate apneic oxygenation
Nasal cannula should be placed to augment preoxygenation and facilitate apneic oxygenation
![]() Pretreatment
Pretreatment
This refers to the administration of medications to attenuate the potential adverse side effects of intubation. Medications are given 3 minutes prior to intubation. While evidence supporting pretreatment is not conclusive, it should be considered in the following groups of patients:
![]() Elevated ICP: To mitigate ICP increase with laryngoscopy and intubation
Elevated ICP: To mitigate ICP increase with laryngoscopy and intubation
![]() Lidocaine 1.5 mg/kg
Lidocaine 1.5 mg/kg
![]() Fentanyl 3 μg/kg
Fentanyl 3 μg/kg
![]() Cardiovascular disease: To decrease sympathetic response
Cardiovascular disease: To decrease sympathetic response
![]() Fentanyl 3 μg/kg
Fentanyl 3 μg/kg
![]() Reactive airway disease: To reduce bronchospasm
Reactive airway disease: To reduce bronchospasm
![]() Lidocaine 1.5 mg/kg
Lidocaine 1.5 mg/kg
![]() Albuterol 2.5 mg nebulized
Albuterol 2.5 mg nebulized
![]() Paralysis and Induction
Paralysis and Induction
![]() Give the induction agent, as a bolus, in sufficient dose to produce immediate loss of consciousness. Common agents are propofol (1.5–3 mg/kg) and etomidate (0.3 mg/kg).
Give the induction agent, as a bolus, in sufficient dose to produce immediate loss of consciousness. Common agents are propofol (1.5–3 mg/kg) and etomidate (0.3 mg/kg).
![]() Push the paralytic agent immediately following the induction agent. Succinylcholine (1.5–2 mg/kg) is the common first choice in RSI because of its rapid onset.
Push the paralytic agent immediately following the induction agent. Succinylcholine (1.5–2 mg/kg) is the common first choice in RSI because of its rapid onset.
![]() Fasciculations will occur 20 to 30 seconds after the administration of succinylcholine
Fasciculations will occur 20 to 30 seconds after the administration of succinylcholine
![]() Apnea and paralysis will occur almost uniformly by 1 minute
Apnea and paralysis will occur almost uniformly by 1 minute
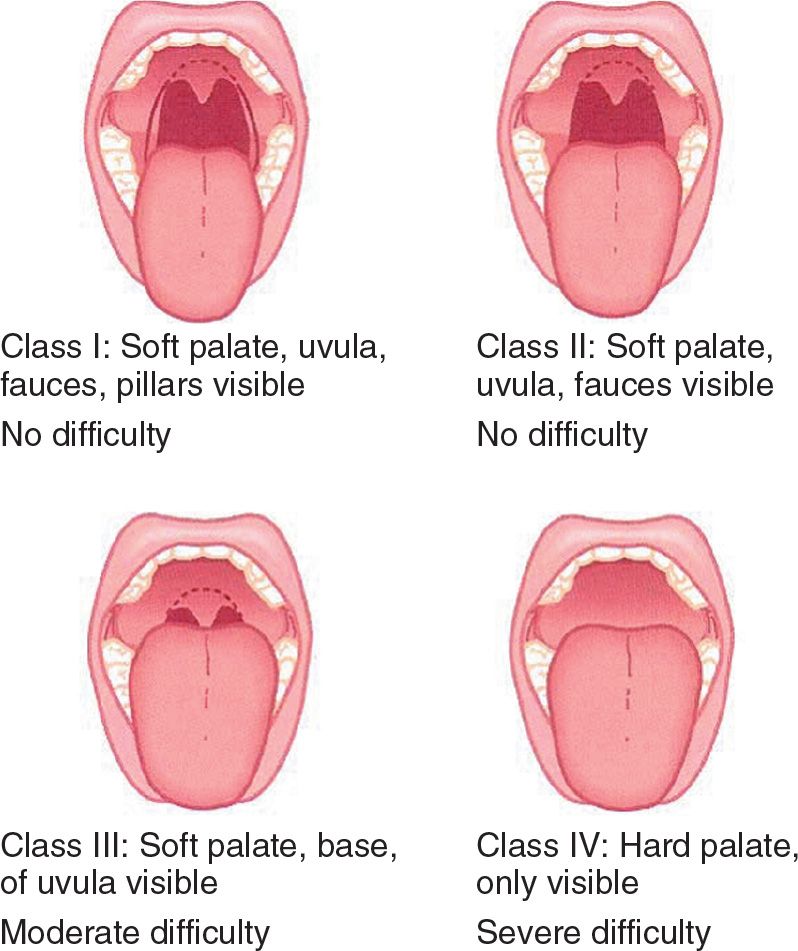
FIGURE 1.3 The Mallampati Scale. (From Walls RM, Murphy MF. Manual of Emergency Airway Management. 4th edition, 2012 version of the Walls Emergency Manual as well. Philadelphia, PA: Lippincott Williams & Wilkins; 2012:78, with permission.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


