![]() Inadequate oxygenation or ventilation
Inadequate oxygenation or ventilation
![]() Airway obstruction
Airway obstruction
![]() Loss of protective airway reflexes (e.g., depressed cough and gag reflexes)
Loss of protective airway reflexes (e.g., depressed cough and gag reflexes)
![]() Excess work of breathing
Excess work of breathing
![]() Nonresponsive and apneic
Nonresponsive and apneic
CONTRAINDICATIONS
![]() Absolute Contraindications
Absolute Contraindications
![]() None for unstable patients (i.e., “crash” airway)
None for unstable patients (i.e., “crash” airway)
![]() Relative Contraindications
Relative Contraindications
![]() In these circumstances one should consider consultation with anesthesiologist/intensivist, alternative techniques, and/or sedation without paralysis
In these circumstances one should consider consultation with anesthesiologist/intensivist, alternative techniques, and/or sedation without paralysis
![]() Infectious: Epiglottitis, croup, retropharyngeal abscess, bacterial tracheitis
Infectious: Epiglottitis, croup, retropharyngeal abscess, bacterial tracheitis
![]() Noninfectious: Anaphylaxis/angioedema, foreign body, trauma, burns
Noninfectious: Anaphylaxis/angioedema, foreign body, trauma, burns
![]() Congenital anomalies (e.g., cleft palate, micrognathia)
Congenital anomalies (e.g., cleft palate, micrognathia)
![]() Unanticipated difficult airway (e.g., multiple failed attempts)
Unanticipated difficult airway (e.g., multiple failed attempts)
RISKS/CONSENT ISSUES
![]() Airway trauma
Airway trauma
![]() Arrhythmia (e.g., bradyarrhythmia)
Arrhythmia (e.g., bradyarrhythmia)
![]() Aspiration of stomach contents
Aspiration of stomach contents
![]() Esophageal intubation
Esophageal intubation
![]() Increase in blood pressure and intracranial pressure (ICP)
Increase in blood pressure and intracranial pressure (ICP)
![]() Hypoxemia
Hypoxemia
![]() Pain
Pain
LANDMARKS
![]() Anatomical differences in children (FIGURE 89.1):
Anatomical differences in children (FIGURE 89.1):
![]() Larger tongue
Larger tongue
![]() Larger and floppy epiglottis
Larger and floppy epiglottis
![]() Narrower cricoid ring
Narrower cricoid ring
![]() Larger occiput
Larger occiput
![]() The glottic opening is more cranial and anterior in children and is located at:
The glottic opening is more cranial and anterior in children and is located at:
![]() C1 in infancy
C1 in infancy
![]() C3–C5 at age 7
C3–C5 at age 7
![]() C4–C6 in the adult (Figure 89.1)
C4–C6 in the adult (Figure 89.1)
![]() Differences are most pronounced under 2 years, transition from 2 to 8 years, then approach small adult anatomy by 8 years
Differences are most pronounced under 2 years, transition from 2 to 8 years, then approach small adult anatomy by 8 years
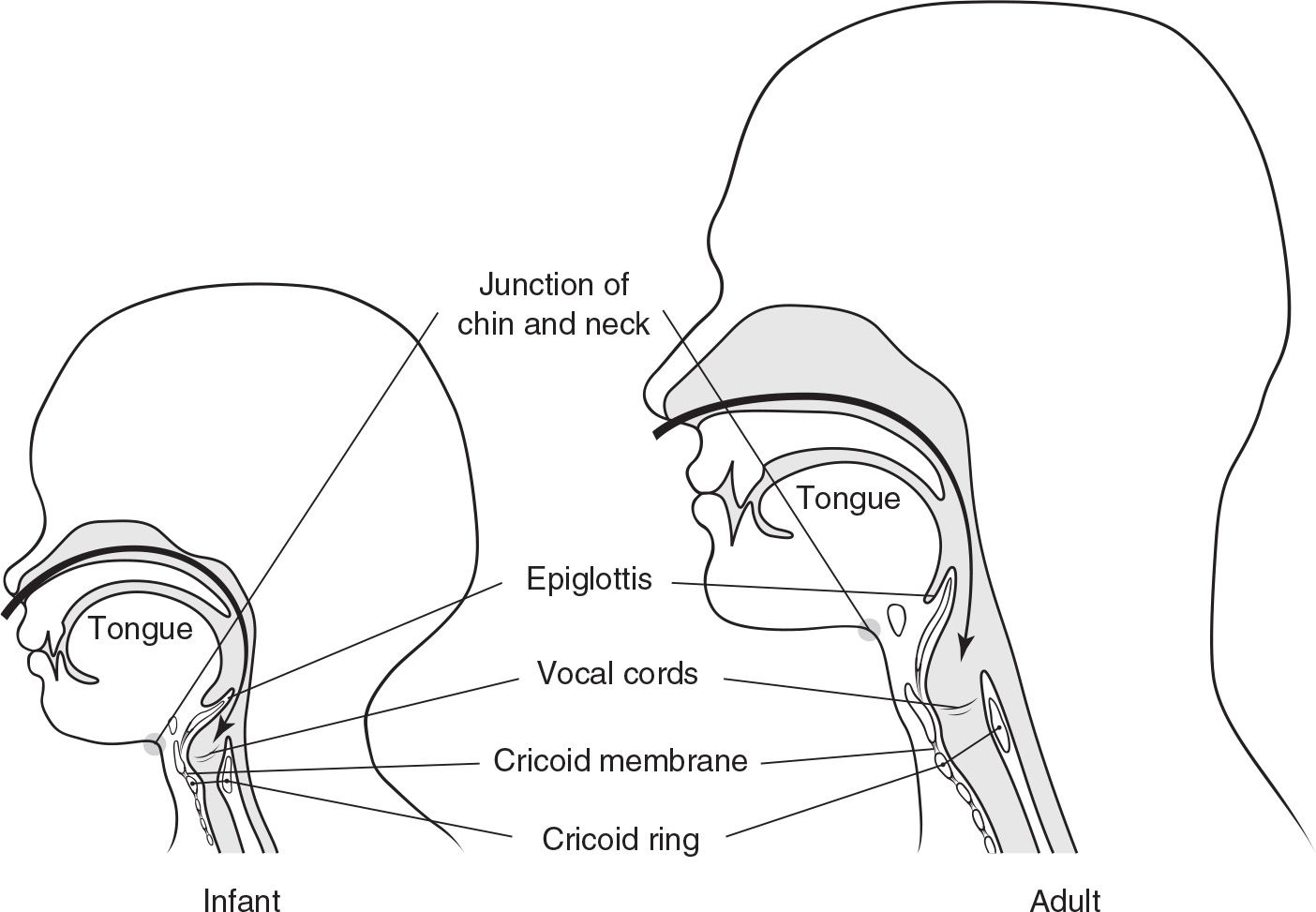
FIGURE 89.1 The anatomic differences particular to children are (a) higher, more anterior position of the glottic opening (note the relationship of the vocal cords to the chin/neck junction); (b) relatively larger tongue in the infant, which lies between the mouth and the glottic opening; (c) relatively larger and more floppy epiglottis in the child; (d) the cricoid ring is the narrowest portion of the pediatric airway versus the vocal cords in the adult; (e) position and size of the cricothyroid membrane in the infant; (f) sharper, more difficult angle for blind nasotracheal intubation; (g) larger relative size of the occiput in the infant.
![]() General Basic Steps
General Basic Steps
![]() Preparation
Preparation
![]() Preoxygenation
Preoxygenation
![]() Pretreatment
Pretreatment
![]() Protection and positioning
Protection and positioning
![]() Paralysis and induction
Paralysis and induction
![]() Placement of tube and proof of tube placement
Placement of tube and proof of tube placement
![]() Postintubation management
Postintubation management
TECHNIQUE
If crash airway and difficult airway algorithms are not indicated, then rapid sequence intubation (RSI) is the preferred approach. This approach is summarized in seven discrete steps, each beginning with the letter “P.”
![]() Preparation: Directed history, physical examination, indications/contraindications for RSI
Preparation: Directed history, physical examination, indications/contraindications for RSI
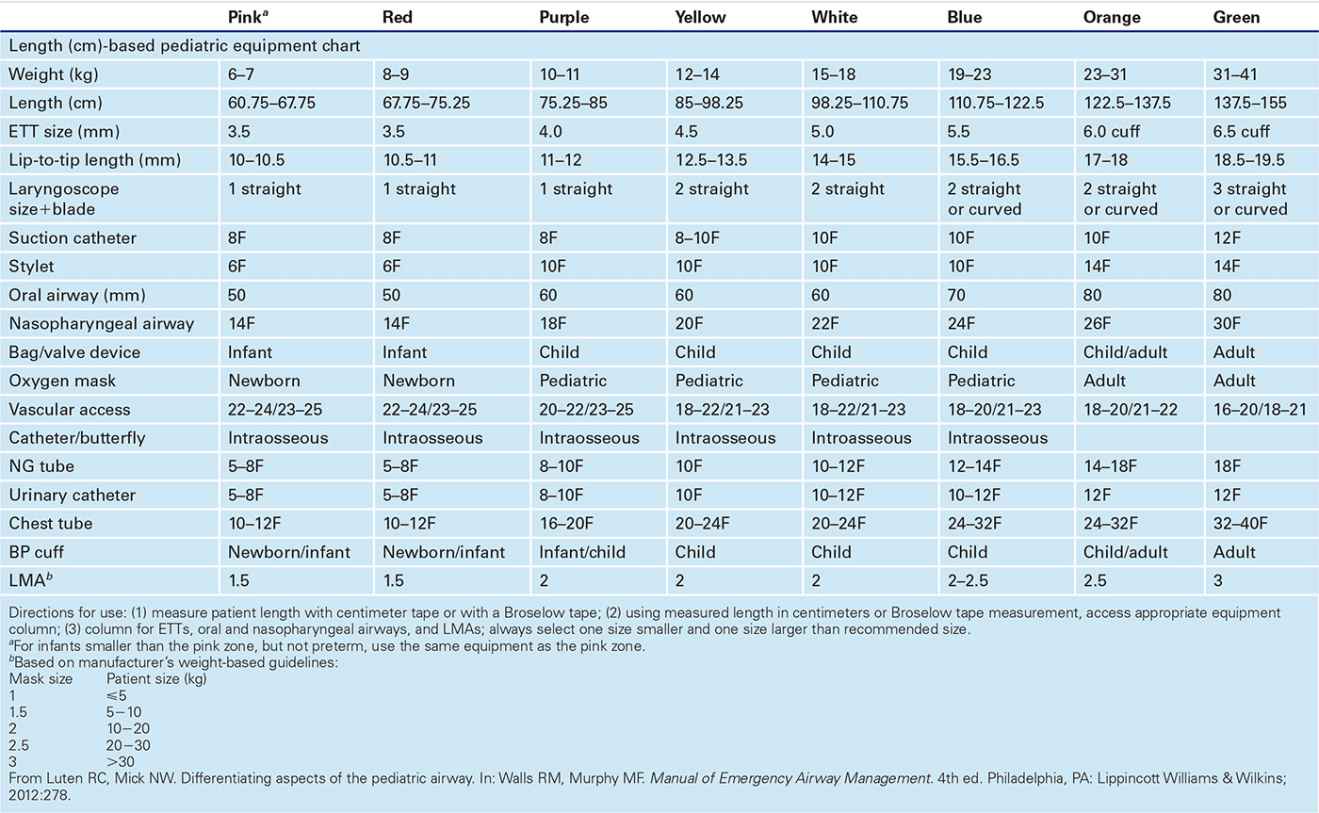
![]() Assemble equipment using the “SOAP ME” mnemonic (TABLE 89.1)
Assemble equipment using the “SOAP ME” mnemonic (TABLE 89.1)
![]() Size is best estimated using Broselow tape or centimeter measuring tape
Size is best estimated using Broselow tape or centimeter measuring tape
![]() Oral airway
Oral airway
![]() Size using Broselow tape or distance from the angle of the mouth to the ear tragus
Size using Broselow tape or distance from the angle of the mouth to the ear tragus
![]() Nasopharyngeal airway
Nasopharyngeal airway
![]() Size using Broselow tape, distance from the tip of the nose to the ear tragus, or largest comfortable size that does not produce skin blanching
Size using Broselow tape, distance from the tip of the nose to the ear tragus, or largest comfortable size that does not produce skin blanching
![]() Laryngoscope blade
Laryngoscope blade
![]() Straight/Miller blade traditionally has been preferred to the curved blade for infants and young children. However, either blade can be used in any age group depending on availability and operator comfort.
Straight/Miller blade traditionally has been preferred to the curved blade for infants and young children. However, either blade can be used in any age group depending on availability and operator comfort.
![]() Endotracheal tube (ETT) size based on Broselow tape or calculated as follows:
Endotracheal tube (ETT) size based on Broselow tape or calculated as follows:
![]() Uncuffed: (Age in years/4) + 4 (subtract 0.5−1 for cuffed tube)
Uncuffed: (Age in years/4) + 4 (subtract 0.5−1 for cuffed tube)
EQUIPMENT FOR RSI—“SOAP ME” MNEMONIC |
S | Suction | Yankaur device (children/adolescents) and/or flexible catheters (infants), suction tubing, wall-mounted suction |
O | Oxygen | Face mask (preferably nonrebreather), oxygen tubing, high-flow oxygen source, Bag/Valve device (with positive-pressure valve) |
A | Airway | Laryngoscope handle with functional light source and blades, endotracheal tubes, airway tape, stylets, oral/nasopharyngeal airways of varying sizes. Rescue equipment (e.g., Bougie, GlideScope, LMA, cricothyrotomy kit, etc.) should be available in case RSI fails. |
P | Pharmacology | Weight-based medications should be prepared in advanced. Agent selection will depend on circumstances and may include sedatives, induction agents, neuromuscular-blocking agents, lidocaine, and atropine. |
ME | Monitoring equipment | Cardiorespiratory monitoring with pulse oximetry and frequent blood pressure checks through postintubation monitoring phase. Following endotracheal tube placement, secondary confirmation with end-tidal CO2 calorimeter (qualitative/semiquantitative) and/or capnography (quantitative) |
LMA, laryngeal mask airway; RSI, rapid sequence intubation. | ||
![]() Historically, uncuffed tubes were preferred in infants and young children due to high rates of subglottic stenosis. Currently, either tube may be used in any age group if leak pressures are monitored.
Historically, uncuffed tubes were preferred in infants and young children due to high rates of subglottic stenosis. Currently, either tube may be used in any age group if leak pressures are monitored.
![]() Prepare extra tubes, both 0.5 size smaller and larger than estimated
Prepare extra tubes, both 0.5 size smaller and larger than estimated
![]() A stylet can be used to provide rigidity (TABLE 89.2)
A stylet can be used to provide rigidity (TABLE 89.2)
![]() ETT depth by Broselow tape or calculated (if age >1 year)
ETT depth by Broselow tape or calculated (if age >1 year)
![]() Formula (in cm): (Age in years/2) + 10 or Tube size × 3
Formula (in cm): (Age in years/2) + 10 or Tube size × 3
![]() End-tidal CO2 monitor
End-tidal CO2 monitor
![]() If weight <15 kg, use pediatric calorimeter to avoid false negative readings
If weight <15 kg, use pediatric calorimeter to avoid false negative readings
![]() Have airway alternatives available (e.g., GlideScope, Airtraq, laryngeal mask airway [LMA], Bougie, needle cricothyrotomy equipment)
Have airway alternatives available (e.g., GlideScope, Airtraq, laryngeal mask airway [LMA], Bougie, needle cricothyrotomy equipment)
![]() Preoxygenation
Preoxygenation
![]() Theoretically, deliver 100% oxygen for 3 minutes. Practically, use nonrebreather facemask (with positive end-expiratory pressure [PEEP] valve) and high-flow nasal cannula once RSI is considered.
Theoretically, deliver 100% oxygen for 3 minutes. Practically, use nonrebreather facemask (with positive end-expiratory pressure [PEEP] valve) and high-flow nasal cannula once RSI is considered.
![]() If child becomes apneic, use bag valve mask (BVM) ventilation prior to intubation
If child becomes apneic, use bag valve mask (BVM) ventilation prior to intubation
![]() Perform neck extension and E-C clamp technique with bag-mask ventilation (BMV) if C-spine injury is not suspected
Perform neck extension and E-C clamp technique with bag-mask ventilation (BMV) if C-spine injury is not suspected
![]() If two providers are available, one person maintains mask seal while the other compresses the bag
If two providers are available, one person maintains mask seal while the other compresses the bag
![]() Use the rhythm “squeeze, release, release” to allow time for exhalation
Use the rhythm “squeeze, release, release” to allow time for exhalation
![]() Insert an oral airway in an unconscious patient who is difficult to ventilate
Insert an oral airway in an unconscious patient who is difficult to ventilate
![]() Pretreatment: Refers to the administration of medications to attenuate the potential adverse effects of intubation (TABLE 89.3)
Pretreatment: Refers to the administration of medications to attenuate the potential adverse effects of intubation (TABLE 89.3)
![]() Prior recommendations summarized by “LOAD” (Lidocaine, Opioid, Atropine, Defasciculating agent)
Prior recommendations summarized by “LOAD” (Lidocaine, Opioid, Atropine, Defasciculating agent)
![]() No pretreatment agent is recommended routinely for pediatric RSI
No pretreatment agent is recommended routinely for pediatric RSI
![]() Lidocaine: May limit further rise in ICP in cases of head trauma or elevated ICP
Lidocaine: May limit further rise in ICP in cases of head trauma or elevated ICP
![]() No data to suggest or refute use to prevent reflex bronchospasm
No data to suggest or refute use to prevent reflex bronchospasm
![]() Fentanyl: Analgesic effects may decrease the reflex sympathetic response
Fentanyl: Analgesic effects may decrease the reflex sympathetic response
![]() May cause hypotension or respiratory depression with other sedatives
May cause hypotension or respiratory depression with other sedatives
![]() Atropine: Used for its anticholinergic effects to prevent or treat bradyarrhythmias
Atropine: Used for its anticholinergic effects to prevent or treat bradyarrhythmias
![]() Antisialogogue effect is delayed, limiting its use in RSI
Antisialogogue effect is delayed, limiting its use in RSI
![]() Interferes with pupillary response of the neurologic examination after paralysis
Interferes with pupillary response of the neurologic examination after paralysis
![]() Defasciculating agent: “Defasciculating” and “Priming” doses are no longer recommended
Defasciculating agent: “Defasciculating” and “Priming” doses are no longer recommended
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


