Introduction to Procedural Sedation
Rahim Valani
Procedural Sedation and Analgesia
Procedural sedation is the technique of administering a sedative or dissociative agent to induce a state that allows the patient to tolerate unpleasant procedures.
Also known as procedural sedation and analgesia (PSA) if analgesia is administered concomitantly.
Now advocated as a core competency in emergency medicine.
Sedation is a continuum (see Figure 1.1 and Table 1.1):
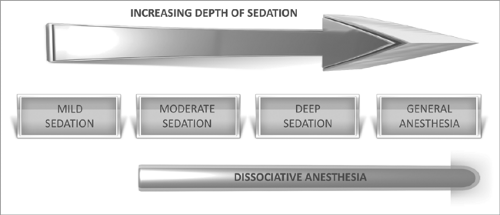
Figure 1.1: Sedation is a continuum, and a patient can easily move from deep sedation to general anesthesia.
PSA is a common practice in the emergency department (ED). The goals of PSA are as follow:
Provide the patient with a safe environment where a painful or unpleasant procedure is required.
Alleviate patient anxiety.
Minimize physical discomfort.
Maximize amnesia.
Control motor behavior and movement if necessary so as to perform painful/unpleasant procedures such as a lumbar puncture or fracture reduction.
Minimize the risk of the procedure, and ensure safe discharge of the patient from the ED.
Table 1.1: Continuum of sedation: levels of sedation and analgesia
Responsiveness
Airway
Ventilation
Cardiovascular function
Mild sedation (anxiolysis)
Responds to verbal commands
Unaffected
Unaffected
Unaffected
Moderate sedation
Purposeful response to verbal or tactile stimuli
No intervention required
Adequate
Usually maintained
Deep sedation
Purposeful response to painful stimuli
Intervention may be required
May be inadequate
Usually maintained
General anesthesia
Unarousable
Intervention required
Inadequate
Impaired
Appropriate policies and protocols enable a safe practice within the ED.
Ensure quality control while minimizing risks and adverse outcomes.
Preprinted orders and monitoring sheets should be a requirement for any department performing PSA.
There is an increased need for the use of PSA in the ED due to the following:
Hospital overcrowding – there may be a potential to avoid an admission to the hospital by performing the procedure in the ED and discharging the patient home safely.
Limited availability of anesthesia – the anesthesia team may be in the operating room, and not available for PSA either in the ED or in the operating room.
Increased training of emergency physicians in PSA.
The most common procedures using PSA performed in the ED are as follow:
Orthopedic procedures (most common, and includes dislocations, fracture reductions, and immobilization/splinting).
Abscess incision and drainage.
Laceration repair.
Cardioversion.
Foreign body removal.
Lumbar puncture.
Endoscopy.
The role of PSA is expanding in the ED as it has been shown to:
Increase convenience of the patient – they no longer need to wait to go to the operating room.
Accessibility – procedures can now be done in the ED so as to facilitate easier access.
Cost-effectiveness by reducing wait times, earlier patient discharge, and avoidance of operating room personnel and time.
Exclusion criteria and contraindications for ED sedation include:
Sedation time >30 minutes.
Patient with a potentially difficult airway (see Chapter 2).
Patient with ASA functional class III or greater (see Table 4.2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




