CHAPTER 36
Intradiscal Biacuplasty
INTRODUCTION
Approximately 45% of back pain can be attributed to discogenic source.1,2 Lumbar discogenic pain is typically caused by pathophysiological changes that occur within the intervertebral disc. A loss of hydration in the nucleus pulposus from aging, chronic abnormal posturing, or injury can lead to both, delamination and fissuring in the annulus fibrosus (Figure 36-1A, B). This structural damage is a part of unclear degenerative process, where in addition to described changes, there is an in-growth of the nerve endings (nociceptors) that are normally restricted to the outer third of the annulus, extending now to the nucleus of the affected disc. Inflammatory cytokines such as tumor necrosis factor, nitric oxide and metalloproteinases, are also released, causing pain through several possible mechanisms. These changes transform the disc into a primary nociceptive structure. In addition, structural changes intrinsic to the intervertebral disc can lead to reduced mechanical load-bearing capacity resulting in altered spinal biomechanics, which can contribute to future back pain.
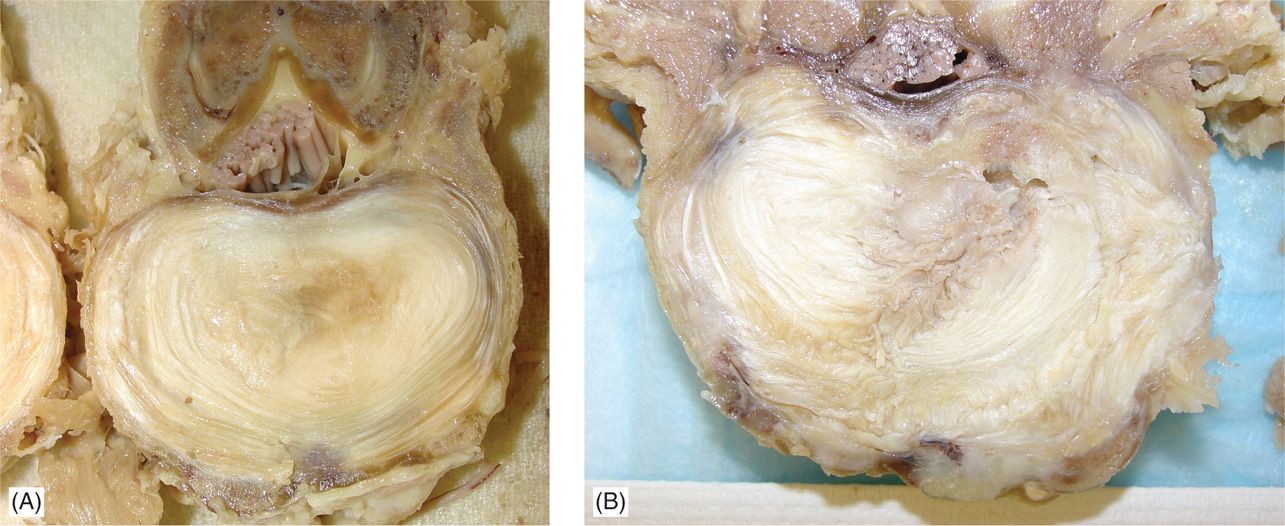
Figure 36-1. Comparison between intact and fairly degenerated lumbar disc. Preparation was fixed in 10% neutral buffered formalin for 1 week. Individual lumbar segments were prepared, taking care to preserve the posterior elements. (A) Mostly intact annulus with minor lamellar disorganization in a minimally degenerated disc with the absence of fissuring. (B) Lamellar disorganization in a degenerated lumbar disc with presence of radiating tear extending to the outer 1/3 of the annulus.
Intradiscal biacuplasty (Figure 36-2) is the latest minimally invasive, posterior annulus heating procedure (annuloplasty) for treatment of discogenic pain. This technique employs two bipolar electrodes, between which bipolar radiofrequency lesioning is conducted. The use of internally cooling electrodes provides for stable and relatively even heating over a large portion of the posterior annulus. Throughout the entire procedure, the patient is awake and able to communicate with the physician. This allows feedback from the patient, and reassurance from the physician, as the probes are positioned and radiofrequency heating conducted. With the patient laying prone, 2 TransDiscal electrodes are inserted bilaterally via introducers using fluoroscopic guidance. Once positioned in the posterior annulus, and confirmed by fluoroscopic imaging, RF generator delivers controlled energy to the tissue. The temperature change is measured via strategically positioned thermocouples near the tip of the probe. Over a period of approximately 10 minutes, the heat delivered should increase temperature of the internal thermo sensor incrementally to 50°C, and then maintained for an additional 5 minutes. The procedure has been shown to lead to significant pain relief at 3, 6, and 12 months, as well as the improvements in functional capacity and patient satisfaction. While still a recently described technique, it appears to be the most promising of all annuloplasty methods. Randomized controlled studies are ongoing, and further evaluation is needed.

Figure 36-2. Intradiscal biacuplasty electrodes properly positioned in bipolar fashion via introducers inside the patients back.
INDICATIONS
Currently, the approved indication for the lumbar biacuplasty is a persistent discogenic lower back pain, despite comprehensive conservative treatment, including physical therapy and a directed exercise1,2 programs. Additional patient selection criteria which, if used, may yield better clinical results include: lack of neural compressive lesion on lumbar spine magnetic resonance imaging (MRI) and reproduction of concordant pain in the lower back area during the provocative discography at a low pressurization in 1 or 2 lumbar intervertebral discs.
BASIC CONCERNS AND CONTRAINDICATIONS
• Contraindications for intradiscal biacuplasty are consistent with contraindications for other disc annuloplasty procedures, and include presence of disc height of less than 50% then adjacent disc when measured on lateral radiographs, and presence of disc degeneration at greater than 2 lumbar levels on sagittal planes of spinal MRI.3
• Relative contraindications for biacuplasty also include significantly overweight patients4 and patients receiving workman’s compensation benefits.4–6 Inclusion criteria for past studies evaluating the efficacy of intradiscal thermal annuloplasty could also be used to aid in identification of patients with the highest potential to benefit from biacuplasty. This criteria could be considered additional relative contraindications and include positive straight leg raise, the presence of any inflammatory arthritis, nonspinal conditions that can mimic lumbar pain, or previous surgical intervention at the symptomatic intervertebral disc level.
SUMMARY OF INDICATIONS/CONTRAINDICATIONS
Primary Indication
• Chronic discogenic low back pain unresponsive to nonoperative/conservative care >6 months
Discogenic pain evidenced by:
![]() Positive provocative discography at low pressurization (>=7/10, at a pressure of <=50 psi above opening pressure with a central disc injection)
Positive provocative discography at low pressurization (>=7/10, at a pressure of <=50 psi above opening pressure with a central disc injection)
![]() Concordant pain reproduction present on provocative discography
Concordant pain reproduction present on provocative discography
Positive Candidate Selection Criteria
• Disc height more than 50% of adjacent disc height on sagittal imaging
• Single level disease or 2 levels of disease without evidence of additional degenerative changes
Absolute Contraindications
• Evidence of compressive radiculopathy
• Symptoms or signs of the lumbar canal stenosis
• Evidence of internal nucleus pulposus herniation on MRI
• Lack of consent
• Pregnancy
• Local infection at injection site
• Systemic or CNS infection
Relative Contraindications
• Obesity
• Workman’s compensation claim
• Inflammatory arthritis
• Underlying psychological pathology
• Prior surgery at the symptomatic level
Relevant Anatomy
Intervertebral disc is cartilaginous enclosure between 2 vertebral bodies. Posterior to the disc, 2 facet (or zygapophysial) joints, composed of the superior articulating process of the vertebral level below the disc and the inferior articulating process of the vertebral level above the disc, articulate and provide protection against excessive flexion and extension of the spine and also limit sheer forces on the annulus of the disc. The nucleus pulposus (NP) is the gelatinous structure in the center of the disc that lacks any blood supply and is composed of proteoglycan aggrecan, collagen fibrils, chondrocytes, and water. The NP is contained by the annulus fibrosus (AF), made mostly of type I collagen, and vertebral end plates (VE), which are cartilaginous plates that supply nutrients to the inner two-thirds of the annulus and the entirety of the NP. An intact, healthy disc is an avascular structure. All nutrition demands of the discus intervertebralis are met by diffusion through the VE and AF. Diffusions of these nutrients, including oxygen, can be compromised following injury and resultant inflammation.
The innervation of the disc is quite complex.7
• Bundles of sensory nerves, branching through rami communicantes, project both above and below the spinal nerve and ganglion.
• Direct fibers from the sympathetic truncus join to form the sinuvertebral nerve, which continue to branch and innervate the circumference of the AF.
The sinuvertebral nerve contains nociceptive, sympathetic, proprioceptive, and vasomotor nerve fibers.8–13 These anatomical studies have shown the close relationship between the sensory fibers and sympathetic fibers, which could explain why lumbar sympathetic blocks14,15 and RF ablation of the ramus communicans16 has been shown to help in patients with discogenic pain.
• The sinuvertebral nerves diverge and project fibers ventrally and dorsally and send branches into the lateral aspects of the AF.
• As the nerve fibers reach the ventral and dorsal aspects of the annulus, they split into finer branches forming several complicated neural networks.
• These plexiform structures innervate the anterior longitudinal ligament (ALL), ventrally and posterior longitudinal ligament (PLL) and ventral dura, dorsal to the disc.7
• These plexi are rich with craniocaudal connections from adjacent spinal segments, as well as bilateral (transverse) neural contributions7,17 and ultimately innervate the ventral and posterior aspects of the disc.18
• This multi-segmented, transverse innervation pattern could account for the varied and often dynamic complaints of patients with discogenic pain.
The key structures to successfully attaining optimal placement of the electrodes lies in identifying the following structures:
• Spinous process
• Lamina
• Corpus vertebrae
• Superior articular process
• Inferior articular process
• Intervertebral foramen
• Pedicles or root of the vertebral arch
• Transverse process
• Posterior annulus fibrosus of the intervertebral disc
Other relevant anatomy that should be taken into consideration when performing this procedure:
• Vertebral end plates
• Existing nerve roots
• Ramus ventralis
• Vertebral arteries
• Erector spinal muscles
Preoperative Considerations
• Informed consent and explanation of potential complications
• Allergies
• Physical examination of lumbar area for anomalous anatomy, infection, or skin ulceration
• Ability of patient to lie prone during procedure
• IV fluids and medications for sedation/analgesia
Fluoroscopic Views
• Start procedure with oblique view of approximately 30 degrees, such that half of the disc is lateral to the SAP. At this angle with the radiation beam parallel to the VE, the height of the disc is maximized (Figures 36-3 and 36-4).
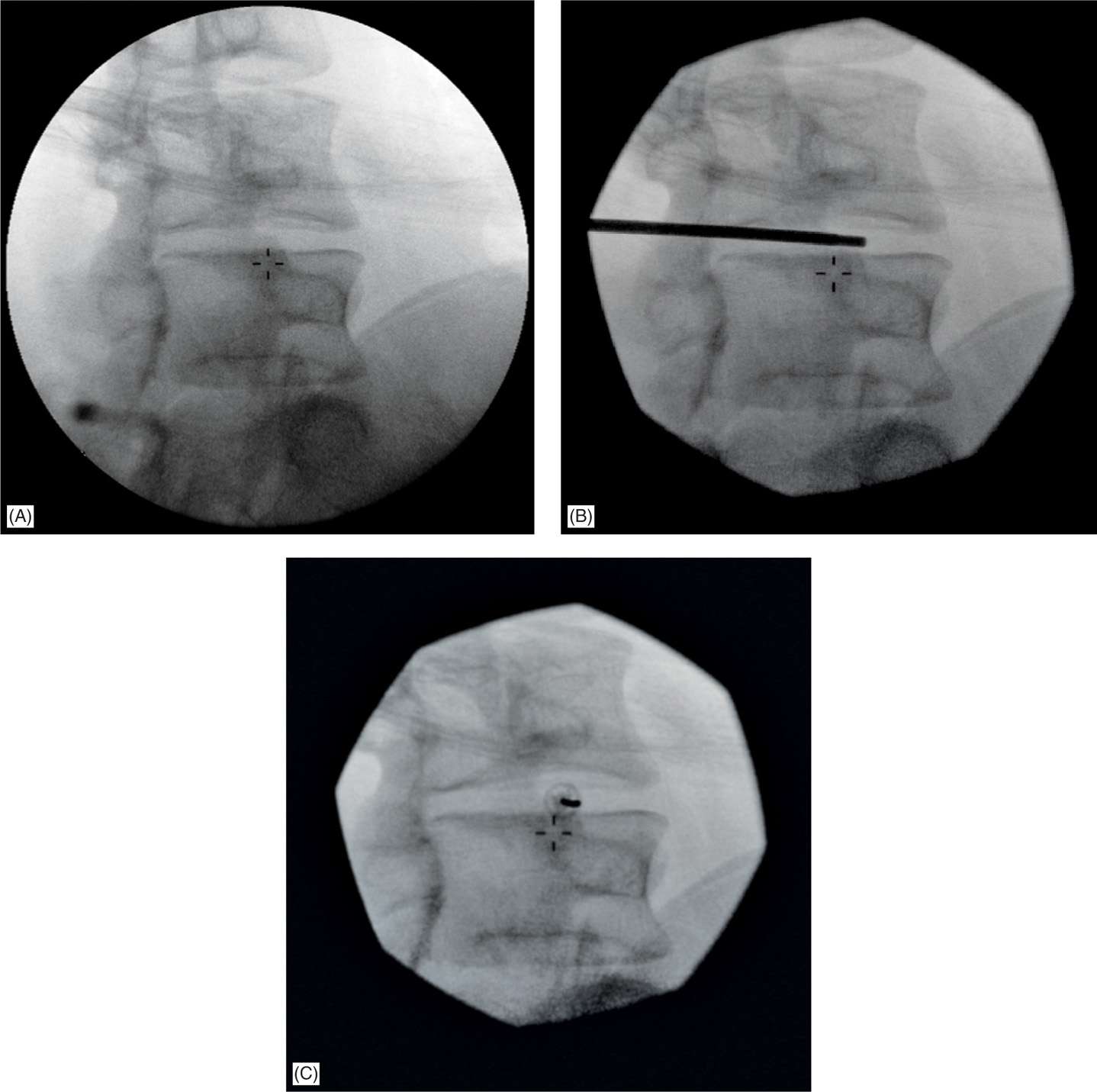
Figure 36-3. Initially the biacuplasty introducer is positioned from the oblique view by rotating the fluoroscopy C-arm to position where the superior articular process of the vertebral level below is moved to about one half the width of the vertebral column. This view allows optimal placement of two electrodes to form a bipolar configuration with approximate distances of less than 3 cm. Notice that the lower end plate is lined (A), pointer placed just next to SAP (B), and then introducer placed (C) via which an electrode will be positioned.
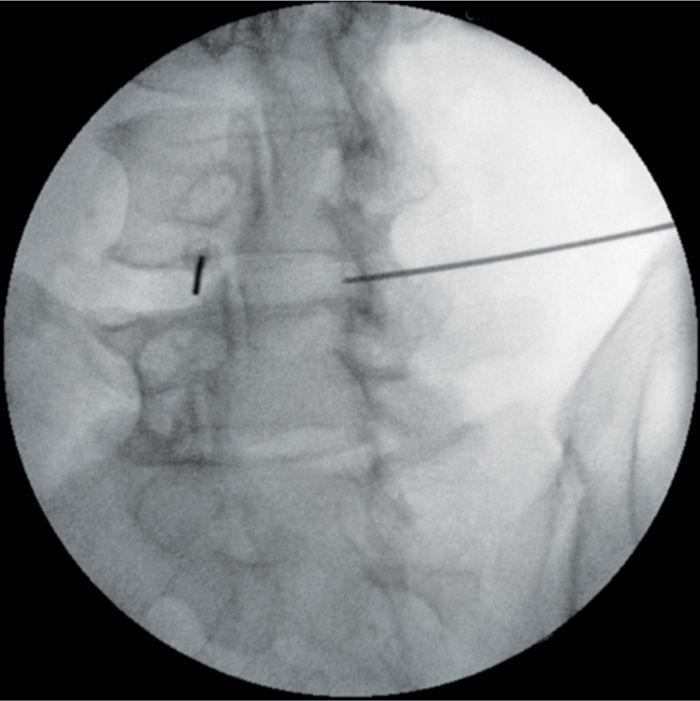
Figure 36-4. Same procedure should be repeated on the opposite side with an introducer placed from the oblique view. Again closeness of the introducer tip to the SAP prevents unnecessary paresthesias.
• Confirm placement of the introducers with anterior-posterior (AP) view. The introducer tips should appear to be within the medial edge of the pedicles (Figure 36-5).
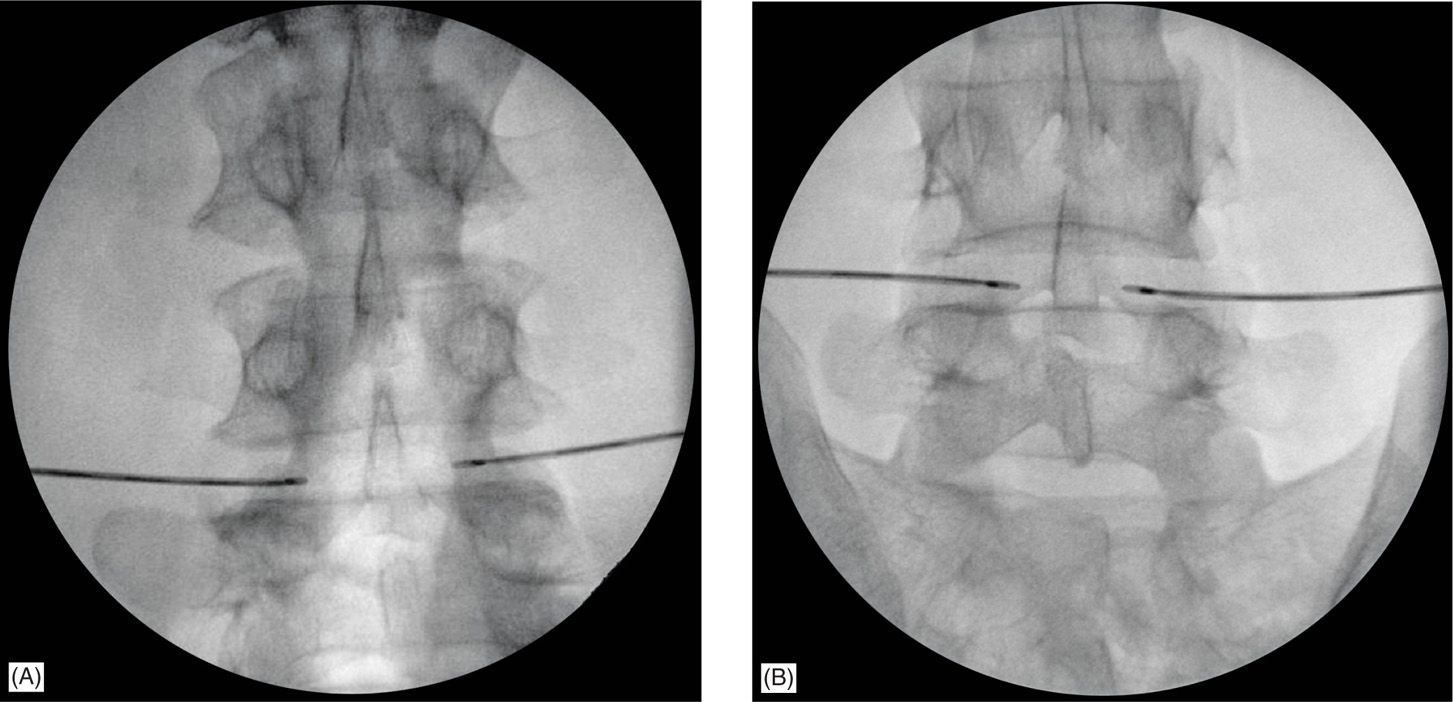
Figure 36-5. Wider angle of insertion may be necessary for large discs to maintain maximum distance between probes to be 2.5 cm to 3 cm. Approach angle should be adjusted from 30 degrees (A) to 45 degrees (B) from the median. Increased approach angle brings probes close enough to create a confluent lesion.
• Once the electrodes have been placed into the disc, positioning and depth should be confirmed with both AP and lateral views with the electrodes just piercing the posterior annulus of the disc (Figures 36-5 and 36-6).
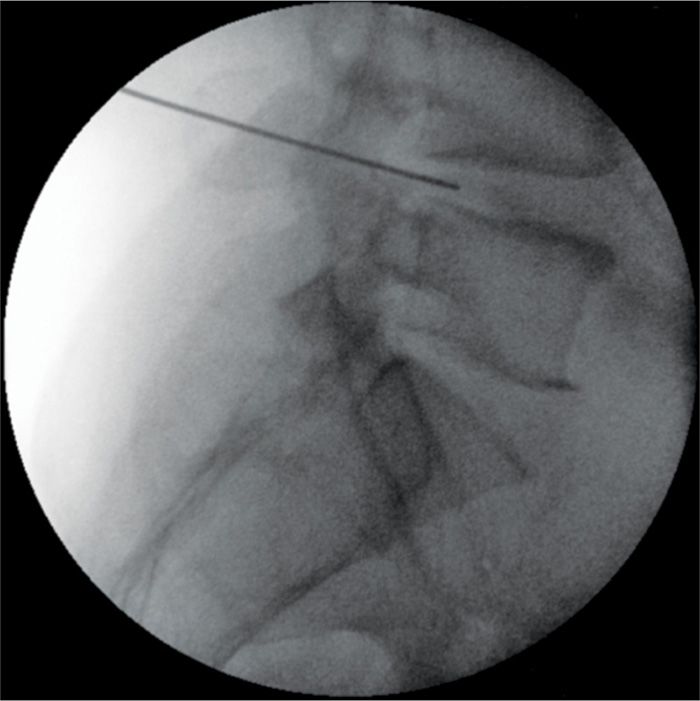
Figure 36-6. Assessment of the introducer depth in the lateral view. Notice that initially (like here with L4-L5 disc) an introducer may be slightly deeper that final electrode position would require. However, no adjustment of introducer is needed. Once when biacuplasty electrode is placed via introducer, it may be pulled out slightly in order to position an active tip within last portion of the annulus.
Equipment
• 25-gauge 1.5-in needle for infiltration
• 10-cc syringe for local anesthetic
Medications
• 0.5% to 1% lidocaine
Technique
The intradiscal biacuplasty procedure is a minimally invasive annuloplasty technique using radiofrequency heat delivery to the posterior annulus of the disc.
• Intravenous access should be obtained and 5-lead electrocardiogram, continuous pulse oximetry, and noninvasive blood pressure monitors are placed.
• Prophylactic intravenous antibiotics were administered 15 to 40 minutes prior to beginning of the procedure.
• The procedure is completed under fluoroscopy, with the patient lying prone and minimal sedated.
• The C-arm of the fluoroscope should be positioned obliquely at approximately 35 to 45 degrees, until the lateral aspect of superior articular process (SAP) is located in the axial middle of the disc.
• With the C-arm properly positioned, a 17-gauge TransDiscal introducer is advanced in parallel with the radiation beams (tunnel view) and directed just lateral SAP approaching the disc posterolaterally at approximately the center of the disc height. This ensures that the electrodes are away from both the nerve roots and the vertebral end plates to increase the safety of the procedure.
• The introducers are advanced until the tips appear to be within the medial edge of the pedicles in an anteroposterior (AP) view.
• Next, an 18-gauge TransDiscal probe (Figures 36-5, 36-7, and 36-8) is advanced through the introducer and positioned inside the disc.
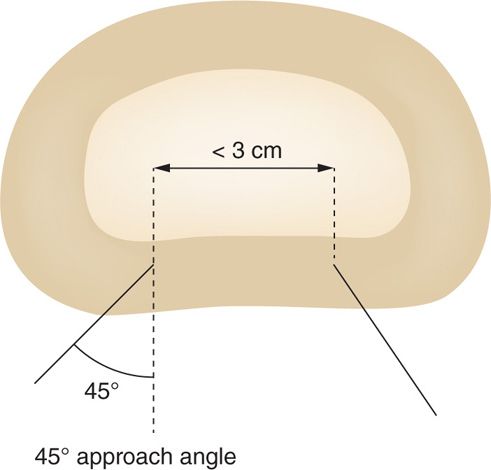
Figure 36-7. Schematic explains on how such wider angle of introducer insertion is achieved within a larger discs to maintain that optimal distance between the probes. Typically, angle taken is about 45 degrees.
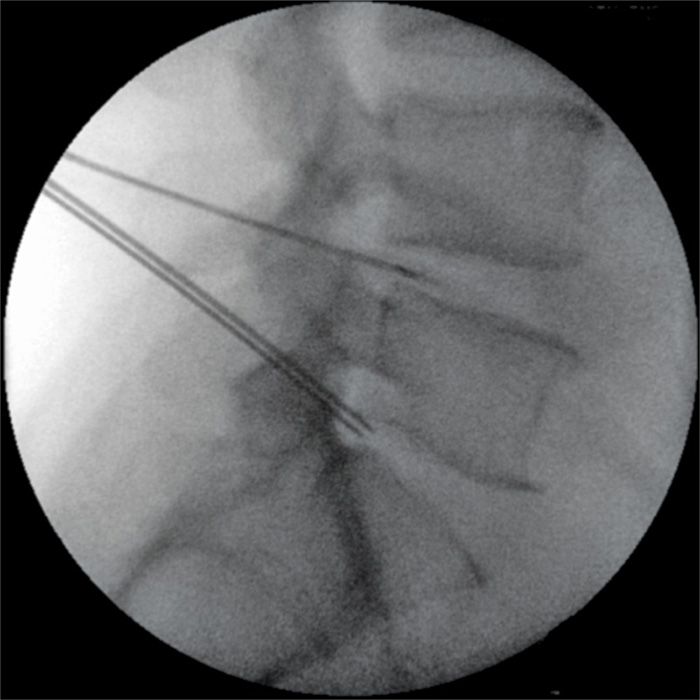
Figure 36-8. Two level biacuplasty in progress with already positioned electrodes within the L4-L5 intervertebral disc and 2 introducers just placed into L5S1 disc observed from the lateral fluoroscopic view. Notice that the tips of the introducers just pierced into the posterior annulus of L5S1 disc.
• Appropriate positioning and depth of probe are assessed by checking AP and lateral views of the lumbar spine (Figures 36-5, 36-8, and 36-9). This procedure is repeated on the opposite side, so that when positioned, the two probes form a bipolar configuration.
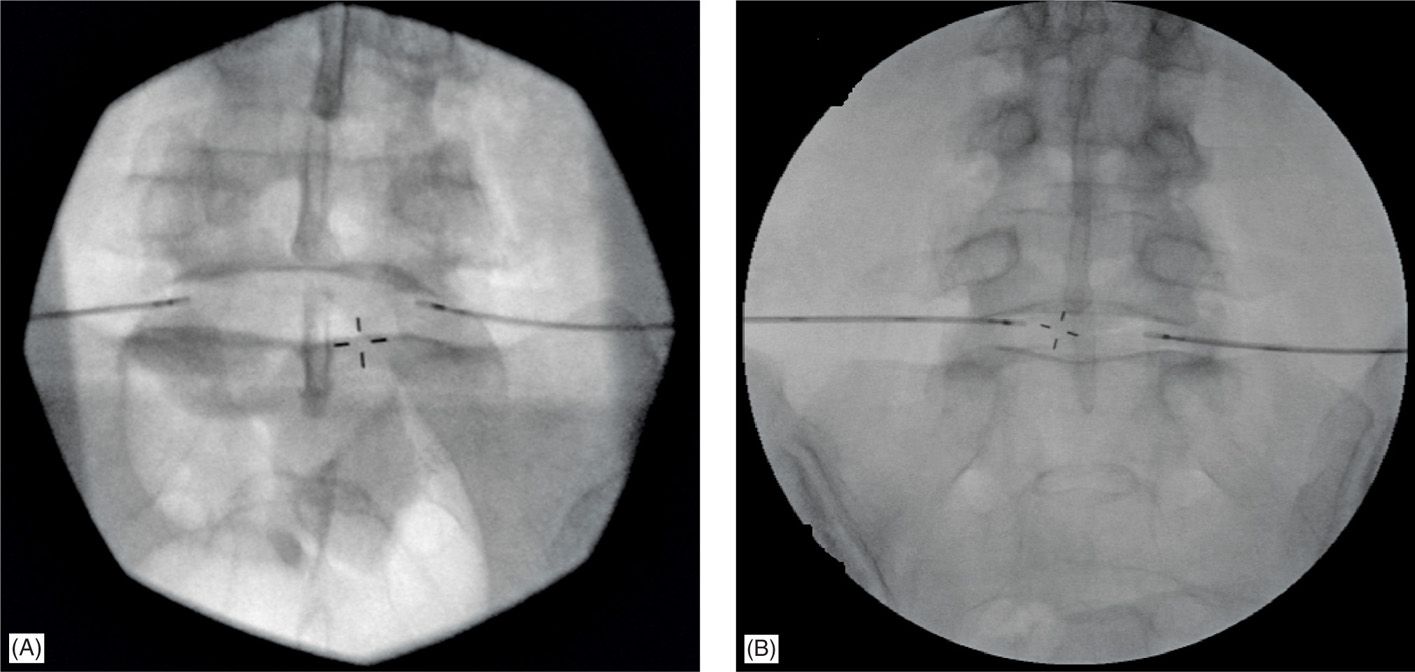
Figure 36-9. Two common mistakes when biacuplasty electrodes positioned within the lumbar discs. (A) Angles on which introducers were positioned are small and distance between 2 electrode tips is greater than 3 cm. Not sufficient to achieve an effective bipolar configuration with optimal level of heat in the middle. (B) One of the electrodes is too close to the end plate even after upper end plate was lined up in anterior-posterior view. That can produce an extensive heat and damage to the end plate of the disc.
• The generator controls the delivery of RF energy by monitoring the temperature measured by a thermocouple at the tip of the probe.
• The temperature increases gradually over a period of 10 minutes to 50°C, with final heating at 50°C for another 5 minutes.
• It should be noted that, although the temperature is set to 50°C on the RF generator, tissue temperature reaches 70 to 75°C because of ionic heating.
• Throughout the entirety of the procedure, the patient is minimally sedated, but awake and able to communicate with the physician, reducing the risk of neurological injury.
• Delivery of the heat to posterior annulus itself usually is not painful, frequently patients report mild transient back discomfort without significant leg pain.
• Once the procedure is completed, patients were transferred to a recovery area and monitored for 45 minutes prior to discharge with postprocedural instructions and a stabilizing brace to be worn when awake.
POSTPROCEDURE FOLLOW-UP
Following completion of the procedure, the patient should go through a specific physical therapy program over a rehabilitation period.
• Written post-op instructions should be provided to the patient.
• Oral opioid may be used for 1 to 2 weeks, after which nonsteroidal anti-inflammatory drugs (NSAIDs) should be adequate.
• The use of muscle relaxants is optional and should be based on patient’s symptomatology.
• A lumbar sacral orthosis (LSO) should be worn for 4 to 6 weeks after the procedure.
• A lumbosacral functional restoration program is highly recommended and is further described below.
• Patient education should be provided on how to prevent re-injury and return to work or usual activities carefully planned.
Written post-op instructions should contain the following:
1. Activity restrictions/guidelines
2. Proper use of orthosis
3. Emergency telephone numbers and appointment date for follow-up
4. Explanation of expectable postprocedure pain, and recommendations on the adjunctive use of ice/heat.
These directions should also contain a brief description of the warning signs of post-op complications such as:
• Stiff neck
• Increasing pain
• Lower extremity paresthesia
• Motor deficits
• Bladder or bowel dysfunction
• Wound site drainage
Special emphasis should be placed on appropriate post-op orthosis use. California LSO is frequently well tolerated, although other orthoses can be used.
The orthosis should be carefully fit to the patient with about 15 degrees of lordosis and patient should be instructed to bring it to operation room for immediate post-op use. The brace may be removed briefly for personal hygiene activities.
FUNCTIONAL REHABILITATION AFTER BIACUPLASTY
Week 1:
Short periods of walking after procedure
No driving
10 lb lifting limit only
Week 2:
Gentle stretches
Lifting restrictions of 20 to 40 lb × 12 weeks
Avoid strenuous activity, twisting or sustained flexion
Option to begin gentle lumbar stabilization exercises with neutral bias and abdominal strengthening
Instruct therapist to avoid truncal rotation
No manual therapy
Weeks 3-4:
Therapist guided stretching, strengthening, ROM. Begin neutral-biased dynamic stabilization program. May remove orthosis during PT sessions.
Limit L/S flexion to 40 degrees and torsion to 30 degrees during these weeks.
If not well tolerated in first sessions, may convert to aquatherapy based program.
Minimize driving ≤30 minutes only.
Weeks 5-6:
Progressive strengthening, endurance exercises
NSAID PRN
Education to avoid reinjury
Weeks 6-8:
Advance physical therapy to dynamic lumbar stabilization as tolerated with limited truncal rotation.
Exercise may include swimming, bicycling, and supervised aerobic exercises.
Discontinue use of orthosis.
POTENTIAL COMPLICATIONS AND PITFALLS
Overall, the prevalence of reported complications following intradiscal biacuplasty remains zero. However, complications like discitis, epidural abscess, and bacterial meningitis may occur as the number of the completed procedures increases. Potential complications after any minimally invasive intradiscal procedures can be divided into procedural complications and postprocedural complications.
Procedural Complications
Procedural complications may include:
• Acute paresthesias,
• Muscle spasm, or
• Even bleeding
During the provocative discography excessive amounts of local anesthetic injected deep, close to the disc/foramina, prior to intradiscal needle placement,4 puncturing an intervertebral disc with a needle could potentially lead to progressive disc disruption.19
With the high temperatures used in biacuplasty, electrode placement could lead to nerve injury or osteonecrosis of end plate, causing radicular pain, axial pain, or even transient paralysis. Commonly listed risk factors for postsurgical spinal complications, such as obesity, history of leg pain, smoking, diabetes mellitus, and duration of the back pain, are unlikely to predict higher risk for complications after annuloplasties.
Other possible complications include:
• Radicular signs and symptoms (from burning sensation to foot drop)
• Discitis, septic or aseptic
• Cauda equina syndrome
![]() While never reported after biacuplasty, but has been described following IDET procedure.21–23
While never reported after biacuplasty, but has been described following IDET procedure.21–23
• Postprocedural disc herniation
![]() Also reports as a complication IDET, but not after biacuplasty.4
Also reports as a complication IDET, but not after biacuplasty.4
Up to this date, no complications were reported in the literature on biacuplasty24–26 or by the electrode maker (author’s correspondence).
CLINICAL PEARLS
• More strict selection criteria may improve clinical results of biacuplasty.
• Strong candidates for biacuplasty include patients with evidence of 1 or 2 levels of disc degeneration on MRI and 1 or 2 levels positive on provocative discography.
• The ideal distance between the bipolar electrodes is 2.5 cm to 3 cm or less.
• This optimal positioning is achieved by using an oblique view with the fluoroscopy C-arm rotated to where the superior articular process of the vertebrae 1 level below the disc is ½ the width of the vertebral column.
• Postprocedure rehabilitation program is required to ascertain a good outcome.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






