Introduction
Interstitial cystitis/painful bladder syndrome (IC/PBS) is a condition characterized by pelvic pain, pressure, or discomfort related to the bladder filling, and is typically associated with a persistent urge to void, or urinary frequency, in the absence of infection or other pathology [ 1 ]. The prevalence is 30–300 per 100,000 population; however, this statistic may grossly underestimate the frequency of the disorder given the variability of how IC/PBS is characterized and identified [2].
Because the presenting symptoms of IC/PBS are variable, it is frequently confused with endometriosis (see Chapter 19), recurrent urinary tract infections, overactive bladder, irritable bowel syndrome (see Chapter 21), generalized vulvodynia (GVD) (seeChapter 12), andvestibulodynia (PVD) (see Chapter 8) [3–6]. The female-to-male ratio of people diagnosed with IC/PBS is approximately 10:1 [7].
The etiology of IC/PBS remains incompletely understood, which has resulted in debate as to what characterizes the disorder. It has become clear that IC/PBS is heterogeneous condition with multiple etiologies, the components of which act in combination to cause the symptoms of IC/PBS [8]. It is likely that structural, neurologic, immunologie, genetic, infectious, environmental, dietary, and psychological factors all play a role in IC/PBS.
The most commonly accepted hypothesis of the pathogenesis of IC focuses on an abnormality of bladder mucosal integrity [9]. Normally, the epithelium of the bladder is protected by the glycosaminoglycan (GAG) layer which prevents penetration by ions and toxic substances. If the bladder is subject to repeated insult or injury, the GAG layer can become damaged and more permeable. This increased permeability permits potassium to leak through the bladder mucosa and causes irritation of the underlying nerves, resulting in neurogenic pain and inflammation. Mast cell activation (see Chapter 27) leads to the release of histamine and other inflammatory mediators, increasing pain and tissue damage [10]. There is further degradation of the GAG layer, leading to a vicious cycle of pain and inflammation [11],
It also appears that IC/PBS is similar to other chronic visceral pain syndromes, such as GVD [12]. Substance P, an inflammatory mediator, is found in high concentrations in the bladder mucosa and urine of women with IC/PBS. Substance P stimulates the unmyelinated C-afferent nerve fibers which, in turn, stimulates the dorsal horn of the spinal cord [8]. Persistent activation of the dorsal horn leads to activation of the N-methyl-D-aspartate (NMDA) receptors, resulting in a wind-up phenomenon in which the dorsal horn neurons are disin-hibited. This disinhibition is the pathophysiology underlying allodynia and hyperpathia. Lastly, normally afferent nerves can become efferent, leading to a neurogenic inflammation in the bladder mucosa that perpetuates the pain cycle [8],
The diagnosis of IC/PBS begins with thorough history outlined in Chapter 4. A urinalysis and culture are the initial diagnostic tests in the work-up of IC/PBS. If hematuria is present, urine should be sent for cytology. The physical exam should focus on the abdomen and pelvis, with palpation of the anterior vaginal vault along the course of the urethra, bladder neck, and bladder fundus. The pelvic floor musculature should be examined as thoroughly outlined in Chapter 6.
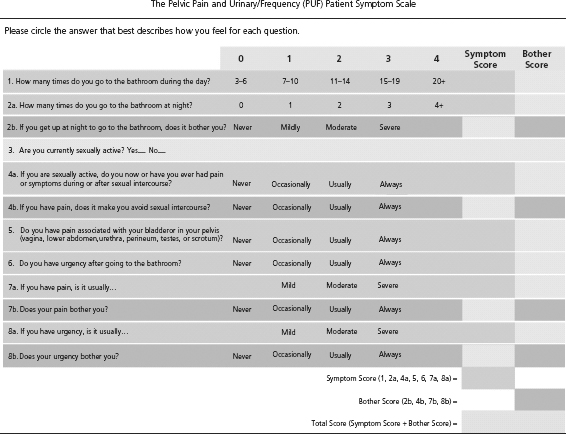
There are several validated scales that can be useful in the diagnosis of IC/PBS. In addition, these scales can quantify the severity of IC/PBS and its impact on sexual function. The Pelvic Pain and Urgency/Frequency Scale (PUF) is a short, self-assessment questionnaire that combines symptom and bother scores [13] (Table 14.1). The symptom score includes the assessment of daytime and nighttime urinary frequency, urinary urgency, pain with sexual activity, andpain location. The bother score quantifies the degree of discomfort related to the variables comprising the symptom score.
The PUF scale has been validated in a large multicenter study, including both urologie and gynecologic patients with chronic pelvic pain (CPP) [13, 14]. Women without IC/PBS generally have PUF scores less than 4. A score of 12–15 is suggestive of IC/PBS, whereas a score greater than 15 is associated with a very strongly likelihood of having IC/PBS. In a study of 334 patients with IC/PBS and 48 controls, 84% of women with PUF scores greater than 15 had a positive potassium sensitivity test (PST; see below). While degree of discomfort is thoroughly assessed and quantified in the PUF questionnaire, bother related to sexual issues is limited to one question on dyspareunia [13].
The O’Leary-Sant Symptom and Problem Index (OSSOI) can differentiate IC/PBS from other urinary disorders. The OSSOI may be used as a screening tool for IC/PBS, but it appears to be most helpful in gauging changes in clinical state over time. The OSSOI does not independently have high enough sensitivity and specificity to warrant its use as the sole diagnostic tool of IC/PBS [ 15 ].
Another multidimensional self-report questionnaire that may be used to assess the impact of IC/PBS on sexual function is the Female Sexual Distress Scale (FSDS) [ 16]. The FSDS is a self-report screening tool shown to be a valid and reliable measure for assessing sexually related personal distress in women. The FSDS consist of 12 items that relate to feelings such as sexual distress, unhappiness, guilt, frustration, stress, inferiority, worry, inadequacy, regretful, embarrassment, dissatisfaction, and anger during the past 30 days. Each item is scored as never (0), rarely (1), occasionally (2), frequently (3), and always (4). Women with high distress associated with their sexual health problem, such as sexual pain, will score high on this measure. Longitudinal scores are useful to assess improvement or worsening of the distress over time [ 16].
A procedure called the PST is useful in the diagnosis of IC/PBS [17]. Initially, sterile saline is instilled through a catheter in an empty bladder. The patient then rates her sensations of urinary frequency and pain. The bladder is then emptied and a solution containing potassium is instilled [18]. Again, the patient rates her symptoms. If she experiences increased pain with the potassium solution, the test is positive, indicating that the diagnosis of IC/PBS is highly likely. A positive PST has been observed in 78% of women with symptoms of IC/PBS but is positive in only 4% of healthy controls [13].
Cystoscopy with hydrodistention is a useful diagnostic tool, but it is not required when making the diagnosis of IC/PBS [19]. Glomerulations (petechial hemorrhages) are found in 95% of women with IC/PBS. Ulcérations of the bladder mucosa (Hunner’s ulcers) are found in only 5–10% of women with IC/PBS [20].
A range of therapeutic interventions, including pharmacologie modalities, are recommendedforthe management of IC/PBS. Initial treatment should include patient education and behavior modification. The practice of keeping voiding diaries detailing the frequency, volume of voided urine, time of urination, and associated symptoms should be encouraged. Recording such information may help to identify foods and behaviors that cause an exacerbation of symptoms.
Given the complexity of IC/PBS, a multifaceted medical treatment regimen is recommended in targeting the various pathophysiologic aspects of the disorder [9]. Current pharmacologie treatment recommendations include several concurrent treatments, each addressing different disease mechanisms. In addition, there is evidence that early recognition and treatment of IC/PBS leads to a more rapid relief of symptoms [21].
Medication to restore the protective barrier between the bladder and urine which counteract dysfunctional epithelium include pentosanpolysulfate sodium (PPS) (Elmiron®) or intravesical heparin (with or without li-docaine) [8]. To date, PPS is the only oral medication approved by U.S. Food and Drug Administration (FDA) for use in the treatment of patients with IC/PBS.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree