INTERFACILITY TRANSPORT AND STABILIZATION
GEORGE A. WOODWARD, MD, MBA AND NICHOLAS TSAROUHAS, MD
PEDIATRIC INTERFACILITY TRANSPORT
Infants, children, and adolescents are commonly evaluated and transported by Emergency Medical Services (EMS) systems worldwide. That discipline of medicine is also termed prehospital care, and the terms are used interchangeably. Chapter 139 Prehospital Care addresses prehospital stabilization and EMS systems. Although there is often overlap in personnel and services between prehospital and interfacility transport, this chapter will focus primarily on interfacility transport medicine and transport stabilization.
Pediatric interfacility transport involves patient transfer from one medical location to another. This aspect of care delivery is vital, especially with the increased regionalization and specialization of our care systems, both in the United States and internationally. Patient status can vary from relatively stable to critically ill. The disease processes involved are detailed throughout this text and include patients with unclear diagnoses, progressively worsening illnesses, traumatic injuries, and medical or surgical processes needing further management. Transport clinicians should be prepared to handle the entire spectrum of ages from very low birth weight, premature neonates through adolescence. Although the ABC (airway, breathing, circulation) approach to care is always vital during interfacility transport, it is essential to understand the disease process and expected progression of the disease during the anticipated transport period. While pediatric transport medicine has been a formally recognized entity for approximately 25 years, it is still developing. A 2013 update, published by Stroud et al., includes the discussion and results of multiple topics from a consensus conference addressing pediatric and neonatal interfacility transport.
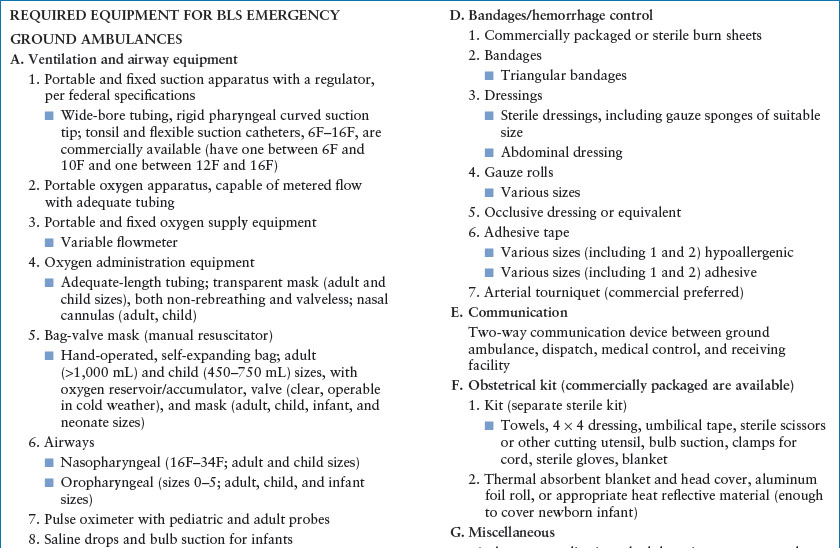
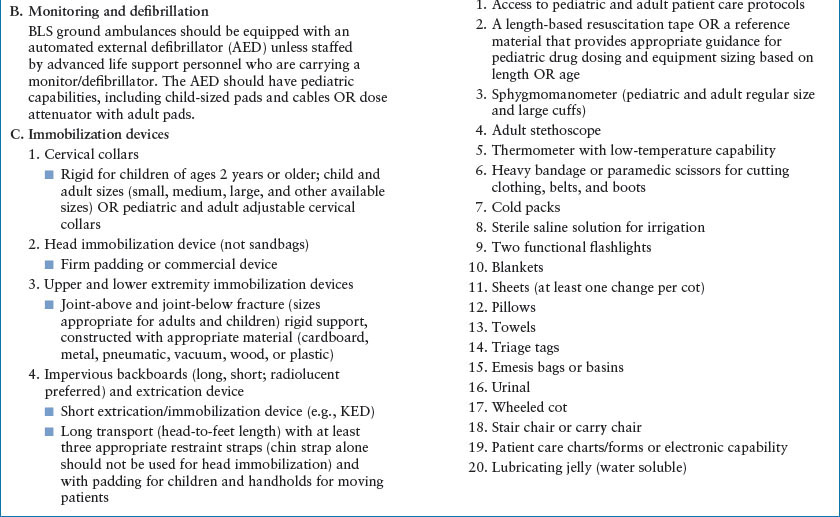
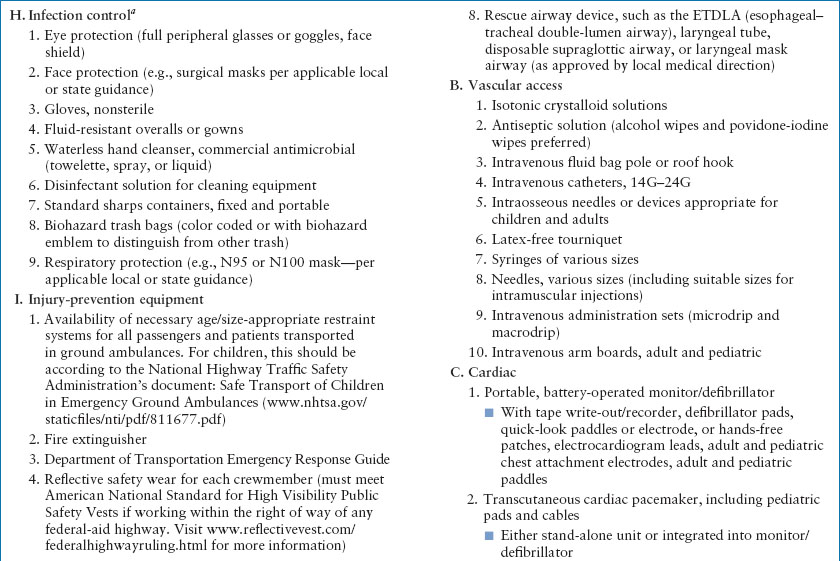
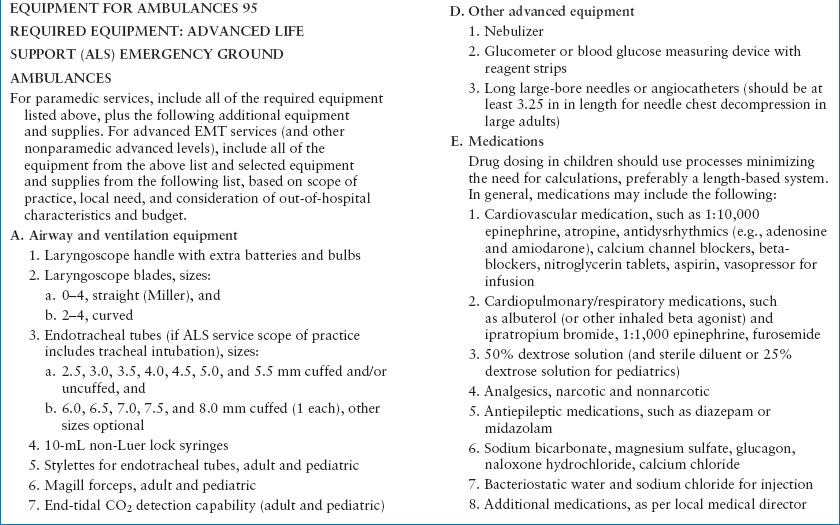
Interfacility transport can originate from hospitals, emergency care centers, physician offices, clinics, or other medical care facilities. There may not always be a clear distinction in scope of practice between interfacility and prehospital transport in terms of equipment, process, and in some instances, personnel. Although transport providers care for patients with disease processes and injuries similar to those seen in emergency departments and critical care units, the environment and delivery of care differs (Figs. 6.1 and 6.2). Interfacility transport teams may also transport patients from the prehospital environment, while EMS may be involved in interfacility transport. Differences between prehospital and interfacility transport teams may include management protocols, extrication issues, personnel types, staff education, and team experience. Table 6.1 summarizes equipment common to both ground EMS and transport ambulances. Lowe’s article describes how interfacility transport services can expand their standard efforts to effectively augment our emergency care responses after mass casualty incidents.
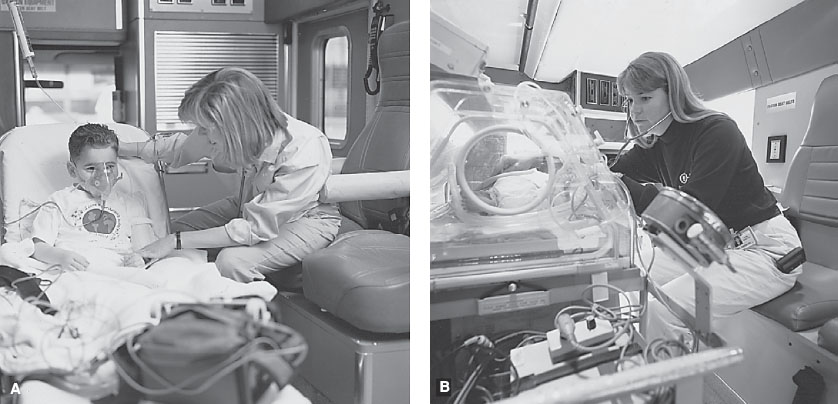
FIGURE 6.1 A, B: Pediatric interfacility ambulance environment. Examples of patients being transported within the ambulance environment. Note relative limitations of space and patient access. (Used with permission, © The Children’s Hospital of Philadelphia, Philadelphia, PA.)

FIGURE 6.2 A–D: Air medical transport environment. A: 1, 2, 3 Examples of patient care area of a twin engine Eurocopter (EC) 135 (A1 and A2) and a single engine Agusta A109E (A3) medical helicopter (“rotor-wing”). (Used with permission, University of Washington Medicine/Airlift Northwest, Seattle Washington. © University of Washington.) B: Example of patient care area of a medical helicopter (“rotor-wing”). (Used with permission, © The Children’s Hospital of Philadelphia, Philadelphia, PA.) C: Patient care area of transport jet. (Used with permission, © The Children’s Hospital of Philadelphia, Philadelphia, PA.) D: Patient care area of transport turboprop plane. (Used with permission, University of Washington Medicine/Airlift Northwest, Seattle Washington. © University of Washington.)
TABLE 6.1
EQUIPMENT FOR GROUND AMBULANCES
Interfacility transport begins with the determination of the need or desire for medical care at another institution. The most common reason for acute interfacility transport is the need for advanced or specialized levels of care or services that are not available at the referring facility. Examples include the need for specialized capabilities (hyperbaric O2), unique facilities (pediatrics, NICU, burn unit), or additional subspecialists (pediatric neurosurgeon). Other reasons for transport may include patient, parent, or provider’s preference for a particular caregiver, location, or institution. This may be due to a desire to obtain a second opinion, but it may sometimes emanate from parent or provider frustration, as well.
Financial considerations, importantly, may not dictate transport decision making for an unstable patient from either the transferring or receiving end. The Consolidated Omnibus Budget Reconciliation Act (COBRA) of 1985, and the federal Emergency Medical Treatment and Active Labor Act (EMTALA) regulations, which were passed as part of COBRA, prevent finance-based emergent transport decisions. Interfacility transport cannot be used by the referring institution as a method to avoid initial assessment, stabilization, or intervention. Similarly, the receiving institution cannot use a patient’s ability to pay to determine transport acceptance; if the receiving institution can provide the higher level of services needed by the patient, the transport should not be declined. To adequately prepare for interfacility critical care transport, a transport system should have access to specialized equipment, trained personnel, and appropriate certifications and licenses. The transport system is responsible for ensuring the safety of the patient, team, and family members during the transport, as well as guaranteeing that the patient is cared for in the appropriate medical environment. The transport system should have identifiable medical and program directors who are responsible for ensuring adequate training and education, as well as continuing competency assessment of personnel and process. The medical and program directors are ultimately responsible for ensuring a safe, reliable transport system.
Significant preparation is required for efficient, quality, and safe transport services. The users of a transport system (the referral hospitals and providers) must ensure the selected transport services meet the standards required for the transfer of their patients. The referral providers must avoid the lure of simply getting the patient out of their initial care environment as quickly as possible. It is incumbent on the referring providers to ensure medical stability to the best of their abilities to ensure the safest possible transport of the patient.
There are several groups who are dedicated to promoting transport safe practice. Transport Medicine has been an established section within the American Academy of Pediatrics (AAP) for 25 years and offers a wealth of transport-related information and education. Other groups, such as the Air Medical Physicians Association (AMPA) and the Association of Air Medical Services (AAMS), are dedicated to ensuring optimal care for transported patients. Transport organizations such as these offer continuing education and are conduits for information regarding Transport Medicine. The AAP published the third edition of its “Guidelines for Air and Ground Transport of Neonatal and Pediatric Patients” in 2007, with the 4th edition scheduled for publication in 2015. A useful pediatric transport Listserv is transmedaap@listserv.aap.org and is available through www.aap.org/sections/transmed/.
Transport Considerations
Familiarity with the transport environment, and the ability to troubleshoot as necessary, is critical for the successful transport of a patient. Therefore, acutely configuring/staffing a transport team in response to an unexpected request for patient transport should be avoided; adequate preparation and training is mandatory. Transport-specific logistic issues to consider include specialized providers with the need for close teamwork and communication, transport durable equipment, ample available medication supplies, unique oxygen delivery and suction setups, the ability to intervene in a cramped mobile environment, the need to safely secure the patient to the stretcher and the stretcher to the transport vehicle, appropriate monitoring in a moving vehicle or aircraft, understanding of inverter power (and how to operate should it be lost), and personnel safety under sometimes challenging transport conditions.
Noise, vibration, and temperature can be formidable problems for the patients and providers alike, if not anticipated. Motion sickness (air and ground) can be quite problematic for non–transport-acclimated personnel. Ideally, transport personnel should be cognizant of their usual and acute capabilities to tolerate the rigors of transport, as this could seriously affect their ability to function optimally.
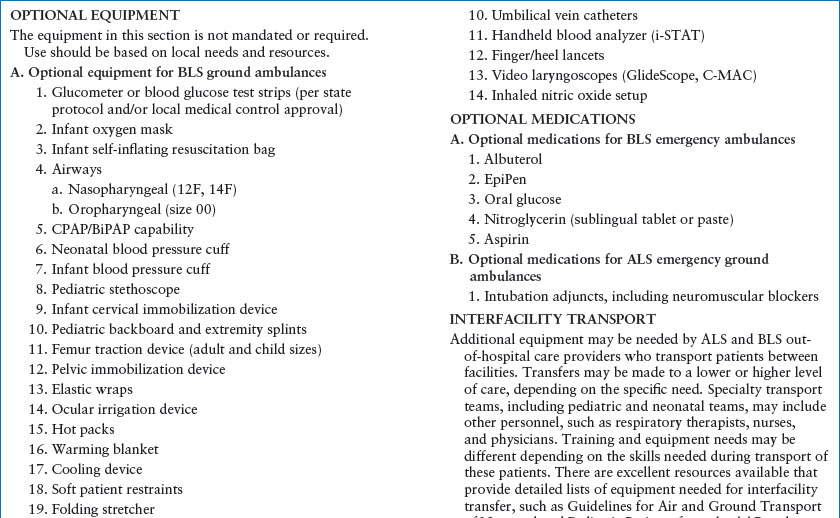
Transport teams should consider the development and use of a pretransport “Safety Checklist.” This tool should be meticulously completed for each transport. It should include a comprehensive review of necessary equipment, medications, oxygen supply, essential demographic information, and other important reminders. All team members should participate in the completion of the safety checklist, and it should be done for all modes of transport. A similar checklist should also be completed prior to departing from the referring institution. Figure 6.3 depicts a sample safety checklist from The Children’s Hospital of Philadelphia.
During the transport process, one must be prepared for all types of patients and complications. When the transport team arrives, the patient’s status may be significantly different than initially described. This can be the result of progression of disease, unexpected change in the patient’s condition, incomplete assessment by the referring physician or transport team, or suboptimal communication between the referring and accepting clinicians. The ability to correctly assess the severity of illness or injury, and then transmit that information to the accepting team, is crucial to facilitate appropriate triage and advice for pretransport care. This process also enables sound decision making regarding the best mode of transport (air or ground), and proper personnel configuration decisions. Orr et al. have presented predictive models to help appropriately triage and critically assess pediatric transport systems. Their research suggests several factors are useful in predicting inhospital mortality for transported patients. These include blood pressure, respiratory rate, oxygen requirement, and altered mental status. They also found that the risk of mortality increases with performance of major interventions, as did the occurrence of unplanned events. Orr et al.’s 2009 paper “Pediatric specialized transport teams are associated with improved outcomes” demonstrates the positive patient impact of specialty pediatric transport teams. Some researchers have looked at the Shock Index (SI) in an attempt to determine stability and level of illness, while others use specific triage tools to determine optimal response required (Advanced Life Support [ALS], level of critical care transport) for each particular patient. Kanter et al. evaluated use of the PRISM score in the pre-ICU populations. Use of electronic adjuncts to care is also increasing; telemedicine interactions prior to and during transport can potentially augment information flow and accessibility, ultimately improving patient care and safety. The transport team may also be asked to transfer a different patient if a more critical patient has presented to the same referring institution. Flexibility in personnel, equipment, and medication availability lead to better outcomes.
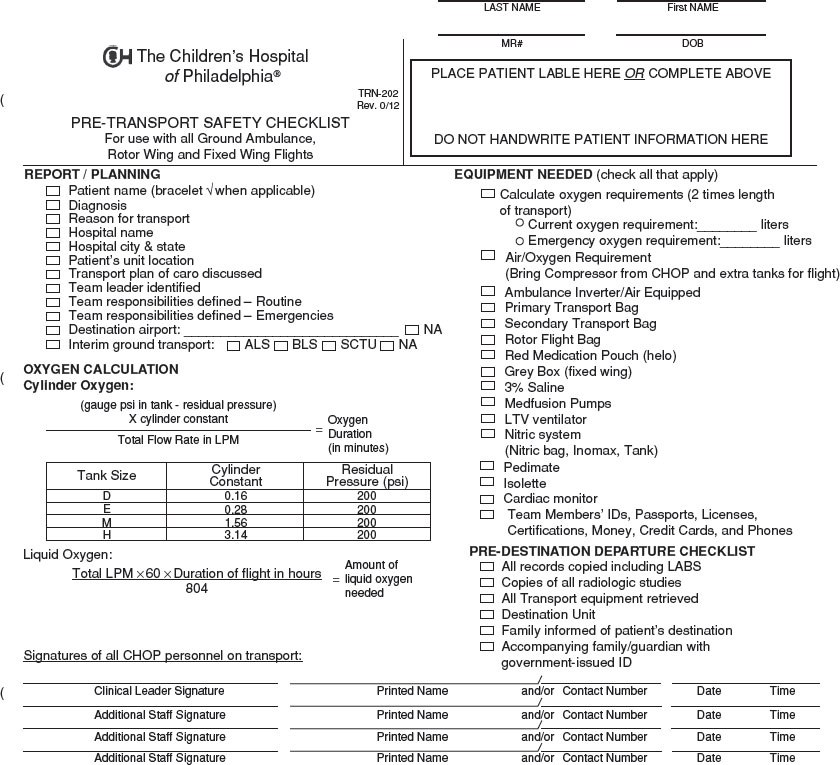
FIGURE 6.3 An example of a pretransport safety checklist. (Used with permission, © The Children’s Hospital of Philadelphia, Philadelphia, PA.)
The medical capabilities of the transport system are important to assess and plan. All transport teams do not have equivalent levels of pediatric skills. Transport services can vary from specialized pediatric teams, such as those supplied by tertiary care pediatric hospitals, to generalized transport services that transport both adults and children. In addition, some teams have additional specialized capabilities, such as the ability to initiate or transport patients requiring extracorporeal membrane oxygenation (ECMO), inhaled nitric oxide, and high-frequency ventilation or oscillation. A generalized transport service might accept all ages and types of patients; unfortunately, there are no universal standards or regulations regarding the level of experience or expertise in pediatrics required to transport pediatric patients. There are, however, accrediting agencies and standards that can be reviewed. The most specific transport accreditation process for transport systems is through the Commission on Accreditation of Medical Transport Systems (CAMTS). Although this is often a voluntary appraisal of a system, certification is mandatory for licensing of some services in specific states. All hospital-based teams should, however, comply with Joint Commission on Accreditation of Healthcare Organizations requirements for patient care and safety. The 2003 National Patient Safety Goals mandate to improve safety of high-alert medications does not exempt transport teams from compliance. The mandate to remove concentrated electrolytes (including, but not limited to, potassium chloride, potassium phosphate, and sodium chloride greater than 0.9%) from patient care units has been a challenge for some transport systems, but must be accomplished for optimal patient safety. Standardizing and limiting concentrated electrolytes in the transport environment is an important patient safety change. Optimally, transport personnel should try to predict the need for specific electrolytes prior to transport, or ensure availability at the referring facility, if they cannot carry or safely prepare specific fluids. For example, management of diabetic ketoacidosis is a process that requires proactive planning for the fluid/electrolyte therapies needed, especially for prolonged transports.
Although different types of transport systems can efficiently and safely transport pediatric patients, the referring physician is responsible for assessing the selected transport system for medical sophistication and safety. As pediatric diseases and processes differ from those in adults, one should not assume a general transport service has adequate experience in pediatrics to offer the appropriate or optimal level of care. In some cases, expedient patient transport by a general team may be perfectly acceptable. For example, the stable trauma patient, the child with a clearly defined medical process, or the patient needing referral for a nonprogressive, non–life-threatening issue, may be adequately transported by a transport team without extensive pediatric experience. Alternatively, however, when the differential diagnosis needs to be explored during the transport process, or when the patient’s condition is rapidly changing, an experienced pediatric team with critical care skills is usually preferred. This process may be classified as bringing pediatric care to the patient, as opposed to getting the patient to pediatric care quickly.
Ideally, advanced pediatric care should begin the moment the transport team is contacted. Pediatric medical or surgical advice, before the arrival of the transport team, can be stabilizing and potentially lifesaving for the patient. Finally, in geographic locations where specialized pediatric transport is unavailable, involvement of skilled acute care/critical care pediatricians on the referring and/or receiving end is extremely important.
Technical skill capability in general transport teams does not necessarily translate into technical skill competence in the treatment of children. This is perhaps most relevant in children needing advanced airway intervention. A child’s anterior larynx, and the recommendation to avoid nasal intubation in children, are complicating factors in successful airway intervention by personnel who are not sufficiently educated or experienced in managing the pediatric airway. Nonpediatric transport services should strive to ensure that they receive the technical skills training necessary for adequate assessment and care of the critical pediatric transport patient.
When a decision is made to transport a pediatric patient, there is often a discussion on the appropriate mode of transport. Nonmedical transports include a parent’s automobile or a taxicab. Problems with those options include lack of assurance of direct transport to the receiving facility, inability to ensure patient safety, and the lack of available medical care during the transfer. Even the accompaniment of a physician or nurse does not markedly improve the ability for medical intervention in these nonmedical vehicles. A Basic Life Support (BLS) ambulance offers direct transportation to the receiving institution, but does not offer much in the way of pediatric expertise or intervention capability. Physician or nurse accompaniment in a BLS ambulance increases potential level of medical care, however the BLS environment is limited with regard to standard personnel, pediatric equipment, and medications. Advanced Life Support (ALS) transport offers more sophisticated resuscitation abilities but may provide variable and inconsistent levels of pediatric experience, expertise, and/or equipment. Addition of a physician or advanced care provider may increase the level of available medical care within the ALS environment, but that impact may be limited by the particular service’s use of protocols and offline medical direction. Critical care transport services can increase the medical sophistication of ALS providers by ensuring the presence of a critical care transport nurse or paramedic, but these providers may be lacking significant pediatric training, experience, expertise, and/or skills. Pediatric critical care transport systems include critical care participants (nurses, physicians, respiratory therapists, nurse practitioners, physician assistants) with significant pediatric experience and expertise.
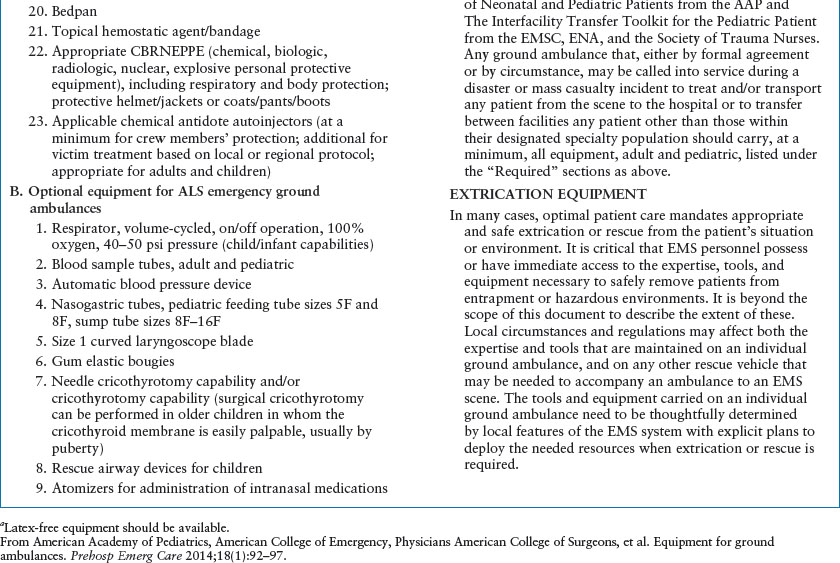
When transport services are needed, the modalities to be considered include ground ambulance, rotor-wing (RW) (helicopter), and fixed-wing (FW) (jet or prop plane) aircraft (Figs. 6.4 and 6.5). Often, the decision is straightforward. For example, the available transport system may be ground only, or inclement weather may prevent air transport. Alternatively, the distance may be so great or traffic issues significant enough that ground ambulance transport is impractical. Several important issues should be considered when mode of transport is discussed. The first is skilled personnel availability. If the transport modes require or offer different personnel configurations, the mode with the most appropriate personnel should be strongly considered. Ideally, a pediatric transport service with the capability for air and ground transport is available, so comparative personnel issues are not the major deciding factor. A choice between speed of transport and appropriate medical personnel can be difficult, although they are not necessarily mutually exclusive. Often, the referral hospitals or physicians want to have a patient taken to the receiving hospital as quickly as possible. They are sometimes willing to accept a transport process with limited pediatric sophistication based solely on speed of transport. Occasionally this may be appropriate, but caution needs to be exercised to ensure the transport system is capable of handling issues that can occur during the transport process. The referral physicians must be proactive in the mode of transport decision. This includes being aware of the transport systems that are available and evaluating those systems before requiring their use. In areas without tertiary care pediatric transport options, local pediatric providers and receiving physicians should be available to provide expertise to the general transport services to help bridge the gap between the general (primarily adult) and pediatric providers.

FIGURE 6.4 Fixed-wing transport aircraft. Both jet and piston (propeller) aircraft are used. (Picture used with permission, Clare McLean, University of Washington Medicine/Airlift Northwest, Seattle Washington. © University of Washington.)

FIGURE 6.5 Rotor-wing transport aircraft (helicopter). (Picture used with permission, Clare McLean, University of Washington Medicine/Airlift Northwest, Seattle Washington. © University of Washington.)
Transport across international borders may also be required. This mode of transport requires significant preplanning. Specific issues to be considered for these patients include language issues of providers (and patients), compatibility and redundancy of medical equipment, power sources, medication issues with customs, communications during transport, visas, passports, other documentation, and logistics of transport durations. For many international, long-distance transports, air crews are required to “time out,” necessitating transport times that may require multiple days, or use of additional personnel for the transport. Similar work rules considerations, although perhaps not as rigid as established Federal Aviation Administration (FAA) crew requirements, should be afforded to the transport healthcare personnel. Options and solutions to these issues are available, but must be anticipated prior to need. Several services specialize in international transports; these services are useful consultants for teams less familiar with international transports. As an example of a subtle nuance important in international transports, if both custodial parents are not accompanying the patient, it may be necessary to have a certified letter from the parent(s) not present, giving the team permission to leave the country.
The disease process must also be considered in mode of transport decisions. The patient with developing petechiae, fever, and hypotension should not be transported several hours by ground if a quicker method of transport is available. Thomas et al. reported an association between helicopter transport and increased survival in blunt trauma patients (adult and pediatric). However, short air transport for a relatively stable patient may not be an appropriate use of resources or be in the patient’s or team’s best interest. Eckstein et al. and Arfken et al. suggested that helicopter services may be overused and may not influence outcomes when compared with alternative modes of transport. One must be cognizant of the many issues surrounding the mode of transport choices; these choices should be individualized for each patient. Although appropriate medical care should not be withheld for financial reasons, a cost comparison of air and ground transports is often useful, and should ideally be accomplished before the need for acute transport. In general, RW (helicopter) transport costs two to three times as much as a ground transport for local transfers. However, the savings may potentially offset the cost in time saved. A helicopter, which can travel directly to and land at the patient’s location, is much quicker than an ambulance, which must take a less direct route. If the helicopter cannot land directly at the referring or receiving center, however, the potential time savings by air transport may be limited. In that situation, in addition to the decreased time savings, the patient may be placed at greater risk due to the multiple transfers involved, as the patient must first be loaded onto a stretcher for an additional ambulance ride to a remote helicopter landing zone, then unloaded from the EMS stretcher to into the helicopter. The riskiest time for the patient is often during transfer from stretcher to stretcher or vehicle to vehicle (Fig. 6.6). These transfers increase opportunities for dislodgement of endotracheal tubes, central venous catheters, chest tubes, and other lifesaving equipment. Communication center personnel, transport team members and medical control (command) physicians should all be aware of times, distances, and particular medical and logistical nuances of each referring institution and location.
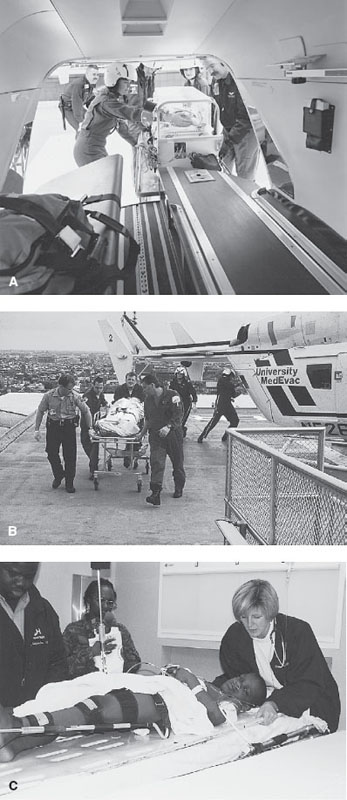
FIGURE 6.6 A–C: Transfer of patient during transport process. Patient transfer between vehicles or stretchers can be risky to the patient. Tube, line, oxygen, or medication disconnection or disruption, as well as shifts in immobilization, must be avoided. (A, C: Used with permission, © The Children’s Hospital of Philadelphia, Philadelphia, PA; B: From Hahnemann University Hospital, University MedEvac, Philadelphia, PA, with permission.)
MEDICAL OVERSIGHT OF EMERGENCY MEDICAL SERVICES
There are two types of medical oversight—direct (online) and indirect (offline). Both models require initial and ongoing input by physicians, and each model has its own risks and benefits. A physician “with experience and knowledge of EMS” (Emergency Medical Services Systems Act of 1973) is required to be involved in the operations of all ALS (and now most BLS) EMS systems (see Chapter 139 Prehospital Care).
Direct Medical Control
Direct medical oversight refers to the real-time provision of supervision or authorization of care activities by a physician using radio or phone, or who is present on scene; this is sometimes referred to as “medical control” or “medical command.” This model enables a clinician to direct care after an assessment is transmitted to them. This may include voice reports and electronic broadcast of data, such as a 12-lead EKG. The benefit of such an arrangement is true customized care, but the drawbacks include additional time spent reporting instead of treating, time demands on medical staff, potential decision making inconsistency within medical control staff, supervision of transport personnel by clinical staff who are not experienced in the transport setting, and technical problems with the communications gear. Although this was once a common model, some transport systems are now trending toward using indirect oversight through the use of standing orders and protocols to standardize care, quality variability, and time requirements associated with direct medical control. Interfacility transport teams often use a combination of care guidelines, orders and protocols (indirect control), with review by predetermined medical control physicians (direct control) at various points of the transport assessment and care.
Indirect Medical Control
Indirect medical control includes the medical management of an EMS/transport system through the use of established care guidelines in place before the call for help arrives. The medical director for a service, who is ultimately responsible for every aspect of patient care, authorizes the personnel to utilize standard protocols for the care of patients in order to save time and reduce the variability of orders. This has the benefit of saving time in critical situations, as well as reducing interoperator variability in patient assessment and medical decision making. In most systems, the option remains for personnel to speak with a clinician for direct medical control, if they have questions, or if the protocol does not clearly apply. This may also be necessary for certain procedures or medications considered to be higher risk to the patient. In EMS, the protocols may be established by the regional or state EMS authority, while in interfacility transport, these are determined by the transporting service, often in conjunction with physician content experts. Medical control physicians should be literate with transport guidelines, protocols, personnel capabilities, medications, and equipment to be able to add the most value in an efficient manner during the transport process.
Team Composition and Models
There are several common models of transport teams across the country. Dedicated pediatric transport teams are often free-standing teams whose primary responsibility is to transport patients. These teams often do not take on direct patient care assignments, though often assist throughout the hospital during their “down-time.” Many dedicated teams transport both neonatal as well as “pediatric” patients, though some teams are exclusively “neonatal or pediatric.” Another model is the “unit-based” team. These teams mobilize team members from clinical units when a transport request is made. For example, a NICU nurse is pulled from a patient assignment to go retrieve a patient for the NICU. Finally, there are some programs that utilize hybrid models of the above. Many types of providers can function effectively as part of a pediatric transport team. Nurses, nurse practitioners, physician assistants, respiratory therapists, EMTs, paramedics, and physicians serve on various transport teams. In general, the personnel chosen for the transport team should have experience in the care of critically ill infants and/or children, and be competent in the transport environment. Excellent bedside clinicians may be less effective in the transport environment if they do not know where to find resources in the ambulance or helicopter, how to turn on the oxygen or suction, or become an additional patient due to motion sickness. The team may not be as capable if one of the providers is limited in knowledge or ability to perform specific patient care tasks, such as medication administration and delivery. The transport environment, especially if constrained by space, may not be the ideal environment to add an additional learner.
The primary mission of the team must be kept in mind when selecting personnel and planning training. For example, a team devoted to neonatal transport should consider team members with experience in the care of critically ill neonates, whereas teams that also perform transports from nonhospital locations may want to employ personnel with prehospital care experience. Teams that have more broad-based missions, such as those that transport both neonates and older children, should attempt to recruit team members from varied hospital areas, including the NICU, PICU, CICU, and Emergency Department. By necessity, such teams have to devote considerable time to the medical cross-training of staff members. However, having team members from varied backgrounds offers the potential for those members to assist in and complement the training and care delivery processes. Regardless of the medical background of the transport participants, pretransport education and experience in the mobile environment is imperative.
Transport team capabilities and types of personnel can vary significantly, depending on the transport system. However, pediatric critical care transport teams, often the optimal interfacility transport configuration for children, usually have several specific types of providers. At the center of most pediatric critical care transport teams are highly trained pediatric critical care transport nurses. These nurses usually have significant critical care and/or emergency medicine experience before becoming members of the transport service. Their technical and cognitive skills are enhanced by additional formal and informal specialized training and experience. Such training may allow them to be classified or credentialed as practitioners with advanced skill certification in certain jurisdictions. Depending on the sophistication of the transport system, training opportunities, skills, and medical licensure issues, transport nurses often provide advanced management for these children. This includes diagnostic and assessment skills, as well as procedural interventions (e.g., advanced airway management, central venous access, pleurocentesis, etc.). In addition to their cognitive and technical skills, transport nurses must serve as experts in the environment in which they practice. The transport nurse should be intimately aware of all operating systems within the transport environment, as well as safety procedures for the patient and the transport team. The medical skills of pediatric transport nurses can often be complemented by the addition of a physician (attending, fellow, or senior resident with prior critical care exposure and experience), nurse practitioner, physician assistant, respiratory therapist, paramedic, or another nurse.
The most common model for neonatal transport teams is one registered nurse and one respiratory therapist. Karlsen et al. found 26 different team configurations in a survey of 335 neonatal transport programs. The second most common model is two nurses. Most experts recommend at least two clinical members on each team, but some one-person teams exist. Other teams routinely utilize three members. Team compositions vary greatly in different systems, and no single team configuration is optimal for all situations. The ideal team composition is one that can address the acute and projected needs of the patient, but also has the flexibility to quickly be revised when necessary.
One also needs to recognize the potential educational value (as compared with service use) of resident trainees in the transport environment. Many pediatric programs include residents and fellows as part of the patient care team; in other cases, they participate primarily an educational role. Durbin et al., as well as Fazio et al., reviewed the use and educational value associated with residents on transport. If residents or fellows are used in more than an educational role, they must bring a skill set to the transport environment that is additive and complementary to the other team members, and equals or exceeds that of those who could take their place. If the resident cannot function as a full member of the team (and has replaced someone who could), reassessment of personnel configurations is indicated.
In addition to the personnel already described, transport teams usually include drivers or pilots who may have no role in providing patient care, or who may assist the other personnel in a limited fashion. Communications specialists may be employed as part of the team’s call receipt and dispatch process. Finally, all transport teams should have a clearly identified supervisory medical director(s) and appropriate medical control physicians who are usually involved with every transport.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







