INJURY: ANKLE
FRANCES TURCOTTE BENEDICT, MD, MPH AND ANGELA C. ANDERSON, MD, FAAP
Approximately 26% of sports-related injuries in school-aged children involve the ankle. It is often difficult for children to localize pain, therefore young children with ankle injuries may complain of pain anywhere from their mid-calf to their toes. Conversely, pathology in the lower leg and foot can cause referred pain to the ankle.
The ankle joint is composed of three bones: The tibia, the fibula, and the talus. The bony prominence of the distal fibula constitutes the lateral malleolus, whereas the prominence of the distal tibia forms the medial malleolus. The physes are located 1 to 2 fingerbreadths above the distal ends of the tibia and the fibula.
The ankle ligaments are attached to the epiphyses. The distal fibular physis is the most commonly injured growth plate in the lower extremities. It is second only to the distal radius in the incidence of physeal injuries.
Growth plates and bones are weaker than ligaments. Consequently, ankle trauma in preadolescent children is much more likely to cause fractures of the physis and the adjacent epiphysis and/or metaphysis than ligamentous injuries or sprains.
DIFFERENTIAL DIAGNOSIS
A number of traumatic injuries may cause ankle pain (Table 35.1). Although trauma is the most common cause of ankle pain in children, infectious, rheumatologic, inflammatory, neoplastic, and hematologic abnormalities also should be considered (Table 35.2) because trauma may occasionally merely exacerbate pain in children with underlying conditions. Again, keep in mind that a complaint of ankle pain may result from a lesion anywhere between the knee and the toe, particularly in preverbal children. The most common injuries vary according to age (Table 35.3).
ANKLE FRACTURES
Fractures of the ankle account for 5.5% of all fractures in pediatrics. The system used to classify ankle fractures in children differs from the one used in adults because of the presence of growth plates and the possible implications of physeal injuries. The Salter–Harris (S-H) classification is most commonly applied, as described in Chapter 119 Musculoskeletal Trauma.
Inversion ankle injuries in preadolescents most commonly cause a S-H type I fracture of the distal fibula (Fig. 35.1). Clinically, the patient presents with swelling about the lateral malleolus and tenderness at the distal fibular physis. Fractures confined to the physes may not be visible on radiographs. Consequently, routine radiographs may appear normal despite the presence of a fracture.
In severe inversion injuries, the distal fibular fracture described previously may be accompanied by a fracture of the medial malleolus (Fig. 35.2). This medial malleolus fracture is usually a S-H type III or IV fracture of the distal tibia. These patients will have tenderness at the medial malleolus and the distal fibular physis.
Fractures resulting from eversion of the ankle are usually a combination of a S-H type II fracture of the lateral tibia and a transverse fracture of the fibula (Fig. 35.3). The fibular fracture is relatively high (4 to 7 cm above the fibular physis). Therefore, it is important to examine the full length of the fibula in patients with ankle injuries.
Direct axial compression of the ankle is uncommon but can cause a S-H type V injury to the distal tibia.
External rotation injuries are responsible for lesions known as transitional fractures. Transitional fractures occur during adolescence when closure of the growth plates is beginning. Closure of the distal tibial physis starts centrally and then spreads medially, posteriorly, and finally laterally. The distal tibial physis closes before the distal fibular physis. As skeletal maturity (and physeal closure) progresses, the relative strengths of various parts of the tibia change. As a result, the same mechanism of injury may cause very different fracture patterns, depending on the age of the patient. The juvenile Tillaux fracture and the triplane fractures are examples of transitional fractures.
In the juvenile Tillaux fracture, a fragment of bone is torn off the lateral border of the tibia by the anterior tibiofibular ligament (Fig. 35.4). It is a S-H type III injury of the distal tibia. This fracture is seen almost exclusively in patients between the ages of 12 and 14 years. This is because the closure of the medial aspect of the distal tibial physis begins around 12 to 14 years of age, whereas the lateral aspect remains open and therefore less stable for approximately another 18 months. The greater the skeletal maturity of the patient, the more lateral the epiphyseal fracture line occurs.
Diagnosis of a juvenile Tillaux fracture may be difficult because routine radiographs may not show the fracture line well. If displacement is minimal, the only radiographic sign may be a slight widening of the lateral tibial physis or a faint vertical fracture line through the epiphysis on anteroposterior (AP) or oblique views. In some cases, the only finding may be local tenderness in the area of the lateral tibial physis. Multiple oblique views, or computed tomography (CT), may be needed to adequately delineate the extent of the fracture.
Growth arrest and angular deformity are rare because these fractures occur at the time of physeal closure. However, ankle joint arthritis may complicate the long-term outcome if the diagnosis is missed or if reduction is inadequate.
Triplanar fractures are characterized by a fracture line that runs in three planes: Coronal, sagittal, and transverse. Two types of triplane fractures have been described. The first is a three-fragment fracture (Fig. 35.5). The first fragment is the same as the one found in the juvenile Tillaux fracture—a fragment of the epiphysis torn off the anterolateral quadrant of the tibia. The second fragment is the remaining medial part of the epiphysis, which is attached to a posterior spike of the metaphyseal bone. The third fragment is the tibial shaft.
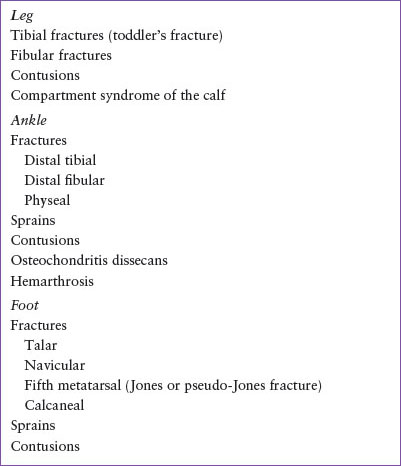
TABLE 35.1
DIFFERENTIAL DIAGNOSIS OF TRAUMATIC INJURIES THAT CAUSE ANKLE PAIN
A two-fragment fracture has also been described. The first fragment is again the lateral tibial epiphysis, but it is attached to a posterior spike of the metaphyseal bone. The second fragment is the remaining medial epiphysis and is attached to the tibial shaft (Fig. 35.6).
On a radiograph, triplanar fractures have the appearance of a S-H type III fracture on the AP view and a S-H type II fracture on the lateral view. If only the AP view is obtained, it may be difficult to distinguish these fractures from the juvenile Tillaux fracture. The key to diagnosis is the posterior metaphyseal spike seen on the lateral film.
ANKLE SPRAINS
Ankle sprains in children or preadolescents are less common than fractures because the ligaments in this age group are much stronger than growth plates or even bone. If a ligamentous injury occurs in a child with an open growth plate, an associated avulsion fracture is almost always present. However, once skeletal maturity is reached, ankle sprains become the most common of sports injuries.
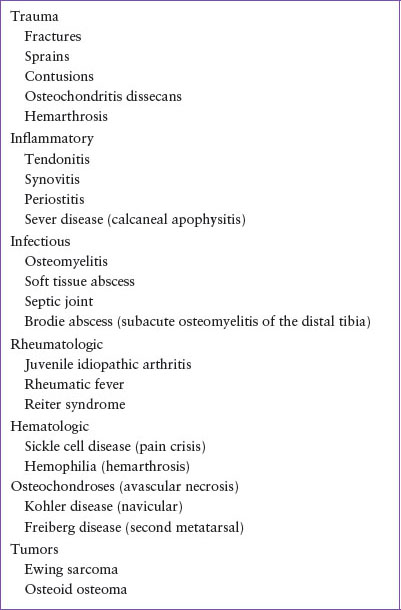
TABLE 35.2
DIFFERENTIAL DIAGNOSIS OF ANKLE PAIN
Inversion injuries cause 85% of ankle sprains. The most commonly injured structures are the lateral ligaments. Three lateral ligaments support the ankle joint: The anterior talofibular (ATFL), the calcaneofibular (CFL), and the posterior talofibular (PTFL) (Fig. 35.7). The ATFL is the weakest and most commonly injured of the three. The CFL is intermediate in strength and is rarely injured without an associated tear of the ATFL. The PTFL is the strongest and least injured of the lateral ligaments. Because its fibers run horizontally, only extreme dorsiflexion will stress this ligament. The peroneus brevis tendon also traverses the lateral aspect of the ankle joint and can be injured by inversion stress. It inserts at the base of the fifth metatarsal.
TABLE 35.3
COMMON INJURIES ASSOCIATED WITH ANKLE PAIN ACCORDING TO AGE
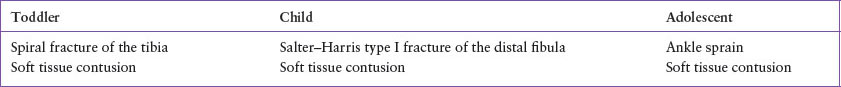
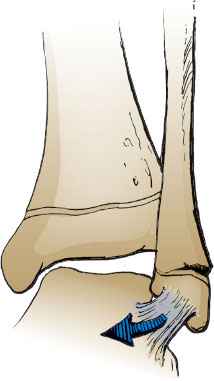
FIGURE 35.1 Inversion injury.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







