INTRODUCTION
Musculoskeletal trauma involves injury to one or more of the following structures:
Bone: A unit of the skeleton composed of the hardest variety of connective tissue. Bones give shape and support to the body. In addition to surrounding and protecting vital organs, they serve as points of attachment for the muscles of the limbs, making movement possible.
Joint: The area where two or more bones articulate with one another. Joints are usually classified in terms of the amount of motion permitted at the articulation. Most joints of the extremities are synovial joints, which allow the greatest amount of motion.
Ligament: A bundle of connective tissue forming part of the fibrous capsule surrounding a joint and attached to it. Every joint of the extremities is reinforced by two or more ligaments, whose purpose is to stabilize the joint by confining its movements to specific planes and preventing movement beyond physiologic limits.
Tendon: The fibrous structure connecting a voluntary muscle to bone, cartilage, or ligaments. Tendons enable muscles to effect motion in the joint or body area to which they are attached.
Orthopedic injuries to these structures include the following:
Fracture: A disruption of bone tissue. Fractures may be caused by: (1) an application of force exceeding the strength of the bone, (2) repetitive stress, or (3) an invasive process that undermines the bone’s integrity.
Dislocation: Complete disruption of a joint, such that the articular surfaces of the bones that comprise the joint are no longer in contact with one another.
Subluxation: Partial disruption of a joint, in which some degree of contact between the articular surfaces remains.
Fracture-dislocation or fracture-subluxation: Disruption of a joint combined with fracture of at least one of the bones involved in the articulation.
Strain: A tearing injury to muscle fibers resulting from excessive tension or overuse.
Sprain: A tearing injury to one or more ligaments of a joint, which occurs when the joint is forced beyond the limits of its normal planes of motion.
PATHOPHYSIOLOGY OF FRACTURES
Properly assessing and treating bony injuries in the ED requires an understanding of the physiologic processes by which fractures are created and by which they heal. Practical knowledge of fracture pathophysiology may provide the index of suspicion needed to diagnose an injury that might otherwise be missed. It also may help prevent or minimize complications and sometimes may form the basis for advising the patient regarding the outlook for recovery of function.
Although fractures are sometimes classified in terms of the mechanism that created them, they also may be described in terms of the physiology involved.
Most fractures are the result of significant trauma to healthy bone. The bony cortex may be disrupted by a variety of forces, including a direct blow, axial loading, angular (bending) forces, torque (twisting stress), or a combination of these.
Fractures that result from relatively minor trauma to diseased or otherwise abnormal bone are termed pathologic fractures. In such cases, a preexisting process has weakened the bone and rendered it susceptible to fracture by forces that, under normal circumstances, would not disrupt the cortex. Common examples of such injuries are fractures through metastatic lesions, fractures through benign bone cysts, and vertebral compression fractures in patients with advanced osteoporosis. Numerous other disease processes may render an individual susceptible to pathologic fracture. Because these injuries often are not associated with a history of significant trauma, subtle pathologic fractures may go undetected unless there is a clinical index of suspicion.
Bone may undergo a “fatigue” fracture by being subjected to repetitive forces before the bone and its supporting tissues have had adequate time to accommodate to such forces. An example is a metatarsal shaft fracture in unconditioned foot soldiers (“march fracture“). Radiographs often are negative early in the clinical course of stress fractures. The initial diagnosis may be presumptive, based solely on the history and findings of point tenderness or localized swelling. Days or weeks may pass before the fracture line or new bone formation becomes visible radiographically.
Fractures involving the physis, the cartilaginous epiphyseal plate near the ends of the long bones of growing children, were originally classified by Salter and Harris1 and are commonly called Salter fractures. New bony material needed for the elongation of bones during growth is provided by specialized cells within the physis. When growth is completed, the physis transforms from cartilage into bone, ultimately fusing with the bone surrounding it, and disappearing as a distinct entity. By definition, Salter fractures cannot occur in fully grown adults.
Damage to the epiphyseal plate during a child’s growth may destroy part or all of its ability to produce new bone substance, resulting in aborted or deformed growth of the limb. The potential for growth disturbance from an epiphyseal plate injury is related to the number of years the child has yet to grow (the older the child, the less time remains for deformity to develop) and to the pattern of the fracture line through the epiphyseal area. Classification of Salter fractures and their clinical implications are discussed in the section Describing Radiographs in this chapter.
An understanding of the short- and long-term aspects of bone healing helps decision making regarding fracture reduction, treatment modality, and the prognosis for regaining function or being left with residual deformity. Fracture healing consists of three phases: inflammatory, reparative, and remodeling, each of which blends into the next, with some degree of overlap between them.2 When a fracture occurs, the microvessels crossing the fracture line are severed, depriving the damaged bone ends of their blood supply. As a result, the bone ends gradually necrose, triggering a classic inflammatory response in which neutrophils, macrophages, and lymphocytes migrate to the area. The proteins and peptides (collectively termed cytokines) released by these cells promote revascularization.3 This early phase is brief but creates the tissue environment for the most predominant aspect of fracture healing, the reparative phase.
Granulation tissue soon begins to infiltrate the area.4 Within the granulation tissue are specialized cells capable of forming collagen, cartilage, and bone—the ingredients of callus. Callus gradually surrounds the fractured ends and stabilizes them, becoming more densely mineralized with time.
Meanwhile, the necrotic edges of the fragments are removed by osteoclasts, cells whose function is to resorb bone. That is why some “hairline” fractures do not appear on a radiograph until days after injury. Invisible initially, the diagnostic fracture line appears only after necrotic bone has been resorbed from the area.
The final phase of bone healing, the remodeling phase, is the longest, sometimes lasting years. Remodeling is the tendency of bone gradually to regain its original shape and contour. During this phase, superfluous portions of callus are resorbed, and new bone is laid down along the natural lines of stress. These layers, easily visible on radiographs of normal bone, are the bony trabeculae. The formation of trabecular bone is a physiologically efficient process providing maximum strength relative to the amount of bone material used.
The anticipated degree of remodeling after a fracture is related to a number of factors. Predictors of satisfactory remodeling include youth, proximity of the fracture to the end of the bone (but not involving the epiphyseal plate), the amount of angulation, and the extent to which the direction of angulation coincides with the plane of natural joint motion.
Clinical decisions regarding the aggressiveness of fracture reduction are directly linked to knowledge of bone-healing physiology. Some angulation near the end of a long bone, for example, may be more accepTable than the same amount of angulation near the midshaft. In the wrist, dorsal or volar angulation has a better prognosis than does ulnar or radial angulation because the natural plane of wrist motion is dorsal to volar. Mild angulation in a 2-year-old child may be left to remodel on its own, whereas the same amount of angulation in an adult may require correction.
ORTHOPEDIC EMERGENCIES
An open fracture is a fracture associated with overlying soft tissue injury, creating communication between the fracture site and the skin. Although this term may convey the image of grossly exposed bone, the term is equally applicable to any puncture wound extending to the depth of an underlying fracture. Such puncture wounds may be created by external forces or may occur from within, when a sharp bone fragment transiently protrudes through the skin before receding back beneath the surface.
A potential major complication of open fracture is osteomyelitis. Once established, osteomyelitis may result in months or years of pain, disability, medical therapy, surgical procedures, and, in some cases, amputation. Although osteomyelitis may sometimes be unavoidable, it is less likely when treatment is prompt and meticulous.
Open fractures are usually classified by their severity, based on the extent of overlying tissue disruption, lack of bone coverage, kinetic energy of the injuring force, and evidence or likelihood of significant contamination. Irrespective of these factors, any open fracture should be promptly and carefully treated.
Subluxation is a condition in which the articular surfaces of a joint are nonconcentric to any degree. Dislocation is the most extreme form of subluxation. A joint is dislocated when the articular surfaces of the bones that normally meet at the joint are completely out of contact with one another. The urgency of reducing a dislocation is based on several factors. One is the potential for neurologic or circulatory compromise. The neurovascular bundle passing close to the affected joint may become “kinked” around the dislocation. This may result in neurologic or vascular deficit that might be temporary if the deformity is reduced promptly but irreversible if treatment is delayed. Another consideration is that the longer a joint has been dislocated, the more difficult it may be to reduce and the less sTable the reduction is likely to be. This is probably due, at least in part, to edema, muscle spasm, and other tissue changes that increase over time.
Dislocation of the hip also carries the potential for avascular necrosis of the femoral head. The necrosis occurs because much of the blood supply to the femoral head is delivered through vessels that emerge from the acetabulum. When the joint is dislocated, circulation to the femoral head is disrupted. At some point, the vascular insult becomes irreversible, and bony necrosis results. Although aseptic necrosis may occur despite the clinician’s best efforts, its likelihood increases with the delay until reduction.
Any injury associated with neurologic or vascular compromise should be addressed as soon as possible. The longer such a deficit goes untreated, the longer it is likely to persist and the greater the possibility that it will be irreversible. In some cases, reducing a deformity by means of longitudinal traction is all that is necessary to restore circulation or nerve function.
PREHOSPITAL CARE
Effective splinting of an injured extremity is important for several reasons: (1) it reduces pain, (2) it reduces damage to nerves and vessels by preventing them from being compressed between the fracture fragments or being stretched by angulation at the fracture site, (3) it reduces the chance of inadvertently converting a closed fracture to an open one should a sharp bone fragment poke its way through the skin, and (4) it reduces the pain associated with patient transport by minimizing motion of the fracture fragments.
Many splinting modalities are available to EMS personnel. These may range from sophisticated devices, such as vacuum splints containing small beads that conform to the extremity when air is removed, to simpler techniques such as cardboard or pillow splints, or padded IV boards.
For injuries of the wrist or forearm, consider using a sling to supplement the splint, because optimal immobilization includes the joint above and the joint below the fracture, and a sling helps keep the elbow at rest.
For suspected injuries to the shoulder, humerus, or elbow, a sling-and-swathe arrangement works well. This method involves applying a sling, then binding the affected arm to the thorax with a gauze wrap. An exception to this principle is immobilization of patients with suspected anterior dislocation of the shoulder. Many patients with this injury have difficulty adducting the forearm, and forcibly binding it to the thorax may be painful. A simple sling is adequate in such cases. Injuries to the ankle may be immobilized in a pillow or well-padded cardboard splint. If a fracture of the tibial shaft or knee is suspected, the device should extend well above the knee to immobilize the joint above and the joint below the fracture.
Some injuries warrant special splints, such as a winch-mechanism traction apparatus for femoral shaft fractures. Although such a device does not immobilize the hip (the joint above the fracture), the traction component makes this unnecessary. If a traction device is not available, then both the hip and knee should be immobilized. One method of accomplishing this is to bind the legs together, then bind the patient to a backboard from ankles to thorax with folded sheets or towels beneath the lower legs (but not the feet) to ease pressure on the heels.
Other types of splints exist, but their use is controversial. InflaTable plastic splints, for example, may be used for injuries to the ankle or wrist but sometimes are used inappropriately for fracture of the humerus or femur. Because these devices normally do not extend sufficiently proximally, they provide inadequate immobilization for such injuries. Also, overinflating the device may impair circulation. If the inflaTable splint cannot be dented by moderate thumb pressure, it is probably overinflated. InflaTable splints should not be applied over clothing, because wrinkles in the clothing may cause pressure sores in swollen and vulnerable tissue.
Also controversial are nonmalleable aluminum splints, because they are based on the “one size fits all” principle, which some clinicians interpret as “this size fits none.” Malleable aluminum splints are preferable, as they can be made to conform more closely to the contour of the extremity, even accommodating some degree of deformity. If used, aluminum splints of either type should be well padded, because their hard surface may cause pressure sores. Like any splint, they should immobilize the joint above and the joint below the fracture when used for long-bone injuries. For example, an above-knee splint is indicated for suspected fracture of the tibial shaft. Aluminum splints should be removed promptly once a fracture is diagnosed or ruled out. If a fracture is confirmed, replace the splint with an alternative immobilization dressing before the patient leaves the ED, because aluminum splints may cause pressure sores even when padded.
Another controversial device is military antishock trousers. This device may be used during ambulance transport of patients with already diagnosed pelvic ring fracture, or for patients with a clinically apparent femoral fracture when a traction device is not at hand, as the device immobilizes the joints above and below the fracture. Some EMS systems also advocate its use for patients with bilateral femur fractures even when traction is available, because of the anatomic difficulty of applying two traction splints. However, military antishock trousers are cumbersome to apply, their efficacy is not firmly established, and they can possibly contribute to compartment syndrome, fluid and electrolyte imbalance, and circulatory impairment.5,6
Many EMS programs do not recommend prehospital reduction of deformity for an injured extremity, as injudicious manipulation may convert a pure dislocation to a fracture-dislocation. Even if a fracture had already existed, there would be no way to prove it was not caused by the manipulation. One circumstance in which prehospital reduction of obvious fracture to the shaft of a long bone may be justified is a nonpalpable distal pulse. In the absence of a common standard, the indications for reduction of deformity by prehospital personnel remain at the discretion of the supervising EMS program.
CLINICAL FEATURES
The importance of a careful history and physical examination cannot be overstated. Orthopedic diagnosis is sometimes thought of as being as simple as taking a radiograph of the painful area. Although imaging is an important adjunct, it is not the ultimate diagnostic resource. The pain of a fracture or a dislocation may be referred to another area. For example, patients with disruption of the sternoclavicular joint or fracture of the humeral shaft may complain only of shoulder pain. If the radiograph is based solely on where the patient reports discomfort, then the injured part might not be included on the film. Imaging decisions should be based not only on the chief complaint, but also on systematic palpation, observation of subtle deformity or significant point tenderness, and mechanism of injury.
Some fractures or dislocations may be demonstrated only by special radiographic views, which are not part of the standard series for that body part. Such views will never be ordered unless the clinician has already formulated a presumptive diagnosis based on the history and physical findings.
Some injuries might not be radiographically apparent on the first day, regardless of what views are taken. Common examples are fracture of the scaphoid, nondisplaced fracture of the radial head, and stress fracture of a metatarsal. The classic radiographic signs accompanying these injuries, such as the fat-pad sign of the elbow, are not always conveniently present, but mechanism, history, and findings suggesting the injury often are. CT or MRI may allow early diagnosis of fractures that are not radiographically evident. However, such tests are not always available or feasible on the day of injury. In such cases, the diagnosis of fracture may be purely clinical until 7 to 10 days post-trauma, when enough bony resorption has occurred at the fracture site to reveal a lucency on plain radiographs.
The value of the history in cases of orthopedic trauma is often underestimated. Knowing the precise mechanism of injury may be the key to diagnosing some fractures or dislocations. For example, a history of shoulder injury combined with the complaint of dysphagia may be the only clue to the existence of posterior sternoclavicular dislocation. This entity, which causes pressure on mediastinal structures, often can be demonstrated only by CT and may result in severe complications if treatment is delayed. Table 267-1 provides other examples of mechanisms that may lead the clinician to suspect, or presumptively treat for, specific injuries. This is by no means a definitive or exhaustive list. Some of the mechanisms described may produce injuries other than those mentioned. Conversely, the injuries may be produced by mechanisms in addition to those listed.
| Mechanism | Possible Injury |
|---|---|
| Bilateral compression of the shoulders | Anterior or posterior sternoclavicular dislocation |
| Direct blow to the medial clavicle | Posterior sternoclavicular dislocation |
| Fall, landing on the apex of the shoulder | Acromioclavicular separation |
| Direct blow to the anterior shoulder, fall on the outstretched arm, seizure or electroconvulsive muscular activity | Posterior dislocation of the shoulder |
| Sudden traction force to a toddler’s arm | Subluxed radial head (sometimes misdiagnosed as brachial plexus injury because of pseudoparalysis of the arm) |
| Fall, landing on the outstretched arm or with the elbow beneath the body | Fracture of the radial head (may be occult on initial x-ray) |
| Forced dorsiflexion of the wrist | Fracture of the scaphoid, lunate dislocation, perilunar dislocation, Colles fracture |
| Striking the knee against the dashboard in a high-speed collision | Posterior dislocation of the hip |
| Landing flat on the feet from a height | Calcaneus fracture; tibial plateau fracture; acetabular fracture; vertebral compression fracture, usually lumbar |
| Ankle inversion force | Fracture of any of the three malleoli, fracture of the base of the fifth metatarsal |
| Rotatory ankle force | Fracture of any of the three malleoli, disruption of the anterior tibiofibular ligament with proximal fibular fracture (Maisonneuve’s injury) |
| Inversion or medial or lateral stress to the forefoot; axial load on the metatarsal heads with the ankle plantarflexed | Midfoot dislocation (Lisfranc’s injury) |
Some musculoskeletal injuries or conditions may not necessarily be associated with a history of direct trauma. Occult fracture of the hip in an osteoporotic individual, occult stress fracture of a metatarsal in someone who has recently done an unusual amount of walking, and slipped capital femoral epiphysis in a preteenager or young adolescent are examples of injuries in which symptoms may be gradual and insidious in onset, unrelated to an isolated traumatic event. Exquisite tenderness to palpation or pain on weightbearing or passive range of motion suggests the possibility of an occult or easily missed fracture. Depending on the index of suspicion, further studies, such as a bone scan or MRI, may be indicated to exclude significant pathologic conditions before the patient is allowed to resume weightbearing.
History taking should not necessarily be limited to orthopedic issues. Depending on the situation, a general medical history should be obtained because it may have implications for further workup, the potential for complications, or ultimate prognosis for recovery of function. Relevant issues may include a history of heart disease or neurologic disease, taking anticoagulant medication, falling due to syncope or transient hemiparesis, or an unsteady baseline gait that cannot withstand further impairment.
Essential components of the examination for musculoskeletal trauma are (1) inspection for swelling, discoloration, or deformity; (2) assessment of active and passive range of motion of the joints proximal and distal to the injury; (3) palpation for tenderness or deformity; and (4) assessment of neurovascular status.
Gross deformity along the shaft of a long bone is pathognomonic for fracture. Deformity at a joint, loss of range of motion, and severe pain at rest suggest the presence of a dislocation or fracture near the joint. An exception is posterior dislocation of the shoulder, which, although intensely painful, might not be accompanied by obvious deformity, although the humeral head may be palpable posteriorly.
When gross deformity is not present, presumptive diagnosis strongly depends on findings noted on palpation. Palpation may disclose areas of bony step-off and the precise location of point tenderness.
The palpation examination should be done systematically and consistently from one patient to the next. The area palpated should extend well beyond the location of pain described by the patient, as the pain may be referred. For example, when an injured patient complains of shoulder pain, palpation should begin at the sternoclavicular joint, then proceed along the clavicle onto the acromioclavicular joint, then onto the humeral head and along the entire humeral shaft. In addition, the scapula should be palpated for tenderness, and the posterior aspect of the shoulder should be palpated for any unnatural prominence or fullness that might suggest posterior dislocation of the humeral head. Injury to any of these areas may be reported by the patient as “pain in the shoulder.” Only a meticulous palpation examination may protect the clinician from being misled by referred pain and missing a crucial diagnosis.
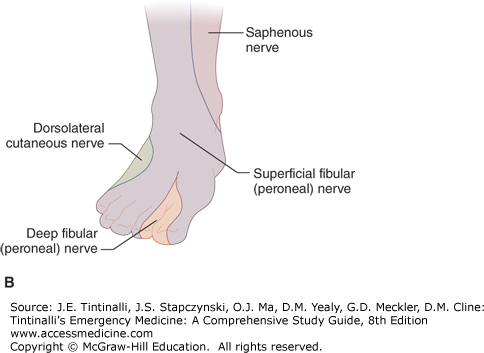
When injury involves an extremity, as opposed to the vertebral column, sensorimotor testing should be performed on the basis of peripheral nerve function, rather than nerve root and dermatomal distribution (Figure 267-1). In the upper extremity, the radial, median, and ulnar nerves should be tested. When the shoulder is anteriorly dislocated, two additional nerves, the axillary (supplying sensation to the lateral aspect of the shoulder) and the musculocutaneous (supplying sensation to the extensor aspect of the forearm), also should be checked. In the lower extremity, examination of the saphenous (sensory only), peroneal, and tibial nerves should be performed. Neurologic deficit is important to document early, particularly before the patient has undergone any significant manipulation or reduction maneuvers.
Assess vascular status early. The sooner circulatory compromise is identified and addressed, the better the chance of avoiding tissue ischemia or necrosis. Injuries such as dislocation of the knee (tibiofemoral joint), fracture-dislocation of the ankle, and displaced supracondylar fracture of the elbow in children may be associated with vascular disruption, with resulting circulatory impairment.
DIAGNOSIS
The joints above and below a fracture should generally be imaged because injury at the proximal or distal joint may coexist with long-bone fractures. Injuries that may require special views or advanced imaging modalities in order to be visualized include acromioclavicular separation, fracture of the scaphoid, posterior shoulder dislocation, and sternoclavicular dislocation.
The use of bedside US has been reported for pediatric clavicle and forearm fractures and long-bone fractures. However, US for these purposes is operator dependent and has not replaced traditional diagnostic imaging.7,8,9,10
Children who have sustained trauma at or near a joint may need comparison studies of the opposite extremity to differentiate fracture lines from normal epiphyseal plates or ossifying growth centers. This is particularly true of the pediatric elbow, which typically exhibits six ossification centers sequentially as the child grows.
Although the clinician may be tempted to base diagnostic and treatment decisions on the radiologist’s report, this is not advisable for at least two reasons. First, a negative radiologic report does not exclude significant injury. Fracture of the radial head, scaphoid, or metatarsal shaft, for example, may be undetecTable on radiographs initially, even when special views are taken. Second, the terminology used by radiologists to describe malposition of fracture fragments or disrupted joints often differs from the terminology used by orthopedists. Because the emergency physician may confer with an orthopedist regarding the initial management of a patient, and because this interaction commonly involves describing the radiographic appearance of an injury, it is important that the two physicians “speak the same language.”
As more hospitals convert from film-based to digital imaging, orthopedic consultants are increasingly likely to be able to examine a patient’s imaging studies by remote access. In the absence of such technology, proper management of the patient may depend on the emergency physician’s ability to convey the radiographic appearance of the injury to the consultant. In such cases, the narrative often will influence the orthopedist’s decision regarding the need for hospital admission and whether surgical versus nonsurgical management is warranted. In essence, the emergency physician should be able to transmit a virtual copy of the radiograph by means of verbal description.
There are a number of ways to characterize the appearance of fractures. The method presented below is intended to be the most practical from the standpoint of communicating with an orthopedic consultant.
Although not a radiologic finding per se, whether a bony injury is open or closed is an important consideration and should be conveyed to the orthopedist at the outset. The implications of open fracture are of such significance that this factor alone may determine the patient’s immediate care or ultimate disposition.
Typical reference points used by orthopedists to describe the location of a fracture along the shaft of a long bone are the midshaft, the junction of the proximal and middle thirds, and the junction of the middle and distal thirds. Any fracture more proximal or distal than these locations may be described in terms of its distance, in centimeters, from the bone end.
When a fracture extends into the adjacent joint, it is termed intra-articular. Intra-articular fractures have special significance because disruption of the joint surface may warrant surgery to restore the joint’s contour and prevent subsequent traumatic arthritis. This feature of a fracture line, if present, constitutes important information.
Anatomic bony reference points should be cited when applicable. A fracture just above the condyles of the distal humerus or femur, for example, is termed a supracondylar fracture. A fracture running from the greater to the lesser trochanter of the proximal femur is an intertrochanteric hip fracture, whereas a fracture just below the trochanters is subtrochanteric, a fracture just above them is said to involve the femoral neck, and a higher fracture just below the femoral head is referred to as subcapital. The area at or proximal to the coronoid process of the ulna is the olecranon and should be referred to as such, rather than simply the “proximal ulna.” Other bony landmarks include the radial head at the elbow, radial styloid at the wrist, and the greater tuberosity of the humeral head. Numerous additional examples exist.
The most common orientations of fracture lines are illustrated in Figure 267-2. Torus and greenstick fractures occur almost exclusively in young children, whose bones are more pliable than those of adults. Note the segmental fracture, which is commonly described incorrectly as a comminuted fracture. To an orthopedist, the term comminuted
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree