36 Inflammatory Bowel Disease
• Acute exacerbations of inflammatory bowel disease are characterized by abdominal pain, nausea, vomiting, diarrhea, and gastrointestinal bleeding.
• Life-threatening complications include bowel obstruction, hemorrhagic shock, toxic megacolon, malabsorption, abscess formation, and sepsis.
• Treatment with analgesics, intravenous hydration, antiemetics, and electrolyte replacement should occur in parallel with appropriate diagnostic imaging and laboratory studies.
• Antibiotics, steroids, and immunosuppressant therapies can be used in conjunction with specialty consultation.
• Hypersensitivity reactions may result from long-term immunomodulator and antiinflammatory therapies.
• Patients receiving immunosuppressant therapy have increased susceptibility to opportunistic infections.
Perspective
Approximately 1 million people in the United States suffer from inflammatory bowel disease (IBD). The two major forms of IBD are Crohn disease and ulcerative colitis (UC). The incidence of both disease processes is similar, although Crohn disease appears to be increasing.1 Each disease may relapse and remit, with exacerbations that often require emergency care and hospitalization.
IBD has a familial predilection, with an absolute risk of 7% among first-degree relatives.2,3 Up to a fifth of patients with IBD have an affected first-degree family member. Ashkenazi Jewish populations continue to have the highest documented incidence per capita of any group in the world. Hispanic and African American populations have a lower incidence of IBD than the Caucasian population does.4
The age at onset of IBD is bimodal. The greatest numbers of new cases are diagnosed in patients 15 to 35 years of age. Classically, a second peak is observed during the sixth decade of life.5 Advances in diagnostic testing have probably contributed to an overall rise in the number of new cases of IBD, as well as to the identification of the disease in younger patients.
Pathophysiology
Crohn Disease
Epidemiology
The cold chain hypothesis suggests that the rise in incidence of Crohn disease has been associated with the development of home refrigeration techniques. Bacteria that thrive in refrigerated foods, such as Yersinia and Listeria, are thought to play a role in stimulation of the immune and inflammatory responses that ultimately lead to Crohn disease.6 Exacerbations of Crohn disease may be worsened during periods of higher physiologic or mental stress.7 Other environmental factors such as cigarette smoking, use of nonsteroidal antiinflammatory drugs (NSAIDs), increased refined sugar intake, increased dietary fat, and decreased fiber intake have been linked to the development of Crohn disease.8–11
Genetic mutations and chromosomal variants have also been linked to the development of Crohn disease. Specific alterations in the NOD2 gene are associated with a 20-fold increase in the likelihood of Crohn disease with ileal predilection.12–15 Patients with Crohn disease may also be HLA-B27 positive.
Clinical Presentation
Crohn disease is associated with an increased risk for demyelinating diseases, as well as a higher incidence of inflammatory processes such as asthma, arthritis, bronchitis, psoriasis, and pericarditis.16,17 Approximately 20% of patients with Crohn disease experience one or more of the following extraintestinal manifestations of disease during their lifetimes: ankylosing spondylitis, uveitis, episcleritis, hepatitis, cholelithiasis, pancreatitis, primary sclerosing cholangitis, cholangiocarcinoma, nephrolithiasis, and erythema nodosum (Fig. 36.1; Box 36.1).
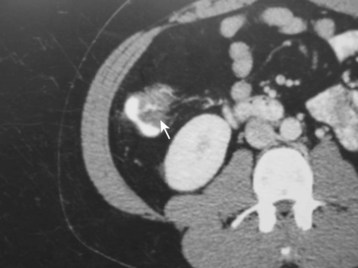
Fig. 36.1 Computed tomography scan showing terminal ileitis (arrow) in a patient with Crohn disease.
Epidemiology
The yearly incidence of UC is relatively constant—in the United States it is 8 per 100,000 people, with a disease prevalence of 246 cases per 100,000 people.18,19 The etiology of this disease is unknown, although certain risk factors have been identified. UC is most commonly found in North American and northern European Caucasian populations. In addition, similar to Crohn disease, development of UC has been linked to the use of NSAIDs, increased refined sugar intake, increased dietary fat, and decreased fiber intake.9–11
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







