Chapter 24 Infectious Disease Exposure
Infectious disease exposure in the operating room (OR) and sterile processing department (SPD) environments is a complex, multifaceted, and ever-changing challenge. Developing a comprehensive understanding of these evolving occupational risks within the OR and SPD environments requires dedication and a commitment to ongoing learning. Advancements in infection control and prevention (IPC) activities within the OR and SPD can be attributed to the involvement and collaboration of many governmental and professional organizations, dedicated professionals, and the patients who provide the impetus for our practices. Preventing infectious disease exposure should always be a primary consideration during the provision of patient care, but prevention must be viewed as a two-way street: the patient on one side and the health care provider on the other. In particular, everyone should strive to make personal hand hygiene the basis for providing quality health care for both the patient and oneself. Although the rationale for performing hand hygiene (HH) may not be ideal, the most recent release of the standard precautions guidelines provides the health care worker with a direction: “Standard precautions are intended to protect patients by ensuring that health care personnel do not carry infectious agents to patients on their hands or via equipment used during patient care” (Siegel et al, 2007). Standard precautions protect not only the patient, but the staff as well. Standard precautions and many other infection prevention and control principles assist with guiding our efforts to mitigate risk for and prevent infectious disease exposure in the OR and SPD.
HISTORICAL BACKGROUND
Harvey Cushing (1869–1939) stated, “Certainly infections cannot be attributed to the intervention of the devil but must be laid at the surgeon’s door” (Miller et al, 2005). This quotation provides a sample of the varying opinions of the time regarding infections. With the advancement and controversy regarding germ theory in the late 1800s one can understand the reasoning behind the thought process. Knowing what we know today regarding germ theory and the complexity of preventing infectious disease exposure, we must recognize how far the efforts have progressed.
Modern IPC as we know it now began to make solid progress during the mid-nineteenth century. As early as 1842 Oliver Wendell Holmes (1809–1894) of Harvard was recommending a hand wash of calcium chloride to prevent the spread of infection from the autopsy room to the ward (Miller et al, 2005). Similarly, Ignaz Philipp Semmelweis (1818–1865) provided a 2-year study demonstrating that a hand wash with a chloride of lime solution reduced puerperal sepsis mortality from 9.92% to 1.27% (Miller et al, 2005). Louis Pasteur (1822–1912) made additional advancements in the IPC world, most notably in germ theory. The germ theory postulated that most infectious diseases are caused by living organisms or germs. Pasteur is also well known for his work in the fermentation and pasteurization processes (Bellis, 2009). Joseph Lister (1827–1912) further advanced the work of Pasteur, applying it to surgical practice. Lister began applying carbolic acid to compound fracture wounds and documented a significant decrease in mortality rate from 45% to 15% (Miller et al, 2005). Upon hearing a lecture by Lister, U.S. neurosurgeon William W. Keen (1837–1932) began pioneering many of Lister’s recommendations to neurosurgical practice with marked success (Miller et al, 2005).
The invention, development, and use of antiseptic solutions and supplies, aseptic technique, and sterilization of surgical instruments further improved the care and prevention of infection in surgical patients. In 1889, following a request by William Stewart Halsted (1852–1922) to Goodyear Rubber Company to develop rubber gloves for his scrub nurse because of an allergy to an instrument disinfectant, wearing of surgical gloves to protect the patient and staff members eventually emerged as common practice (Miller et al, 2005; Rothrock, 2007).
The first IPC efforts in the United States began in the 1950s concurrent with the growth of the intensive care unit and subsequent increases in staphylococcal infections (Friedman and Petersen, 2004). Formal IPC programs became common in hospitals in the 1970s, but it was not until 1976 that standards were established and an IPC program became a requirement for health care organizations (Friedman and Petersen, 2004).
The contributions of all the aforementioned professionals and countless others, as well as governmental and professional entities, have shaped and organized the current IPC programs, regulations, and requirements. Among the most influential in the modern IPC realm is the introduction by the Occupational Safety and Health Administration (OSHA) (2008) of universal precautions in 1991. Universal precautions, in addition to the standard and transmission precautions recommended by the Centers for Disease Control and Prevention (CDC), provided a solid foundation on which to build the modern IPC program. Without these modern-day IPC guidelines the number of infectious disease exposures in the OR and SPD would be astounding. These developments highlight only a few efforts in the development of a professional infection control program and provide a brief history in the evolution and development of modern IPC practices. Implementation of modern practices has been of great benefit to our patients, as well as preventing infectious disease exposure of staff members.
CHAIN OF INFECTION
The human body is resilient and has redundant but necessary and complementary layers in its defense against infectious disease. The body’s defensive measures include external barriers, the inflammatory response, and the immune response (Rothrock, 2007). External barriers include healthy intact skin and mucous membranes. An inflammatory response can occur systemically or locally in tissue following injury in an attempt to isolate the offensive foreign object or pathogen (Phillips, 2004). The final defense measure, the immune response, may be passive or active immunity and is triggered by the inflammatory response (Phillips, 2004; Rothrock, 2007).
Essential to preventing disease exposure and subsequent infections is an understanding of the infectious process. The infectious process is often described as a chain of infection (Figure 24-1). Each link in the chain of infection has categories essential to understanding how to break, prevent, or interrupt the link in the infectious disease process.
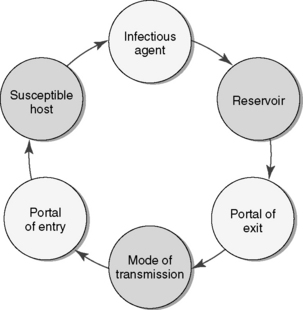
Figure 24-1 Example of chain of infection/infectious disease process.
(From Potter PA, Perry AG: Basic nursing, ed 6, St. Louis, 2007, Mosby.
The first link in the chain is the causative agent or the infectious agent. The causative agent may be bacterial, viral, fungal, protozoan, helminthic, or prionic in nature (Association for Professionals in Infection Control and Epidemiology [APIC], 2005). Activities that will break this link in the chain include early, accurate identification of signs and symptoms of illness and prompt identification of the causative agent. The occupational health screenings and policies must be clear, easy to understand, and available to staff members (APIC, 2005).
The second link in the chain is the reservoir or carrier. Reservoirs are a place for the infectious agent to survive. The most common reservoirs are environmental, human, and animal (APIC, 2005). An infinite number of examples of environmental reservoirs are possible given an improperly cleaned OR or SPD environment. Activities that break this link in the chain related to the OR and SPD start at the point of use, either the OR or clinics. All instruments need to be cleaned of gross debris and sprayed with an enzymatic cleaner before being sent to the SPD department. Implemented processes include stringent monitoring, maintenance, and cleaning of the environment, as well as proper cleaning, disinfection, and sterilization of instruments and equipment. An example of a human reservoir is a health care worker who had a previous multidrug-resistant organism (MDRO) skin infection but now has MDRO skin flora or is colonized with the MDRO. Activities in the OR that can break this link in the chain related to the human reservoir include frequent personal hygiene (hand washing), effective occupational health screenings, and use of standard precautions. For personal safety and the safety of their patients, employees must be aware of and comply with occupational health screenings and policies.
The next three links are very closely related. The portal of exit, mode of transmission, and portal of entry links happen almost simultaneously. The portal of exit is the method by which the infectious agent leaves the reservoir. Portals of exit include respiratory, genitourinary, and gastrointestinal tracts; intact and nonintact skin; mucous membrane; placenta; and blood (APIC, 2005). The mode of transmission is the method by which the infection is passed on to a susceptible host (APIC, 2005). The mode of transmission may be by direct contact between the reservoir and susceptible host or between the environment and a susceptible host. Depending on the organism, the mode of transmission may also be by droplet or airborne transmission. The best opportunity to break the chain during these three links is with the mode of transmission link. This is accomplished in the OR by using appropriate contact, droplet, and airborne precautions based on the infectious illness, an action that may mitigate much of the risk for employee infectious disease exposure (see Appendix B). Portals of entry include the respiratory tract, genitourinary tract, gastrointestinal tract, intact and nonintact skin, mucous membrane, placenta, and parenteral (APIC, 2005).
The final link, the susceptible host, completes the chain of infection. A susceptible host is essential in contracting an infectious agent. The susceptibility of a host is influenced by many factors including age, sex, ethnicity, socioeconomic status, marital status, medical history, lifestyle, heredity, nutritional status, occupation, immunization status, diagnostic/therapeutic procedures, medications, pregnancy, underlying disease, and trauma (APIC, 2005; Otaiza and Pessoa Da Silva, 2008).
The chain of infection provides a good depiction of the infectious disease process. Typically staff members think the infectious disease process centers on mitigating exposure to the infectious patient. However infectious diseases do not discriminate. A susceptible host may come in the form of a patient or a staff member. The staff member who has an infection or is colonized can easily spread an infectious agent to a patient during the provision of health care. Staff members providing direct patient care must be aware of occupational health policies, and if they have an infection or are colonized, they must receive the appropriate treatment and evaluations before returning to their direct patient care job (Otaiza and Pessoa Da Silva, 2008). In addition, staff members must receive periodic occupational health screenings to ensure that they are healthy, are using personal protective equipment appropriately, and understand the postexposure protocols of their institution (Otaiza and Pessoa Da Silva, 2008).
BASIC COMPONENTS OF AN INFECTION PREVENTION AND CONTROL PROGRAM
Surveillance
Surveillance is the systematic, active, ongoing method of collecting, consolidating, and analyzing data concerning the distribution and determinants of a given disease or event, followed by the dissemination of that information to those who can improve the outcomes (APIC, 2005). IPC practitioners obtain, analyze, report, and distribute critical data and information related to the prevention and control of infections within their organization. Surveillance activities include collecting data that enable epidemiologic studies and illness tracking to be performed. The OR and SPD sections provide the IPC practitioner with an immense amount of surveillance data and have a profound influence on the effectiveness of any IPC program. Examples of surveillance activities in an OR include surgical site infection (SSI) rates; compliance with actions to prevent SSIs; monitoring and recording of the environmental parameters; environmental cleaning policies and procedures; flash sterilization rates and quality assurance monitoring, which includes biological and decontamination testing; and environment of care surveys. Examples of surveillance activities in the SPD include quality assurance testing, monitoring and recording environmental parameters and cleaning records, and environment of care surveys. The basic components of the IPC program can provide reciprocating data and information to the OR and SPD departments, including occupational health data, trending of SSIs, enhancing quality assurance activities, and assistance with education and training of OR, SPD, and environmental cleaning staff.
Intervention and Investigation
Following the analysis of the collected data, it is imperative to appropriately intervene to prevent infection. Surveillance may reveal an outbreak of infection. An outbreak is a cluster of infections greater than expected or the occurrence of an unusual infection (Friedman and Petersen, 2004). The source of an outbreak might be a patient, but it might also be a staff member stemming from an infectious disease exposure. Similar infection types of SSIs may indicate an outbreak and warrant an investigation. The goal of an investigation is to control and prevent further infections and to identify contributing factors so that prevention measures can be implemented (Friedman and Petersen, 2004).
Competent Practitioners
One of the most critical effects an IPC practitioner has is that of an educator. The IPC practitioner provides education to both patients and staff members. The IPC practitioner teaches the staff the scientific rationale for the precautions that allow health care workers to apply procedures safely and correctly. IPC practitioners can also teach safely modified precautions based on changing requirements, resources, or health care settings (Siegel et al, 2007). Education requirements for newcomers and annual training, educational refreshers, and in-service programs for staff based on surveillance activities are just a few of the educational offerings an IPC practitioner provides to staff. In a recent study the likelihood of a health care worker’s developing sudden acute respiratory syndrome (SARS) was strongly associated with less than 2 hours of infection control training and lack of understanding of infection control procedures (Siegel et al, 2007).
STANDARD AND TRANSMISSION-BASED PRECAUTIONS
Standard Precautions
The most recent release of standard precautions by the CDC in 2007 evolved from the universal precautions mandated by OSHA. Standard precautions combine universal precautions and body substance isolation and are based on the principle that all blood, body fluids, secretions, excretions except sweat, nonintact skin, and mucous membranes may contain transmissible infectious agents (Siegel et al, 2007). Standard precautions include a combination of infection prevention and control measures such as hand hygiene (HH); use of gloves, gowns, masks, eye protection, or face shield, depending on the anticipated exposure; safe injection practices; respiratory hygiene and cough etiquette; and use of masks for insertion of catheters or injection of material into spinal or epidural spaces via lumbar puncture procedures (Siegel et al, 2007). Standard precautions should be used for all patients regardless of whether an infectious illness is confirmed or unconfirmed and based upon the anticipated level of exposure (AORN, 2009).
Hand Hygiene
HH has been demonstrated to be one of the most important activities to prevent the spread of infection in the health care setting (Siegel et al, 2007). HH is important because it minimizes the risk for transmitting infection to and between patients, as well as staff. A complete HH program not only minimizes risk, but also offers convenient HH options designed to maximize staff compliance (AORN, 2009). Most HH programs offer a selection of traditional or antiseptic hand soap, an alcohol-based hand sanitizer, a surgical hand antiseptic, and hand lotion. Selection of the appropriate HH agent is situationally dependent and must be approved by the hospital’s infection control committee. A staff member’s awareness of a patient illness when choosing the appropriate method of HH is imperative. For example, when a staff member is caring for a patient with a spore-forming illness (e.g., Clostridium difficile or Bacillus anthracis), alcohol-based hand sanitizers are ineffective and a hand wash must be performed. A hand wash should also be performed when hands are visibly soiled. HH should be performed at the beginning and end of a work shift, before and after patient contact and after removing gloves, before and after eating, before and after entering the restroom, anytime there has been a possibility of contact with blood or potentially infectious materials, and anytime when hands are or may have been soiled. In addition, the maintenance of health skin integrity with the frequent application of skin-moisturizing lotions is very important to minimize the portal of entry for infectious disease.
Personal Protective Equipment
Personal protective equipment (PPE) refers to a variety of barriers and equipment used alone or in combination to protect mucous membranes, the airway, skin, and clothing from contact with infectious agents (Friedman and Petersen, 2004; Siegel et al, 2007). PPE includes gloves, masks, goggles, face shields, glasses, and gowns. PPE is intended to prevent the spread of microorganisms from patient to caregiver and from caregiver to patient by creating a barrier between the patient and caregiver and between caregiver, patient, and an infectious organism (Boxes 24-1 and 24-2) (Friedman and Petersen, 2004).
BOX 24-1 Safe Donning of Personal Protective Equipment (PPE)
From Siegel JD et al: Guideline for isolation precautions: preventing transmission of infectious agents in healthcare settings, June 2007, Centers for Disease Control and Prevention, available at http://www.cdc.gov/ncidod/dhqp/pdf/guidelines/Isolation2007.pdf. Accessed August 29, 2009.
BOX 24-2 Safe Removal of Personal Protective Equipment (PPE)
Remove PPE at doorway before leaving patient room or in anteroom.
From Siegel JD et al: Guideline for isolation precautions: preventing transmission of infectious agents in healthcare settings, June 2007, Centers for Disease Control and Prevention, available at http://www.cdc.gov/ncidod/dhqp/pdf/guidelines/Isolation2007.pdf. Accessed August 29, 2009.
Gloves are indicated when it is anticipated that contact with blood or bodily fluids will occur. There are different types of gloves, and gloves are made of many different materials (Friedman and Petersen, 2004). The type of glove used should be based on the specific activity, allergy of the wearer, and personal preference (Friedman and Petersen, 2004). The use of sterile surgical gloves during surgical and invasive procedures protects not only the patient, but also the staff member from the risk for infection. The practice of double gloving for surgical procedures should always be standard practice in the surgical setting for various patient and staff safety reasons. First, the imperviousness of sterile surgical gloves may not be completely intact. The U.S. Food and Drug Administration (FDA) accepts a failure rate of 2.5% for new unused sterile gloves in quality control tests (Berguer and Heller, 2005). Although 2.5% may be a very small and acceptable number according to the FDA, the potential risk to patients and staff is too high not to double glove and minimize risk. Secondly, double gloving can reduce the risk for exposure to patient blood by as much as 87% when the outer glove is punctured (Berguer and Heller, 2005). Furthermore, the volume of blood on a suture needle is reduced 95% when passed through two glove layers (Berguer and Heller, 2005).
Masks, goggles, face shields, and glasses also constitute PPE. These protect the mucous membranes of the nose, mouth, and eyes during procedures and activities that generate splashes, splatters, sprays, or aerosols of blood or other potentially infectious materials (AORN, 2009). The choice of eye wear protection—whether it is goggles, a face shield, or glasses—is based upon the staff member’s perceived level of anticipated exposure and personal preferences. In the OR and SPD setting the potential level of exposure is high; therefore eye protection should be worn consistently in these high-risk environments.
Impervious gowns and aprons must be used to protect the skin and clothing during activities that generate splashes, splatters, sprays, or aerosols of blood or other potentially infectious materials. Scrub attire, laboratory jackets, and warm-up jackets are not considered adequate for PPE because they are not impervious. Grossly soiled scrub attire and laboratory and warm-up jackets should be changed as soon as feasible (OSHA, 2008).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







