Incidents and Adverse Events
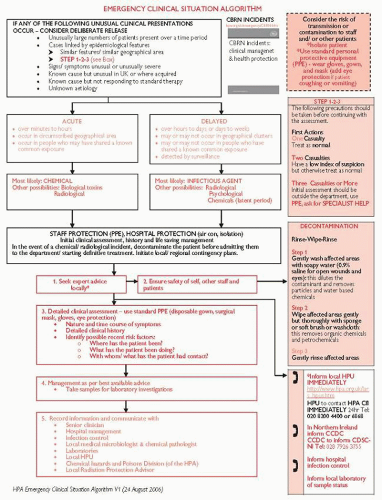
Suspected outbreaks may be associated with infections, biological agents, or poisonings (chemical, nutritional, or radioactive). Suspicious circumstances include: intelligence of a threat, multiple cases, simultaneous outbreaks elsewhere, and illness affecting a particular community.
Presentation and assessment
Illnesses which do not fit any recognizable clinical condition.
A known illness that is not expected in the setting where observed, or follows an unexpected course.
Illnesses that should arouse suspicion include:
Clusters (>2) of patients with similar symptoms.
Signs and symptoms inappropriate to patient’s history/location.
Signs/symptoms of syndromes/toxidromes (see p.452), such as:
p.452), such as:
Respiratory symptoms: chest tightness, pulmonary oedema, associated eye irritation (phosgene, chlorine, mustard gases)
Unexplained severe metabolic acidosis (cyanides)
Skin blistering, unexplained ‘thermal’ type burns
Fever with paralysis, mediastinal lymphadenopathy, or haemorrhagic thrombocytopaenia, see pp.358 and 370 (anthrax, VHFs, tularaemia, pneumonic plague)
pp.358 and 370 (anthrax, VHFs, tularaemia, pneumonic plague)
Aplastic anaemia, hair loss, severe GI loss
Investigations
For biological agent exposure, the following samples may be requested:
Serum and whole blood EDTA (paired sample if recovery occurs).
Blood cultures (at least 1 sample prior to antibiotics if possible).
Sputum or bronchoalveolar lavage (if safe to do so).
Biopsy or aspiration samples of necrotic lesions or vesicles (vesicle swabs should be placed in viral transport medium).
Pus and/or swabs (take multiple samples).
Urine and other body fluids.
Stool or vomitus sample (if food contamination suspected).
Take HPA advice on sample precautions. The specimen should be labelled with surname/forename/DOB, and transported to a clinical microbiology laboratory as soon as possible.
Further actions
Decontaminate before ICU admission; if unsure contact the HPA.
Make list of all staff who may have been exposed; treat waste, property and samples as hazardous until advised otherwise.
Use personal protective equipment as advised by HPA; if uncertain, use gloves, gown, cap, mask and eye protection (see p.384 for instructions on how to don protective equipment in high-risk cases).
p.384 for instructions on how to don protective equipment in high-risk cases).
Give appropriate treatments where they are available:
Further reading
Health Protection Agency. CBRN incidents: clinical management and health protection. London: HPA, 2005.
Health Protection Agency. Initial investigation and management of outbreaks and incidents of unusual illnesses: A guide for health professionals, 2010. Available at:  <http://www.hpa.org.uk/webc/HPAwebFile/HPAweb_C/1201265888951>.
<http://www.hpa.org.uk/webc/HPAwebFile/HPAweb_C/1201265888951>.
 <http://www.hpa.org.uk/webc/HPAwebFile/HPAweb_C/1201265888951>.
<http://www.hpa.org.uk/webc/HPAwebFile/HPAweb_C/1201265888951>.White SM. Chemical and biological weapons. Implications for anaesthesia and intensive care. Br J Anaesth 2002; 89(2): 306-24.
A major incident may be external (a disaster in the community) or internal (e.g. a fire). It is loosely defined as any incident that generates sufficient numbers/types of casualties as to require special arrangements.
Every hospital (and ICU) should have a major incident plan of which staff should be aware. A major incident should trigger involvement of senior management within the hospital to co-ordinate an effective response from different clinical departments. ICU staff may have to work closely with operating theatres, A&E, and other high dependency areas within the same hospital and/or other hospitals.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 p.480
p.480 p.480
p.480 p.458
p.458 p.358
p.358 p.370
p.370