CHAPTER 59
Ilioinguinal and Iliohypogastric Nerve Blocks
INDICATIONS
The diagnosis and treatment of:
• Ilioinguinal neuralgia
• Iliohypogastric neuralgia
• Groin pain
• Inguinal pain, especially after mesh and/or staples
• Pelvic pain
• Postherpetic neuralgia
• Lateral abdominal wall pain postincision or trocar placement
CONTRAINDICATIONS
• Inability to communicate with the patient
• Infection
• Severe anxiety to needle sticks
• Anticoagulant or nonaspirin antiplatelet therapy
• Severe scarring over entire area to be injected
• Coagulopathy
• Psychogenic pain
RELEVANT ANATOMY
Iliohypogastric Nerve
• Branch of the L1 nerve root with a contribution from T12 occasionally.
• In a study of 100 embalmed cadavers, the iliohypogastric nerve originated from T12 on 14 specimens (7%), from T12 and L1 in 28 (14%), from L1 in 20 (10%), and from T11 and T12 in 12 (6%).1
• Follows an oblique course that takes it from L1 and T12 around the flank to perforate the transverse abdominis muscle and is positioned between it and the external oblique muscle terminating inside the ilium (Figure 59-1).
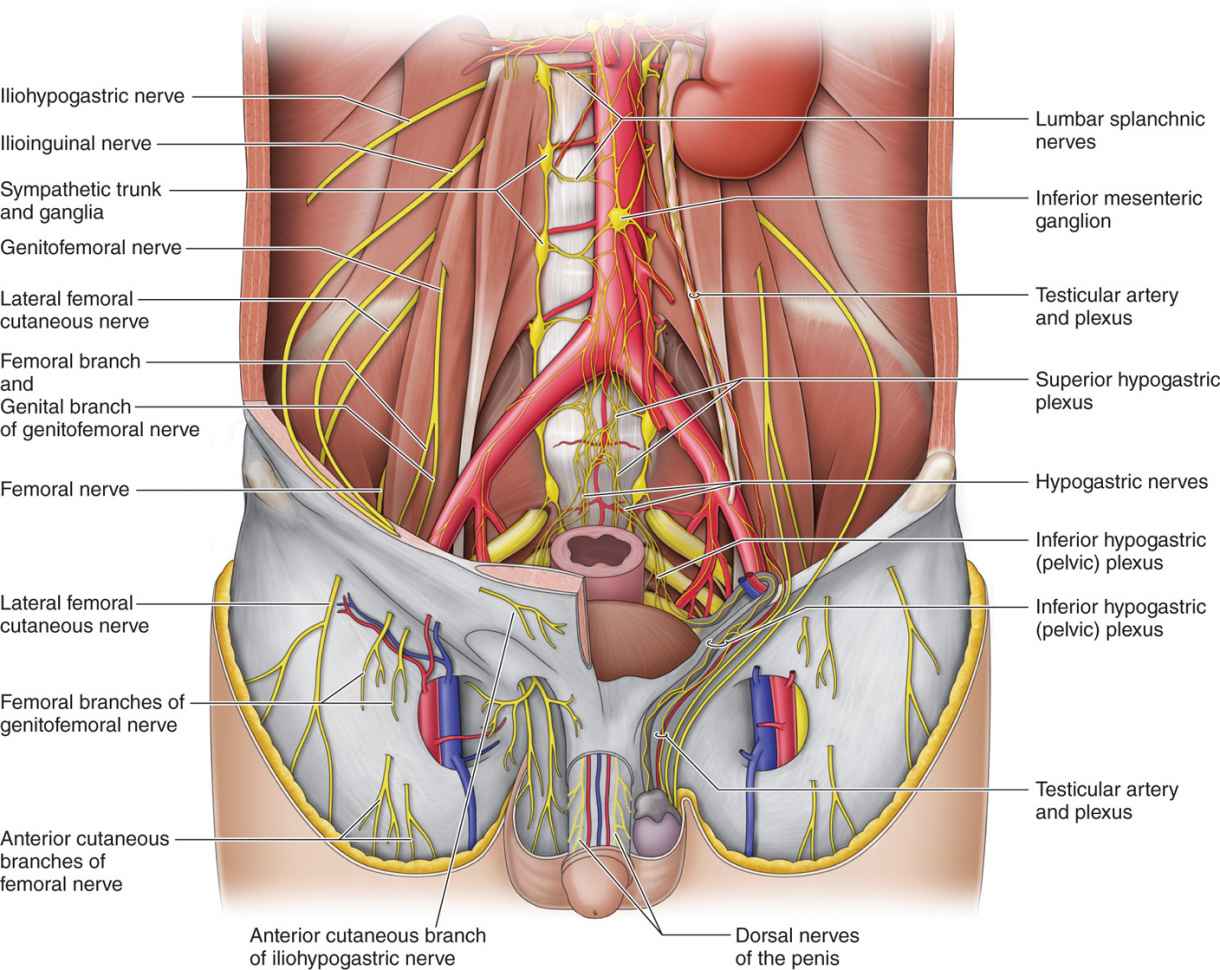
Figure 59-1. Ilioinguinal and iliohypogastric nerves.
• Often entrapped at the lateral edge of the rectus border (Figure 59-2).
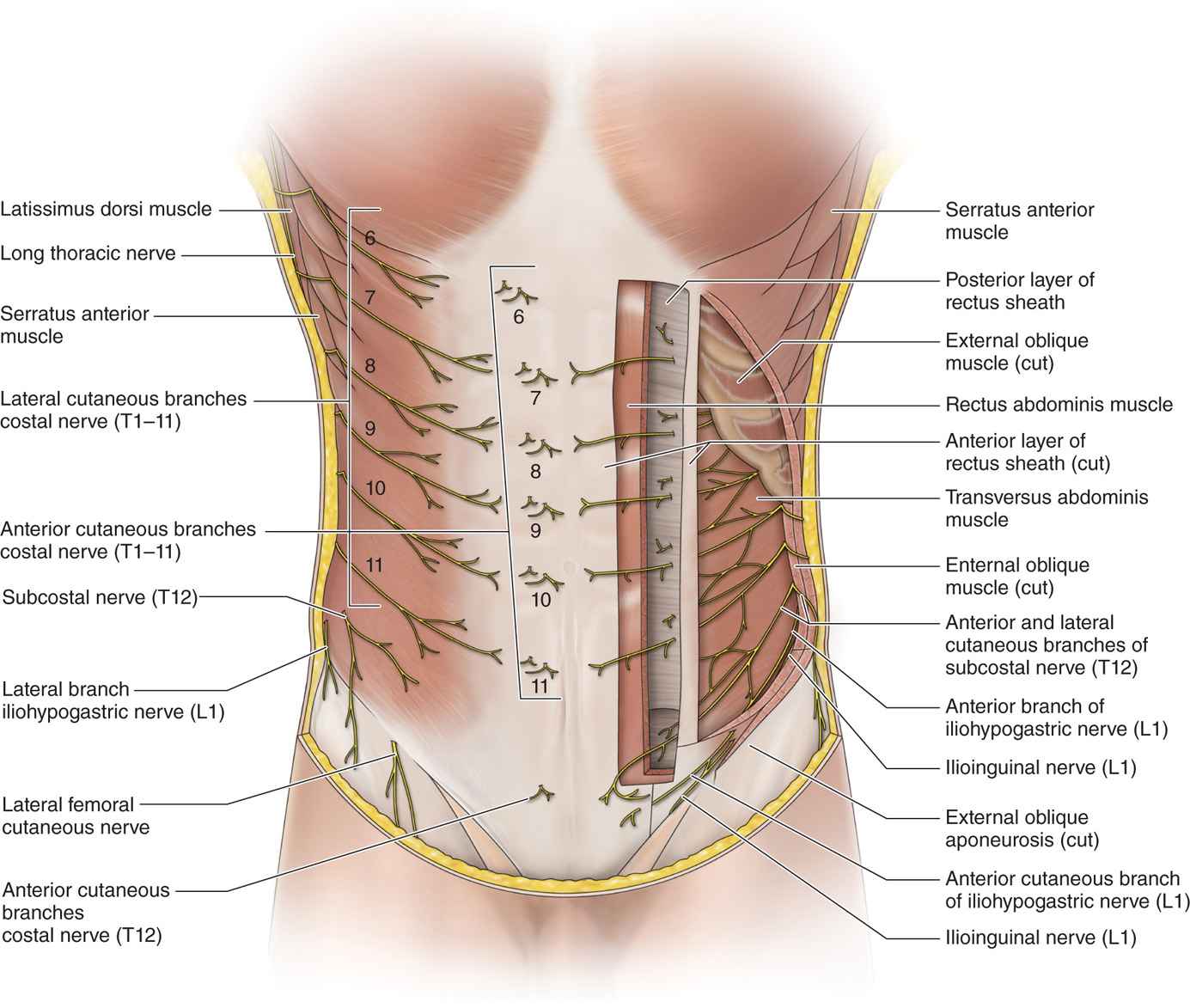
Figure 59-2. Entrapment at rectus border.
• May also be entrapped more proximally at the edge of the external oblique (Figure 59-3).
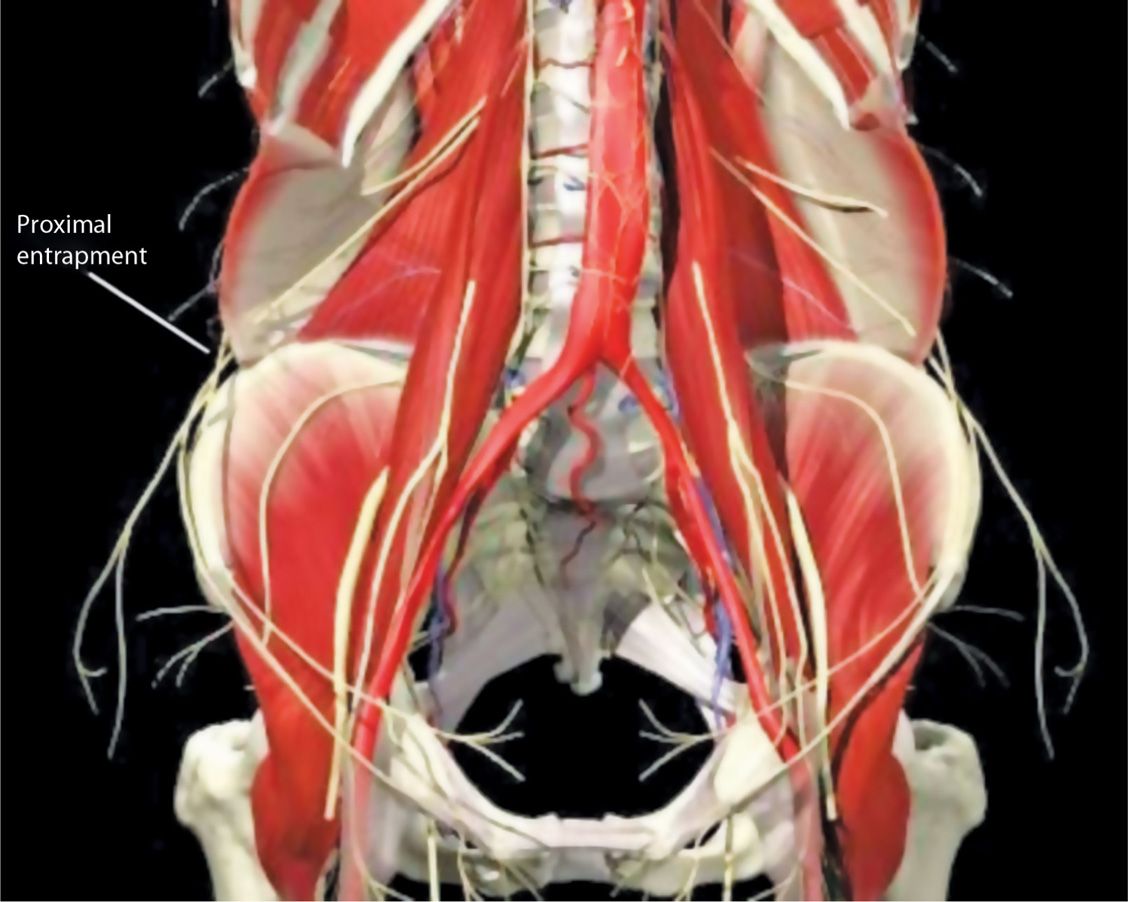
Figure 59-3. Proximal entrapment.
• Divides into an anterior and lateral branch after the perforation of the transverse abdominis muscle.
• The lateral branch gives sensory skin innervation to the posterolateral gluteal region, whereas the anterior branch gives skin sensory innervation to the abdominal skin above the pubis.
• Both ilioinguinal and iliohypogastric branches of this L1 nerve root may interconnect and provide significant variation of sensory innervation.
Ilioinguinal Nerve
• Branch of the L1 nerve root with a contribution from T12 in some patients.
• In a study of 100 embalmed cadavers, the ilioinguinal nerve originated from L1 in 130 specimens (65%), from T12 and L1 in 28 (14%), from L1 and L2 in 22 (11%), and from L2 and L3 in 20 (10%).1
• Penetrates the transversus abdominis at the anterior superior iliac spine and terminates in the ilium.
• Ilioinguinal nerve may interconnect with the iliohypogastric nerve as it passes along inferiorly and accompanies the spermatic cord through the inguinal ring and into the inguinal canal (Figure 59-1).
• Often entrapped at the lateral edge of the rectus border (Figure 59-2).
• May also be entrapped more proximally at the edge of the external oblique (Figure 59-3).
• Innervation of the ilioinguinal nerve includes the skin of the upper portion of the inner thigh, root of the penis, the upper scrotum in men, and the mons pubis and lateral labia in women.
PREOPERATIVE CONSIDERATIONS
• Informed consent and proper explanation of risks, complications, and benefits.
• Lateral abdominal wall, flank and lower abdominal surgeries can result in neuralgia to the ilioinguinal and iliohypogastric nerves, such as:
![]() Open appendectomy
Open appendectomy
![]() Open hernia repair
Open hernia repair
![]() Liposuction of abdominal or flank wall
Liposuction of abdominal or flank wall
![]() Pfannenstiel incisions
Pfannenstiel incisions
![]() Any laparoscopic abdominal procedures
Any laparoscopic abdominal procedures
![]() Liposuction abdomen and flank
Liposuction abdomen and flank
![]() Anterior spinal fusion chevron flank or retroperitoneal incision
Anterior spinal fusion chevron flank or retroperitoneal incision
Blockade of these nerves can be considered in preemptive analgesia for hernia surgery utilizing local anesthesia with or without intravenous or nitrous oxide mask sedation.
Fluoroscopic Views
• Generally not indicated for this procedure, unless obese patient or anatomy impairs palpation of anterior superior iliac spine (ASIS)
![]() Physical examination usually suffices (Figure 59-4)
Physical examination usually suffices (Figure 59-4)

Figure 59-4. Palpation of the iliohypogastric at the rectus border.
• Ultrasound guidance for these nerve blocks provides about 70% to 95% success2,3 (Figure 59-5).
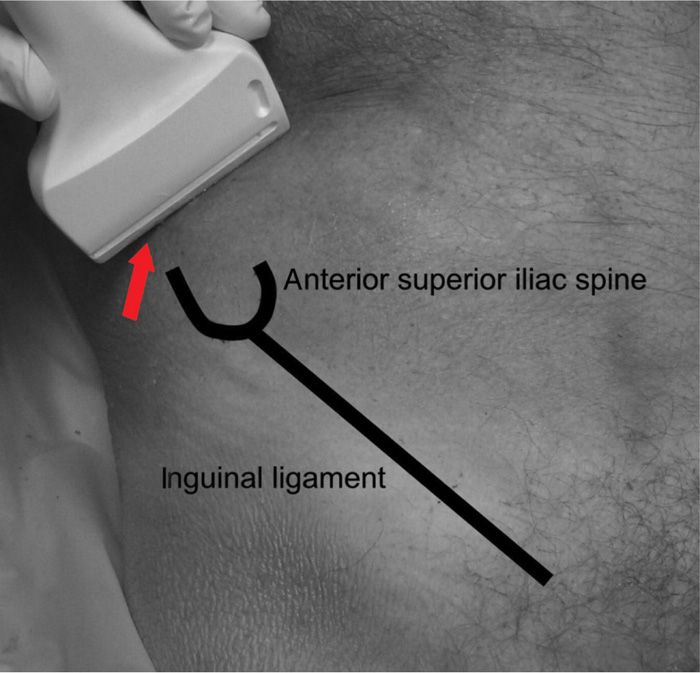
Figure 59-5. Ultrasound localization of ilioinguinal and iliohypogastric nerves at ASIS.
Equipment
• 25-gauge 2.0-in insulated needle
• 3-cc Luer lock syringe for local anesthetic
• Sensory nerve stimulator with alligator clip or other connections for grounding ECG pad and needle
Analgesia or Surgery
• 22-gauge 6- or 8-in spinal needle
• 3-cc syringe with 25-gauge 0.5-in needle
Radiofrequency or cryoanalgesia
• Radiofrequency or cryoanalgesia machine and appropriate cables and needles and/or cannulas and grounding pads as well as 20- or 21-gauge insulated RF needle or 12-gauge IV catheter for cryoanalgesia
Medications
• 0.75% or 0.50%, or 0.25% bupivacaine
• 1% or 2% lidocaine
• Deposteroid
• Neurolytic
![]() 5% to 10% phenol in saline or glycerin
5% to 10% phenol in saline or glycerin
![]() Absolute alcohol
Absolute alcohol
Technique
Diagnostic Block
• The patient is placed in the supine position with a pillow under the knees with the legs extended to avoid exacerbation of abdominal pain due to stretching of extended legs.
• For rectus entrapments, the lateral edge of the rectus is palpated, and the point tenderness identified (Figures 59-4 and 59-6).
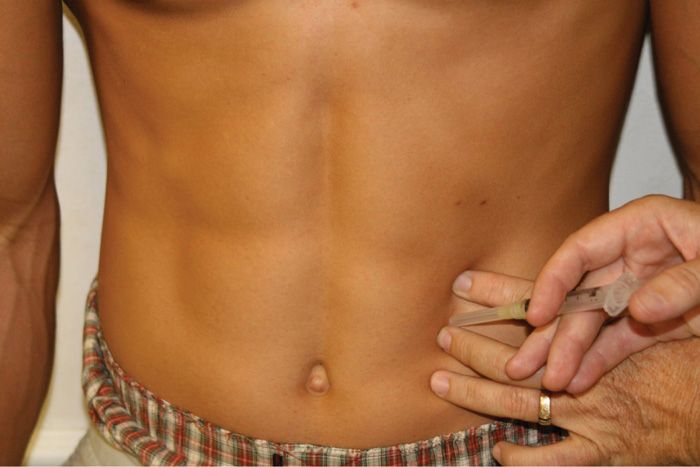
Figure 59-6. Injection at the rectus border.
• For more proximal injections, the anterior superior iliac spine on the affected side is located by palpation. A point 2 to 3 cm inferior and medial to the iliac spine is the insertion site for the 25-gauge insulated needle (Figure 59-7).
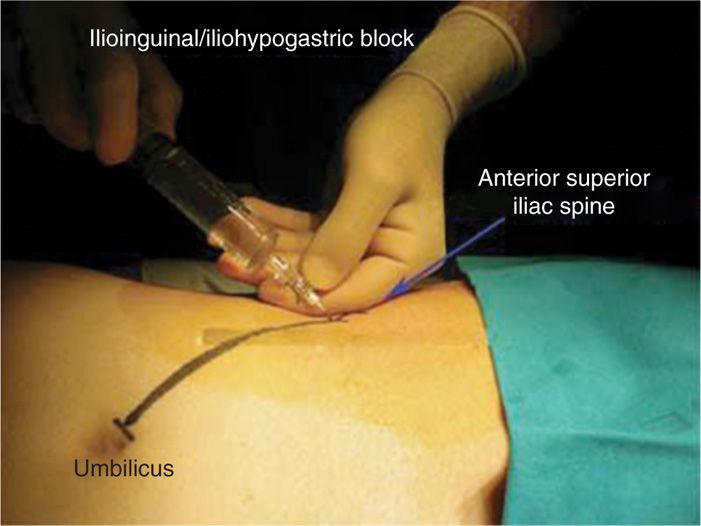
Figure 59-7. Injection at the ASIS.
• Insertion should be directed inferior and slightly medial toward the crease of the affected inner leg junction with the pubis for the ilioinguinal nerve.
• For the iliohypogastric nerve, the needle angle is directed more medial and inferior toward the umbilicus.
• Connect the nerve stimulator and grounding pad to the needle and begin testing for patient sensation along the tested nerve with between 0.2 and 0.5 V.
• It may be necessary to project nearly the entire needle length and to make multiple deliberate parallel needle stimulation passes in order to locate the nerves.
• Once sensation is felt between these parameters, then inject less than 1 cc of local anesthetic with deposteroid onto each nerve and remove the needle.
Preemptive Analgesia or Surgical Block
• Utilize the same ASIS position and location of insertion of needle with the same inferior but more perpendicular approach and inject in a fan like direction through the subcutaneous tissue.
• Then inject along an additional line of subcutaneous and intramuscular injection from the iliac spine to the inferior umbilicus at the midline.
• Now make a new inferior injection through the subcutaneous and intramuscular tissue over the midline starting just below the umbilicus and directed inferior to just above the pubis.
• The surgeon will frequently add injection into the spermatic cord, so calculate your total volume allowing for 5 to 10 cc of local anesthetic by the surgeon.
Ablation by Pulsed Mode Radiofrequency
• Place needle as above for diagnostic block for each nerve, then for RF, place probe into insulated needle.
• Begin sensory nerve stimulation until patient feels stimulation between 0.2 and 0.5 V.
• Maintain firm grip on needle with fingers resting on abdomen and treat at 42 to 45°C for 2 minutes per nerve.
Cryoanalgesia
• Use a larger 12-gauge angiocath and follow the same technique for placing diagnostic needle.
• Remove stylet and place cryoprobe with enclosed nerve stimulator into cannula (Figure 59-8).

Figure 59-8. Cryoneuroablation probe in place.
• Test sensory nerve through the treatment probe as with RF and treat by increasing gas flow to 10 to 12 L/min.
• A series of 3 two-minute freezes with 30 seconds for defrosting between each cycle is performed.
Ablation by Phenol or Absolute Alcohol
• Injection of 1 cc of 5% to 10% phenol or absolute alcohol on each nerve after satisfactory diagnostic block and adding the phenol or alcohol after the local anesthetic injection (to avoid injection pain).
POSTPROCEDURE FOLLOW-UP
• 5 to 10 minutes of immediate follow-up for location and presence of pain relief secondary to local anesthetic along with telephone contact the next day for potential complications as well as significance and length of time of pain relief.
POTENTIAL COMPLICATIONS AND PITFALLS
• Since the diagnostic block, radiofrequency or cryoanalgesia procedures are primarily subcutaneous techniques, they are associated with few complications. There is a chance of hematoma and postblock ecchymosis.4
• The preemptive or surgical block is intramuscular and subcutaneous so the possibility of peritoneal penetration and colon perforation exists. Also there is a possibility of hematoma formation in the area of the cord, which is a relative complication for the surgeon by hindering visualization of the surgical dissection.
• Destruction of surrounding non-nerve tissue is a complication of phenol and absolute alcohol.
CLINICAL PEARLS
• Ilioinguinal and iliohypogastric nerve blocks are relatively simple procedures that usually provide near-complete pain relief.
• These injections can be diagnostic and therapeutic. The patients with positive diagnostic but not therapeutic response are candidates for an ablation procedure using pulsed mode RF, cryoanalgesia, or phenol/alcohol.
• Pressure should be applied to the injection site for prevention of hematoma and ecchymosis, especially for large cannula procedures like cryoanalgesia and after surgical or preemptive blocks.
• Absolute alcohol and phenol injections should only be utilized for cancer pain patients with limited lifespan who suffer from intractable ilioinguinal or iliohypogastric neuralgia.
• The success of the diagnostic procedure is most dependent on accurate placement of the nerve stimulation needle and a steady hand upon location of the affected nerve until injection of the local anesthetic.
• The success of pulsed mode RF depends on appropriate location of the insulated treatment needle more perpendicular than parallel to the nerve and sensation along the nerve tract between 0.2 and 0.5 V. This treatment provides 6 to 18 months of at least 50% relief.5,6 Lower percentage relief usually indicates more than one nerve branch is involved, requiring subsequent treatment of the untreated branch(es).
• Cryoanalgesia provides 4 to 30 months of good to excellent relief for each nerve properly identified with nerve finder stimulation.7
• Phenol provides good relief with the possibility of necrosis on and around the nerve.8,9
• Absolute alcohol provides good relief with the possibility of nerve and surrounding permanent necrosis and damage.10
If patients present with ilioinguinal or iliohypogastric dermatomal pain and do not get relief from a diagnostic block, then consider T12, L1, or L2 nerve root pathology. Also consider pudendal nerve pathology in refractory cases.
• It is not unusual to block branches of both nerves with 1 injection due to the possibility of multiple branches and overlapping innervation of both nerves.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






