INTRODUCTION AND EPIDEMIOLOGY
Hypothyroidism is a clinical syndrome caused by insufficient thyroid hormone production, which slows cell metabolism. Hypothyroidism is common in areas where iodine deficiency is common, particularly inland areas where there is no access to marine foods. In iodine-sufficient areas, chronic autoimmune destruction of thyroid gland (e.g., Hashimoto’s thyroiditis) and iatrogenic causes from treatment of Graves’ disease are the leading causes of hypothyroidism (after thyroidectomy or radioactive iodine ablation). The prevalence of hypothyroidism increases with age, and the disorder is nearly 10 times more common in females than in males.1 Subclinical hypothyroidism is more prevalent than overt hypothyroidism in all age groups and can be seen in 4% to 15% of women, especially the elderly.2,3
Hypothyroidism occurs in 1% to 32% of patients taking amiodarone.1
PATHOPHYSIOLOGY
Primary hypothyroidism is caused by the intrinsic dysfunction of the thyroid gland, and this is the most common type. Secondary hypothyroidism is caused by a deficiency of thyroid-stimulating hormone from the pituitary gland or deficiency of thyrotropin-releasing hormone from the hypothalamus. Table 228-1 lists common causes of hypothyroidism. Euthyroid sick syndrome or low thyroxine syndrome, also called nonthyroidal illness, is the term used for patients with low triiodothyronine and thyroxine levels and a normal or low thyroid-stimulating hormone level, but who are clinically euthyroid. This condition is found in critically ill patients or those with severe systemic illness.
| Primary Hypothyroidism (disorders of thyroid gland) | Secondary Hypothyroidism (disorders at hypothalamic-pituitary axis) |
|---|---|
| Autoimmune etiologies (Hashimoto’s) | Panhypopituitarism |
| Thyroiditis (subacute, silent, postpartum)* | Pituitary adenoma |
| Iodine deficiency | Infiltrative causes (e.g., hemochromatosis, sarcoidosis) |
| After ablation (surgical, radioiodine) | |
| After external radiation | Tumors impinging on the hypothalamus |
| Infiltrative disease (lymphoma, sarcoid, amyloidosis, tuberculosis) | History of brain irradiation Infection (e.g., tuberculosis of the brain) |
| Other Causes | |
Congenital Drugs affecting thyroid gland function
Idiopathic | |
Triiodothyronine is the major form of thyroid hormone. The ratio of triiodothyronine to thyroxine released in the blood is about 10:1. Peripherally, triiodothyronine is converted to the active thyroxine, which is three to four times more potent than triiodothyronine. The half-life of triiodothyronine is 7 days, and the half-life of thyroxine is about 1 day.
CLINICAL FEATURES OF HYPOTHYROIDISM
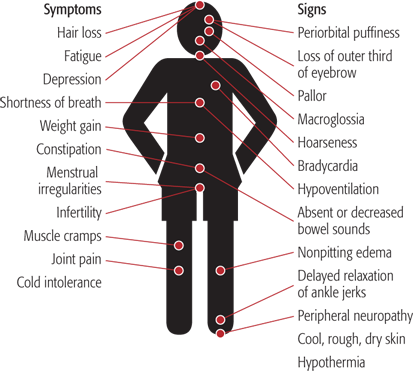
Symptoms can manifest in all organ systems and range in severity based on the degree of hormone deficiency (Table 228-2).
The common clinical features of hypothyroidism are listed in Table 228-2. Additional cardiopulmonary findings include angina, bradycardia, distant heart sounds from pericardial effusion, low voltage on the electrocardiogram, pleural effusions, cardiomyopathy, or hypoventilation.
Figure 228-1 and 228-2 show some characteristic findings of myxedema.
Table 228-3 describes the differences between primary and secondary hypothyroidism.
| Point of Difference | Primary Hypothyroidism | Secondary Hypothyroidism |
|---|---|---|
| Previous thyroid operation | Yes | None |
| Obese | More obese | Less obese |
| Hypothermia | More common | Less common |
| Voice | Coarse | Less coarse |
| Pubic hair | Present | Absent |
| Skin | Dry and coarse | Fine and soft |
| Heart size | Increased | Normal |
| Menses and lactation | Normal | No lactation, amenorrhea |
| Sella turcica size | Normal | May be increased |
| Serum TSH | Increased | Decreased |
| Plasma cortisol | Normal | Decreased |
| Response to TSH | None | Good |
| Response to levothyroxine without steroids | Good | Poor response |
CLINICAL FEATURES OF MYXEDEMA CRISIS
Myxedema crisis is a state of metabolic and multiorgan decompensation characterized by uncorrected hypothyroidism, mental status changes or coma, and hypothermia (usually <35.5°C [95.9°F]).1 In hypothyroid patients, myxedema coma can be precipitated by a number of conditions, including infection, anesthetic agents, cold exposure, trauma, myocardial infarction or congestive heart failure, cerebrovascular accident, GI hemorrhage, metabolic conditions, hypoxia, hypercapnia, hyponatremia, hypoglycemia, surgery, burns, medications (e.g., β-blockers, sedatives, narcotics, phenothiazine, amiodarone), or thyroid medication noncompliance.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree