CHAPTER 3
Hyperventilation
Presentation
The patient is anxious and complains of shortness of breath and an inability to fill the lungs adequately. The patient also may have palpitations, dizziness, intense anxiety, fear, chest or abdominal pain, tingling or numbness around the mouth and fingers, and possibly even flexor spasm of the hands and feet (carpopedal spasm) (Figure 3-1). The patient’s respiratory volume is increased, which may be apparent as increased respiratory rate, increased tidal volume, or frequent sighing. The remainder of the physical examination is normal. The patient’s history may reveal an obvious precipitating emotional cause (such as having been caught stealing or being in the midst of a family quarrel or any other form of stress during work or normal life). The patient may experience alternating periods of hypoventilation or brief periods of apnea as her body tries to allow carbon dioxide (CO2) levels to drift back up to the normal range. If this occurs, the pattern is usually abrupt onset of transient apnea without a drop in O2 saturation, immediately preceded and followed by profound hyperventilation.
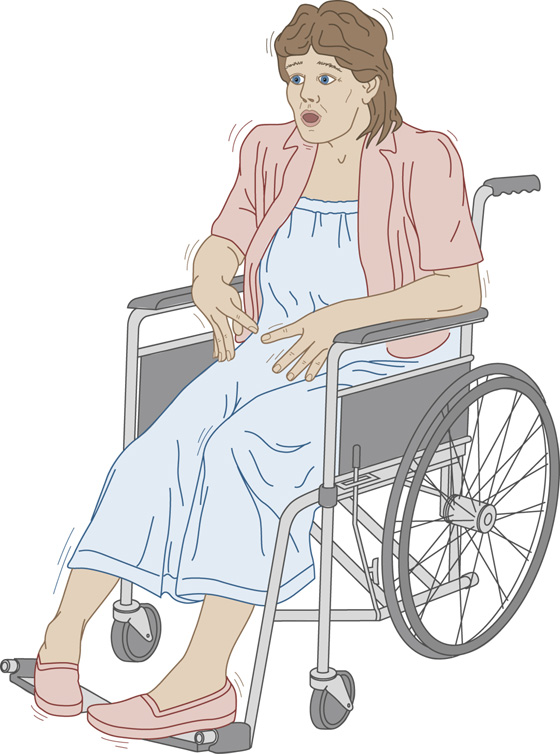
Figure 3-1 The patient experiences anxiety and shortness of breath and feels as though she is unable to fill her lungs, leading to carpopedal spasm.
What To Do:
 Perform a brief physical examination, checking especially that the patient’s mental status is good; there is no unusual breath odor; there are good, equal excursion and breath sounds in both sides of the chest; and there is no swelling, pain, or inflammation of the legs or other risk factors for pulmonary emboli.
Perform a brief physical examination, checking especially that the patient’s mental status is good; there is no unusual breath odor; there are good, equal excursion and breath sounds in both sides of the chest; and there is no swelling, pain, or inflammation of the legs or other risk factors for pulmonary emboli.
 Measure pulse oximetry, which should be between 98% and 100%.
Measure pulse oximetry, which should be between 98% and 100%.
 Calm and reassure the patient. Explain to the patient the cycle in which rapid, deep breathing can cause physical symptoms upsetting enough to cause further rapid, deep breathing. Repeat a cadence (“in… out… in…”) to help the patient voluntarily slow her breathing, or have her voluntarily hold her breath for a while.
Calm and reassure the patient. Explain to the patient the cycle in which rapid, deep breathing can cause physical symptoms upsetting enough to cause further rapid, deep breathing. Repeat a cadence (“in… out… in…”) to help the patient voluntarily slow her breathing, or have her voluntarily hold her breath for a while.
 If the patient cannot reduce her ventilatory rate and volume, provide a length of tubing through which she can breathe (Figure 3-2), or use a reservoir bag with O2, keeping the pulse oximetry monitor on to avoid hypoxia. This will allow the patient to continue moving a large quantity of air but will provide air rich in carbon dioxide (CO2), allowing the blood partial CO2 (PCO2) to rise toward normal. (Carbogen gas [5% CO2] also may be used, if available.) Administration of 50 to 100 mg of hydroxyzine (Vistaril) IM or lorazepam (Ativan) 1 to 2 mg SL, IM, or IV often helps to calm the patient, allowing her to control her respirations.
If the patient cannot reduce her ventilatory rate and volume, provide a length of tubing through which she can breathe (Figure 3-2), or use a reservoir bag with O2, keeping the pulse oximetry monitor on to avoid hypoxia. This will allow the patient to continue moving a large quantity of air but will provide air rich in carbon dioxide (CO2), allowing the blood partial CO2 (PCO2) to rise toward normal. (Carbogen gas [5% CO2] also may be used, if available.) Administration of 50 to 100 mg of hydroxyzine (Vistaril) IM or lorazepam (Ativan) 1 to 2 mg SL, IM, or IV often helps to calm the patient, allowing her to control her respirations.
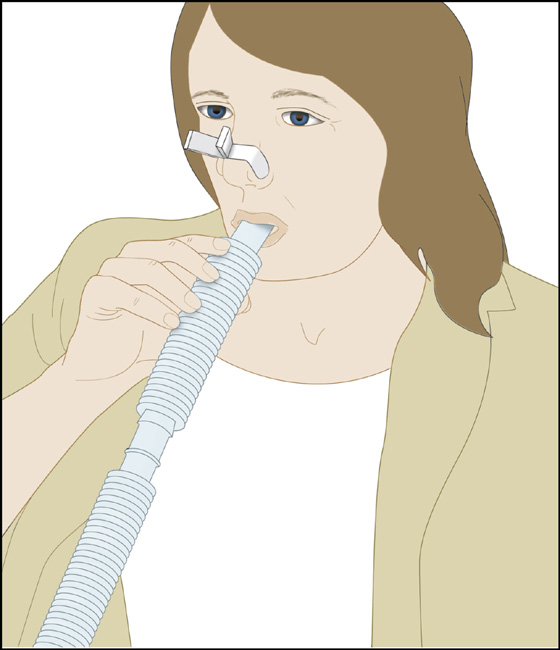
Figure 3-2 Instruct the patient to breathe through a length of tubing to increase the percentage of inspired CO2.
 If these symptoms cannot be reversed and respiratory effort cannot be reduced in this manner within 15 to 20 minutes, double check the diagnosis by obtaining arterial blood gas measurements and looking for a metabolic acidosis or hypoxia indicative of underlying disease.
If these symptoms cannot be reversed and respiratory effort cannot be reduced in this manner within 15 to 20 minutes, double check the diagnosis by obtaining arterial blood gas measurements and looking for a metabolic acidosis or hypoxia indicative of underlying disease.
 Reexamine the patient after hyperventilation is controlled. Identify the psychological stressor that prompted the attack.
Reexamine the patient after hyperventilation is controlled. Identify the psychological stressor that prompted the attack.
 Ensure that the patient understands the hyperventilation syndrome and knows some strategies for breaking the cycle next time. (It may be valuable to have the patient reproduce the symptoms voluntarily). Arrange for follow-up with a primary care physician or psychiatric counselor as needed.
Ensure that the patient understands the hyperventilation syndrome and knows some strategies for breaking the cycle next time. (It may be valuable to have the patient reproduce the symptoms voluntarily). Arrange for follow-up with a primary care physician or psychiatric counselor as needed.
What Not To Do:
 Do not overlook the true medical emergencies, including pneumothorax, asthma, chronic obstructive pulmonary disease (COPD), pneumonia, pulmonary embolus, hyperthyroidism, diabetic ketoacidosis, liver disease, salicylate overdose, sepsis, uremia, substance abuse, sympathomimetic toxidrome, myocardial infarction, congestive heart failure (CHF), and stroke, which also may present with hyperventilation.
Do not overlook the true medical emergencies, including pneumothorax, asthma, chronic obstructive pulmonary disease (COPD), pneumonia, pulmonary embolus, hyperthyroidism, diabetic ketoacidosis, liver disease, salicylate overdose, sepsis, uremia, substance abuse, sympathomimetic toxidrome, myocardial infarction, congestive heart failure (CHF), and stroke, which also may present with hyperventilation.
 Do not use the traditional method of breathing into a paper bag to increase the concentration of inspired CO2. This increases the potential for inadvertently causing hypoxia and is no longer considered to be appropriate therapy.
Do not use the traditional method of breathing into a paper bag to increase the concentration of inspired CO2. This increases the potential for inadvertently causing hypoxia and is no longer considered to be appropriate therapy.
 Do not do an extensive laboratory and imaging study workup when the history and physical examination are convincingly consistent with psychogenic hyperventilation syndrome. However, be suspicious of an organic cause when the patient has risk factors or does not improve as expected.
Do not do an extensive laboratory and imaging study workup when the history and physical examination are convincingly consistent with psychogenic hyperventilation syndrome. However, be suspicious of an organic cause when the patient has risk factors or does not improve as expected.
Discussion
The acute respiratory alkalosis of hyperventilation causes transient imbalances of calcium, potassium, and perhaps other ions, with the net effect of increasing the irritability and spontaneous depolarization of excitable muscles and nerves. First-time victims of the hyperventilation syndrome are the most likely to visit the emergency department or doctor’s office, and this is an excellent time to educate them about its pathophysiology and the prevention of recurrence. Repeat visitors may be overly excitable or may have emotional problems and need counseling.
During recovery after hyperventilation, the transition from hypocapnia to normocapnia is associated with hypoventilation. Be aware that patients may experience significant hypoxemia after hyperventilation. Some investigators believe that there is no benefit in having a patient rebreathe her own exhaled air and that any benefit provided is the result of the reassurance of “instructional manipulation” and the patient’s belief in the treatment rather than the elevated fractional concentration of CO2 in inspired gas (FiCO2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



