Chapter 53
Hypertensive Crisis and Management of Hypertension
Definitions
The classification of hypertension undergoes periodic review by the Joint National Committee (JNC) on Detection, Evaluation, and Treatment of High Blood Pressure. The 2003 report stratifies blood pressure values into four stages: normal, prehypertension, stage I, and stage II (Table 53.1). This report defines patients with a systolic blood pressure (SBP) > 180 mm Hg or diastolic blood pressure (DBP) > 110 mm Hg as having a “hypertensive crisis.” Hypertensive crisis is further stratified to include both hypertensive urgencies and emergencies. A hypertensive urgency is an elevated blood pressure > 180/110 mm Hg without progressive target organ dysfunction. A hypertensive emergency is a blood pressure > 180/110 mm Hg in the presence of progressive target organ dysfunction, where target organs include the brain, heart, retina, and kidney. Hypertensive emergencies usually occur in the presence of blood pressure values > 200/140 mm Hg, though the point at which one develops symptoms is in part dependent on the person’s baseline blood pressure. The diagnosis of hypertensive crisis differs in pregnancy, and the diagnosis and management are reviewed in detail in Chapter 72. It is important to distinguish true emergencies in which rapid blood pressure reduction is necessary from urgent hypertension in which blood pressure elevations can be treated more slowly and with oral medication alone. The diagnosis of a hypertensive emergency does not rest on blood pressure readings alone, but it also requires the concomitant impairment of underlying organ systems. Many clinical situations in which there is a severe elevation of blood pressure warrant the designation of an “emergency” (Box 53.1).
TABLE 53.1
JNC Classification of Blood Pressure
| Classification | Systolic (mm Hg) | Diastolic (mm Hg) |
| Normal | < 120 | < 80 |
| Prehypertension | 120–139 | 80–89 |
| Stage I | 140 ≥ 159 | 90 ≥ 99 |
| Stage II | ≥ 160 | ≥ 100 |
| Crisis | > 180 | > 110 |
JNC, Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure.
From The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure available at www.nhlbi.nih.gov/guidelines/hypertension/jnc7full.htm. Accessed April 12, 2013.
Pathophysiology and Clinical Characteristics
Autoregulation
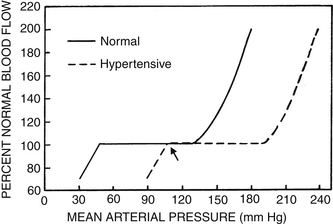
Blood pressure represents a balance between the cardiac output and the peripheral vascular resistance. Hypertensive emergencies are usually due to a marked increase in vascular resistance. Organ systems, in addition to responding to neural and humoral factors affecting blood flow, possess an intrinsic ability to control perfusion known as autoregulation. Autoregulation preserves blood flow over a wide range of blood pressure readings. This phenomenon has been most apparent clinically in the cerebral circulation (Figure 53.1). Chronic, poorly controlled hypertension shifts the lower and upper ends of the autoregulation curve rightward so that, although hypertensive patients tolerate higher blood pressures, the cerebral circulation does not adapt acutely to lower blood pressures that are easily tolerated in normotensive individuals. As a result, when neurologic symptoms result from a hypertensive emergency, it is important to lower blood pressure only by 20% to 25% from presenting levels to avoid precipitating further neurologic deterioration.
Vasospasm
Blood vessels intrinsically constrict in response to increased pressure—that is, they exhibit vasospasm. This may be superseded by a striking decrease in vascular resistance in hypertensive emergencies, causing a “breakthrough” vasodilatation (the rightward end of the autoregulation curve in Figure 53.1) and giving vessels a sausage-like appearance of spasm alternating with dilatation. Vasospasm contributes to organ dysfunction by reducing blood flow. The associated vasodilatation is linked with the formation of edema, thrombus, and fibrinoid necrosis. One clinical correlate of this vascular damage is the appearance of hemorrhages, cotton-wool spots, and exudates in the retina.
Volume Depletion
Patients presenting with a hypertensive emergency are often volume depleted because of the pressure-related natriuresis. This relative hypovolemia activates the renin-angiotensin and the sympathetic nervous systems, both of which potentiate the blood pressure elevation in a vicious cycle. It is important to assess volume status carefully before perfunctorily administering diuretics in a hypertensive emergency.
Diagnostic Evaluation
History and Physical Examination
The evaluation of a patient presenting in a potential hypertensive crisis should be carried out quickly so that therapy can be administered promptly. Certain features in the history and physical examination can help identify hypertensive patients requiring immediate attention from those with elevated blood pressure but who are not in imminent risk of end-organ damage (Boxes 53.2 and 53.3).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree