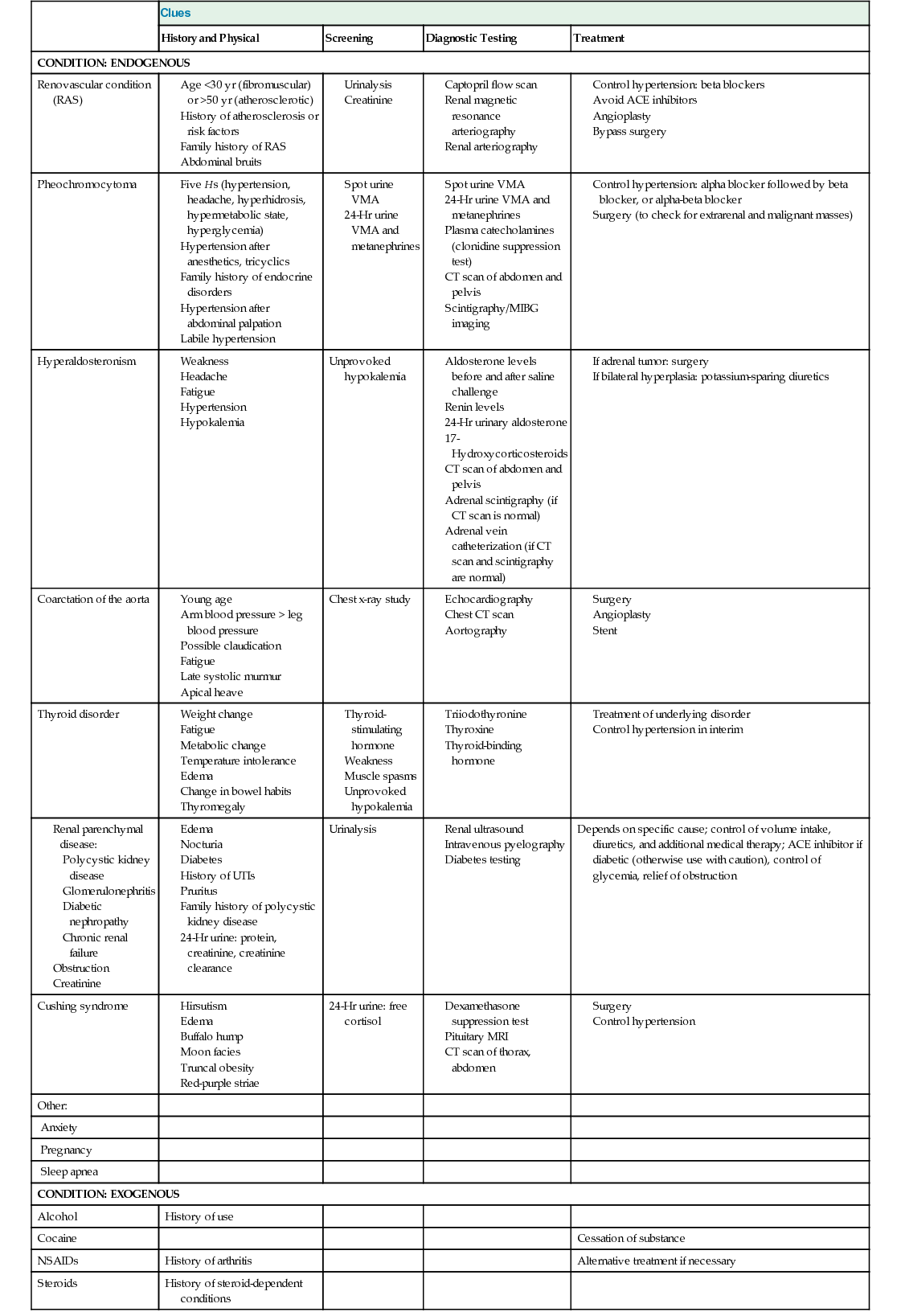
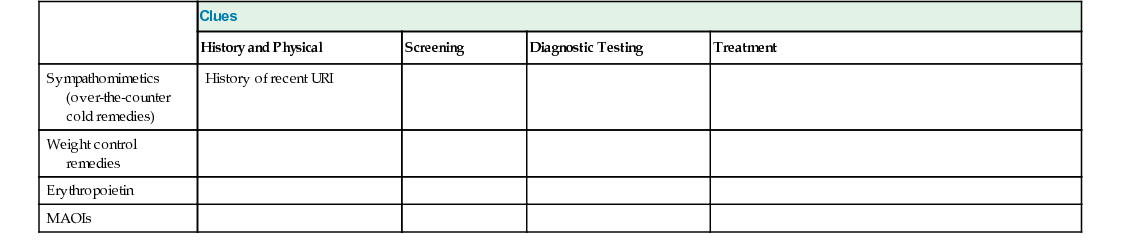
Maryjane Giacalone, Randall M. Zusman Blood pressure is the force in arterial structures created by interplay of flow, volume, and constriction. High blood pressure, or hypertension, has been defined by determining the levels of blood pressure that cause target organ damage, morbidity, and mortality as arterial flow is delivered. It is known that 95% of all hypertension is primary, or essential, hypertension and has no known cause. The remaining 5% is termed secondary hypertension and is directly attributable to structural, circulatory, or chemical abnormalities. In 1972, the National Heart, Lung, and Blood Institute initiated a campaign to improve public awareness of the need for treatment of hypertension. The campaign has been successful in improving awareness and increasing treatment, but control of hypertension in the general population has progressed slowly, reaching 51% in 2009 to 2012.1 Approximately one third of adult Americans have hypertension. Hypertension is a risk factor for coronary artery disease (CAD), heart failure, stroke, peripheral arterial disease, kidney disease, and retinopathy and therefore represents a significant public health threat. In 2011, hypertension was directly responsible for 65,123 deaths and indirectly responsible for 377,258 deaths.2 Research has shown that small gains in the control of hypertension can result in health improvements. Data extrapolated from the Intersalt study have shown that an overall drop of 2 mm Hg in the distribution of blood pressure would result in a 6% annual reduction in stroke, a 4% reduction in CAD, and a 3% reduction in all-cause mortality.3 The most recent data available reveal that although 82% of Americans with high blood pressure are aware of it, 74.7% are undergoing treatment, with 68.9% having adequate blood pressure control.1 As knowledge evolves, guidelines change after reevaluation of past studies and incorporation of findings from new studies to account for different risk levels and treatment regimens. The most recent guidelines from the Eighth Joint National Committee (JNC 8)4 and from the American Society of Hypertension (ASH) and the International Society of Hypertension (ISH)5 have established blood pressure parameters based on these criteria. Both systolic and diastolic blood pressures rise throughout childhood and early and middle adulthood; each is an independent predictor of cardiovascular and cerebrovascular disease, occurring alone or concurrently, in individuals younger than 50 years. The rate of rise in diastolic blood pressure tends to level off or to drop slightly in approximately the fifth decade of life. Systolic blood pressure continues to rise with advancing age, making isolated systolic hypertension more prevalent in the older adult. There is a higher prevalence of hypertension among men until they reach the mid-50s. From 55 to 64, the prevalence of hypertension among men and women is relatively equal. From age 65 to 74, 68% of women have hypertension versus approximately 62% of men, and after 74 years of age, the prevalence increases to 76.4% of men and 79.9% of women.1 In general, people of lower socioeconomic means have a higher prevalence of hypertension. In these groups, poor diet, stress, and poor or less frequent access to health care may play a role in the development of high blood pressure.1 Black adults have higher rates of hypertension than do white or Hispanic adults through age 75. African Americans have a higher incidence of cardiovascular, stroke, and renal complications and have a higher mortality rate related to hypertension than do people of other ethnic backgrounds.2 Enhanced renal sodium reabsorption occurs in 57% of African Americans compared with 27% in other groups. This salt sensitivity contributes to the problem of high blood pressure among African Americans. Obesity, metabolic syndrome, high dietary intake of fat and lower intake of potassium, excessive amount of dietary sodium, physical inactivity, obstructive sleep apnea, excessive alcohol intake, smoking, and stress are associated with the development of hypertension.2 In general, the risk for hypertension is significant for both systolic and diastolic measurements. Prevention, detection, and treatment of hypertension should be public health priorities. The development of hypertension is likely multifactorial and therefore necessitates a coordinated, thoughtful, and individualized approach to diagnosis and treatment. Blood pressure is the product of cardiac output (heart rate, myocardial contractility, and circulating volume and its impact on myocardial stretch) and peripheral resistance (vascular constriction and compliance). Anything that affects any part of this equation can affect blood pressure. In a properly functioning system, feedback loops maintain homeostasis. Primary or essential hypertension is affected by the sympathetic nervous system, either through response to perceived hypovolemia (baroreceptor response) or physical or psychological stressors. Hyperkinetic myocardial muscle, related to neurohormonal stimulation, may cause mild hypertension, primarily in young adults. Hypertension also leads to ventricular hypertrophy. The primary effect of sodium on blood pressure is probably related to excess circulating volume, but sodium may also directly affect hypertrophy, contractility, and vascular resistance. Hypertension associated with salt sensitivity has been postulated to be caused by (1) inability to normally excrete sodium through the kidneys; (2) resetting of the pressure-natriuresis curve, requiring higher blood pressures to maintain normal sodium and water balance; (3) abnormal electrolyte transport, resulting in disturbances in the cytosolic sodium and calcium balance and increased vasoconstriction; or (4) low renin levels, reduced numbers of nephrons, and modified sympathetic nervous system activity.6 Epidemiologic studies generally support a link between higher salt intakes and the prevalence of hypertension.6,7 Age, African-American heritage, diabetes, low renin levels, and nonmodulating hypertension often predict salt sensitivity. Renin is released by the juxtaglomerular apparatus of the kidney in response to a low-flow state (reduced renal perfusion pressure or low circulating intravascular volume), sympathetic nervous system stimulation or catecholamine release, and hypokalemia. Once released, renin acts on angiotensinogen to create angiotensin I. In the pulmonary circulation, angiotensin-converting enzymes (ACEs) change angiotensin I to angiotensin II, a potent vasoconstrictor that over time and with prolonged production causes arterial stiffening and hypertrophy. Vascular hypertrophy results in increased peripheral resistance, depression of angiogenesis, or vessel regression. Angiotensin II also causes aldosterone stimulation, which enhances sodium and water reabsorption from the renal tubules and effectively increases circulating volume. The resulting higher blood pressure should provide feedback to maintain homeostatic responses; however, feedback loops may not work properly in some individuals, allowing higher circulating levels of renin and thus higher blood pressure. There may also be a correlation among obesity, insulin resistance, and hypertension, resulting in impaired salt excretion and enhanced sodium reabsorption, increased sympathetic nervous system activation, and increased angiotensin II and aldosterone production, all of which are associated with higher blood pressure readings.8 The Dietary Approaches to Stop Hypertension (DASH) study showed a relationship between lower potassium intake and hypertension. In this study, it was found that blood pressure also decreased in response to a universally recommended diet that contains generous servings of fruits, vegetables, and low-fat dairy products with reduced sodium and saturated and total fat and increased potassium.7,9 Excessive alcohol consumption (more than two drinks per day) has been associated with hypertension and other cardiovascular risks and should be suspected in individuals who have been resistant to treatment. Alcohol may raise blood pressure by causing increases in sympathetic nervous system activity, activation of the renin-angiotensin system, or decreases in peripheral vascular tone and impairment of baroreceptor effectiveness. Marked increases in blood pressure may occur with acute alcohol withdrawal but are unrelated to mechanisms of chronic hypertension. Overall reduction of alcohol intake results in a lowered blood pressure and overall cardiovascular risks in hypertensive heavy drinkers.10 Blood pressure rises with acute exercise and is most dramatic and serious in those with uncontrolled hypertension. However, regular exercise can be beneficial if the person can adhere to an established exercise routine. The Centers for Disease Control and Prevention recommend regular exercise as an aid in lowering blood pressure. Regular isometric exercise has been shown to prevent the development of hypertension.6 Regular aerobic exercise has been shown to reduce the incidence of cardiovascular events. Secondary hypertension can be ascribed to renal artery stenosis (RAS), pheochromocytoma, hyperaldosteronism, coarctation of the aorta, Cushing syndrome, sleep apnea, and thyroid disease; alcohol and the use of steroids, oral contraceptives (hormone replacement therapy is an infrequent cause), or nonsteroidal anti-inflammatory drugs (NSAIDs) are exogenous causes (Table 122-1).11 Although secondary causes account for approximately 5% to 10% of all hypertension cases, it is important to keep in mind that 5% translates to more than 3 million cases. RAS results in hypertension when there is a 70% to 80% blockage of a renal artery, often activating the renin-angiotensin system. Two different mechanisms have been shown to cause RAS. In individuals younger than 30 years, fibrodysplasia or fibromuscular dysplasia causes tight fibrous bands that alternate with normal or thin tissue along the renal artery, usually the medial portion. Fibrodysplasia affects more women than men. After the age of 50 years, atherosclerosis is the more likely cause of RAS and usually manifests in the proximal artery, extending from aortic plaque. Hypertension from RAS can coexist with essential hypertension; in elderly persons, RAS is likely to be a frequent contributor to hypertension. Angioplasty with or without stenting is the preferred treatment of fibromuscular dysplastic RAS. Atherosclerotic RAS may also be treated with angioplasty, often with stenting if there is elastic recoil in the vessel; an ostial lesion is more difficult to resolve percutaneously. Surgical bypass of the renal artery is another option as long as the individual is healthy enough to undergo surgery.11 Pheochromocytoma is a catecholamine-producing tumor of the adrenal glands and is a fairly rare cause of hypertension (see Chapter 205). A small percentage of these tumors are malignant. Hypertension seen with pheochromocytoma is constant in 50% of cases and labile in the other 50%. Approximately 50% of cases involve the five Hs: hypertension, headache, hyperhidrosis, hypermetabolic state, and hyperglycemia. Bilateral headache, hyperhidrosis, and palpitations occur in 95% of the cases.11 Primary hyperaldosteronism is seen in less than 0.5% of all cases of hypertension and is more common in women. Adrenal adenoma accounts for 70% of all cases of primary hyperaldosteronism and is correctable by surgery. The other 30% results from bilateral adrenal hyperplasia, which must be managed medically. Primary hyperaldosteronism is suspected in patients with unprovoked hypokalemia.11 Coarctation of the aorta (a localized stricture of the aorta) is usually found in youth. It is typified by hypertension in the presence of claudication, delayed femoral pulses, decreased blood pressure in the lower extremities, and notching of ribs on chest x-ray films.12 Treatment usually involves surgical repair, with angioplasty and stenting a less frequent option. Eighty percent of individuals with Cushing syndrome have hypertension (see Chapter 205).12 Cushing syndrome is caused by hypersecretion of glucocorticoids by the adrenal cortex. This hypersecretion results from an adrenal tumor or overstimulation by the anterior pituitary. The use of oral corticosteroids and anabolic steroids may also result in hypertension. All NSAIDs have been associated with hypertension.13 Obstructive sleep apnea, which affects up to 5% of the Western population, is associated with hypertension and is thought to result from a hypoxia-driven sympathetic nervous system discharge. It is more common in individuals with elevated body mass index and appears to plateau at 65 years of age. There is a possible association with leptin, which may be associated with the development of obesity, obstructive sleep apnea, and hypertension.8,11 Use of continuous positive airway pressure (CPAP) resulted in improvement in resistant hypertension over a 12-week study.14 Renal parenchymal disease is associated with the development of hypertension and is also considered a result of hypertension.11 Renal insufficiency is apparent when creatinine levels rise higher than 1.5 mg/dL and the glomerular filtration rate falls to less than 50 mL/min. Renal parenchymal disease encompasses glomerular diseases (e.g., chronic renal failure, systemic lupus erythematosus, nephritis, diabetic nephropathy, glomerulonephritis, renal vasculitis) and interstitial diseases (e.g., polycystic kidney disease, chronic interstitial nephritis). The pathophysiologic mechanism of renal parenchymal disease and hypertension probably involves factors that impair sodium excretion and lead to increased circulating volume. Some studies have found a genetic link to some secondary causes of hypertension, such as hyperaldosteronism. No single significant association has been found for a genetic basis of essential hypertension. Because most patients with hypertension are asymptomatic, the importance of screening cannot be overemphasized. Symptoms of high blood pressure usually occur only after the physical consequences of end organ damage arise. Stroke, CAD or heart failure symptoms, renal dysfunction, retinopathy, and aortic dissection are potential presenting conditions that result from long-standing undiagnosed hypertension. Secondary causes of hypertension are more likely to manifest with early symptoms reflective of the underlying cause, such as diabetic nephropathy and Cushing syndrome. Blood pressure should be measured at each patient visit. The medical history, physical examination, and laboratory data obtained from a patient with high blood pressure should focus on eliciting the presence of cardiovascular risk factors, dysfunction of target organs, and evidence of possible secondary causes of hypertension.5 Cardiac risk factors are assessed in the medical history. The health risks associated with hypertension are compounded by tobacco use, hyperlipidemia, left ventricular hypertrophy, glucose intolerance, and positive family history. In addition, a complete cardiovascular, cerebrovascular, renovascular, endocrine, and family history is documented. Any recent surgical, psychological, social, environmental, or traumatic stress should be elicited. Such events may precipitate a temporary elevation in blood pressure or suggest a secondary cause of hypertension. For example, pheochromocytoma can adversely affect hemodynamic stability during surgery. All over-the-counter and prescribed medications (both currently and formerly used by the patient) should be listed, including nicotine, herbal treatments, steroids, oral contraceptives, NSAIDs, sedatives, sympathomimetics, amphetamines, cyclosporine, erythropoietin, tricyclic antidepressants, monoamine oxidase inhibitors, and alpha- and beta-adrenergic agonists.5 The dosage, frequency, and duration of medications should be documented. A dietary assessment of sodium, cholesterol, fat, and alcohol intake must also be obtained. The provider should elicit clues for potential secondary causes of hypertension, such as sleep apnea (loud snoring, erratic sleep, daytime somnolence), pheochromocytoma (severe headaches, diaphoresis, palpitations), aldosteronism (muscle cramps, weakness, polyuria, polydipsia, nocturia, rhabdomyolysis, paresthesias), mineralocorticoid alteration (licorice intake, chewing tobacco, oral steroid use), and renovascular conditions (hypokalemia). Symptoms indicative of target organ damage must be sought. These symptoms can be neurovascular (transient weakness or blindness, loss of visual acuity, severe headache, confusion, lethargy, seizures), vascular (coarctation, impotence, claudication), cardiovascular (chest pain, dyspnea, palpitations, syncope), and renal (oliguria, hematuria, dysuria).
Hypertension
Definition and Epidemiology
Incidence and Prevalence
Risk Factors
Pathophysiology
Primary Hypertension
Secondary Hypertension
Renal Artery Stenosis.
Pheochromocytoma.
Primary Hyperaldosteronism.
Coarctation of the Aorta.
Cushing Syndrome.
Use of Certain Medications.
Obstructive Sleep Apnea.
Renal Parenchymal Disease.
Genetics.
Clinical Presentation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree