Chapter 99
Head Trauma 
Classification of Head Trauma
Skull Injury
The thin anterior base of the skull is particularly susceptible to injury. The presence of “raccoon’s eyes” (periorbital ecchymoses) or Battle’s sign (retromastoid hematoma) reliably signifies a skull base fracture. CSF otorrhea or rhinorrhea, hemotympanum, or blood in the external auditory meatus without evidence of direct ear trauma is also a hallmark of these fractures. Skull base fractures can involve the carotid canal and result in carotid rupture, dissection, or thrombosis. When this is suspected, cerebral angiography is indicated to evaluate vessel integrity. ![]()
Brain Injury
Focal Brain Injuries
In a study of 1448 patients with mild head injury (defined as a Glasgow Coma Scale [GCS] score of 13 to 15; ![]() Table 99.E1), the most common lesion was a contusion. Contusions often involve the surface of the brain beneath vault fractures, at points where brain the surface collides with bony surfaces of the middle and frontal fossa, or in regions of the cortex where high surface strains are produced by the inner table of the skull. This occurs most commonly in the frontal and temporal lobes but may occur at any site including the brain stem and cerebellum. In patients with focal injuries, the presence of contusion alone tends to portend a good prognosis. Intracerebral hematomas result from torn blood vessels in deeper brain structures. They are not contiguous with the cortical surface and typically occur in the deep white matter of the frontal and temporal lobes. Injuries in which the pial surface is violated with parenchymal disruption are termed cerebral lacerations.
Table 99.E1), the most common lesion was a contusion. Contusions often involve the surface of the brain beneath vault fractures, at points where brain the surface collides with bony surfaces of the middle and frontal fossa, or in regions of the cortex where high surface strains are produced by the inner table of the skull. This occurs most commonly in the frontal and temporal lobes but may occur at any site including the brain stem and cerebellum. In patients with focal injuries, the presence of contusion alone tends to portend a good prognosis. Intracerebral hematomas result from torn blood vessels in deeper brain structures. They are not contiguous with the cortical surface and typically occur in the deep white matter of the frontal and temporal lobes. Injuries in which the pial surface is violated with parenchymal disruption are termed cerebral lacerations.
Diffuse Brain Injury
Concussion is a mild form of global neurologic dysfunction. The exact mechanism and pathophysiology of concussion remain an enigma. The neurologic disturbances seen in concussive syndromes may relate to the magnitude and site of head injury. Although concussion may or may not be associated with loss of consciousness, amnestic periods and long-term higher cognitive deficits have been reported. In classic concussions (i.e., those associated with a “reversible” neurologic deficit and temporary loss of consciousness), it is theorized that there is temporary neurophysiologic perturbations within the reticular activating system. Although there are no grossly evident radiographic or neuropathologic lesions, neurochemical and ultrastructural changes have been observed.
TABLE 99.E1
Scoring for Glasgow Coma Scale∗
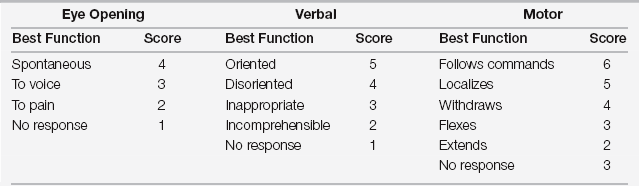
∗The Glasgow Coma Scale is calculated as the sum of the highest scores from each of the three categories listed. The maximal score is 15 and minimal score is 3.
Diffuse axonal injury (DAI) is the most severe form of diffuse brain injury. When the tensile strain from angular acceleration and deceleration forces act on the brain parenchyma, axons and small vessels tear. Characteristically, the head-injured patient presents with a low GCS score (3 to 8), but no gross neuroradiographic abnormalities are evident. Placement of an ICP monitor may reveal intracranial hypertension that may require intensive medical therapy over the following days (see Chapter 41). ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



