INTRODUCTION AND EPIDEMIOLOGY
Minor head injury in children is responsible for almost 400,000 ED visits each year,1 with children 0 to 4 years of age most commonly affected. Of all children with minor head injury coming to the ED, it is estimated that about 5% have intracranial injury,2 and <1% of those with intracranial injury require neurosurgical intervention.3,4
Given the rarity with which head-injured children require intervention, the diagnostic challenge is to distinguish the small subset of seriously injured children, while minimizing evaluation of those at low risk of significant intracranial injury. Therefore, careful risk stratification of children with minor head injury is important for safe and efficient medical care.
This chapter focuses on evaluation of children with minor head injury and concussion, as well as the treatment of children in whom significant intracranial injuries are identified.
The definition of minor head injury varies in the literature. The American Academy of Pediatrics defines children with minor head injury as “those who have normal mental status at the initial examination, who have no abnormal or focal findings on neurologic (including funduscopic) examination, and who have no physical evidence of skull fracture.”5 The Glasgow Coma Scale (GCS; Table 138-1), or its derivative for younger, preverbal infants and toddlers, is often used to determine the severity of head injury. Head injuries resulting in a GCS score of ≤8 are severe, those with scores of 9 to 13 are moderate, and those with scores of 14 or 15 are mild.
| Response | Adults | Infants | Score |
|---|---|---|---|
| Eye opening | Spontaneous To voice To pain No response | Spontaneous To voice To pain No response | 4 3 2 1 |
| Verbal response | Oriented Disoriented Inappropriate words Incomprehensible No response | Coos, babbles Irritable Cries to pain Moans to pain No response | 5 4 3 2 1 |
| Motor response | Obeys commands Localizes pain Withdraws to pain Decorticate posture Decerebrate posture No response | Makes normal spontaneous movements Withdraws to touch Withdraws to pain Decorticate posture Decerebrate posture No response | 6 5 4 3 2 1 |
PATHOPHYSIOLOGY
Head trauma is classified as blunt or penetrating based on the mechanism of injury. In children, the vast majority of head trauma is caused by blunt force with the underlying mechanism varying according to the age of the patient. In younger children, the most common causes of head trauma are falls and assaults/child abuse.6 In fact, in children under 2 years of age, nonaccidental trauma is the leading cause of death due to head trauma. In older children, falls, sports and recreation, assault, and, increasingly, motor vehicle collisions are more common. Penetrating injuries are most frequently related to dog bites in infants or gunshot wounds in older children. In the largest study of pediatric minor head injury to date, including over 42,000 patients, radiographically documented intracranial injuries were found in approximately 1.8% of children with minor head injury who presented to the ED for evaluation, and only 0.9% required intervention.4 This is a lower number than cited in prior studies, likely due to the inclusion and clinical follow-up of lower-risk children not undergoing CT. The true incidence of intracranial injuries is probably even lower, because many children with mild injuries do not present to the ED.
The pattern of injury is different in children compared to adults. In children, diffuse injuries are proportionally more common, and in adults, focal injuries such as epidural and subdural hematomas and cerebral contusions are more common.6
The differences in brain development and pediatric anatomy explain the specific pattern of childhood injuries compared to adults. In blunt head injury, rotation of the brain around its center of gravity leads to more diffuse injuries (diffuse axonal injury and subdural hematoma), whereas linear forces are generally less damaging to the brain and cause local (coup and contrecoup injury) rather than diffuse injury. The type and severity of the injury are determined both by the type of deceleration and its magnitude.7 Younger age is a significant risk factor for intracranial injury. Even among infants, the greatest risk for intracranial injury is in children under 3 months of age.2
More details of physiology are discussed in chapter 257, “Head Trauma.”
Skull fractures can involve the calvarium or the base of the skull. The presence of skull fractures is a risk factor for underlying brain injury in infants under 2 years of age (Figures 138-1 and 138-2).4
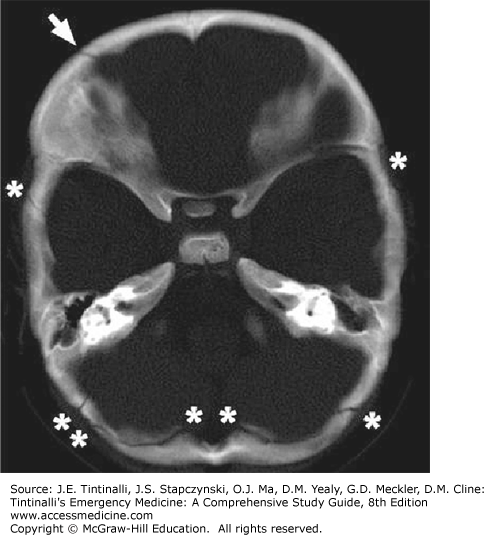
FIGURE 138-1.
Linear fracture seen on CT. Arrow indicates skull fracture, and asterisks indicate normal cranial suture lines. [Image used with permission of Joseph Piatt, Jr., MD, Division of Neurosurgery, A. I. duPont Hospital for Children, Wilmington, Delaware; Departments of Neurological Surgery and Pediatrics, Thomas Jefferson University, Philadelphia, Pennsylvania.]
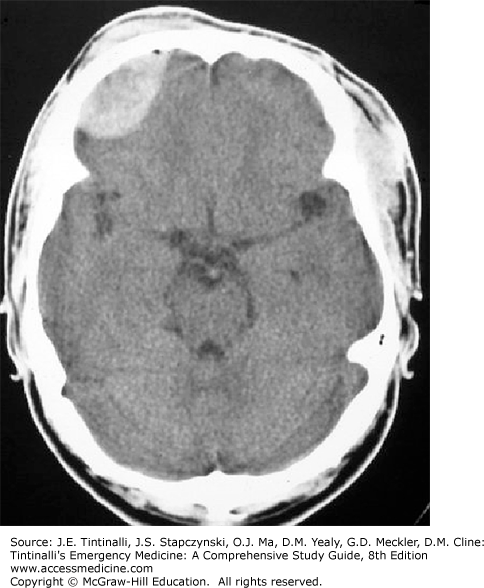
FIGURE 138-2.
Open skull fracture with underlying cerebral contusion. This injury was sustained from a fall of two stories. [Image used with permission of Joseph Piatt, Jr., MD, Division of Neurosurgery, A. I. duPont Hospital for Children, Wilmington, Delaware; Departments of Neurological Surgery and Pediatrics, Thomas Jefferson University, Philadelphia, Pennsylvania.]
However, significant brain injury can occur in the absence of skull fractures in 50% of cases.8 Plain films of the skull should therefore not be obtained as a replacement for CT to evaluate for underlying brain injury.9 Depressed skull fractures occur in response to the application of significant force and require neurosurgical consultation, as surgical elevation is often required. Compared to adults, skull fractures in children are more common but less frequently associated with underlying brain injury.6
A growing fracture can occur when the leptomeninges are torn beneath the fracture, allowing for the formation of a cerebrospinal fluid leptomeningeal cyst that forces apart the fracture edges and leads to nonunion. Growing skull fractures typically present weeks to months following an injury resulting in skull fracture. This rare complication is unique to infants and requires neurosurgical repair.
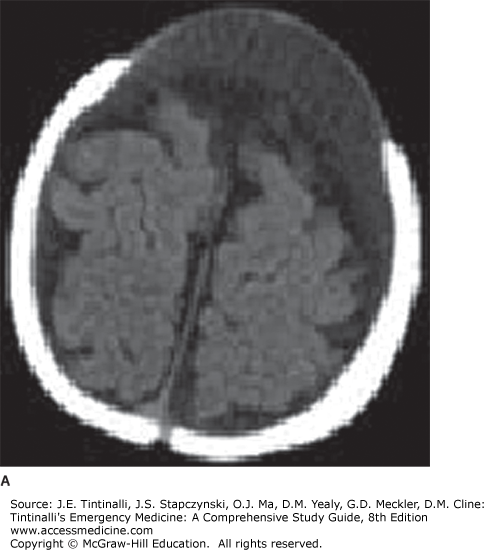
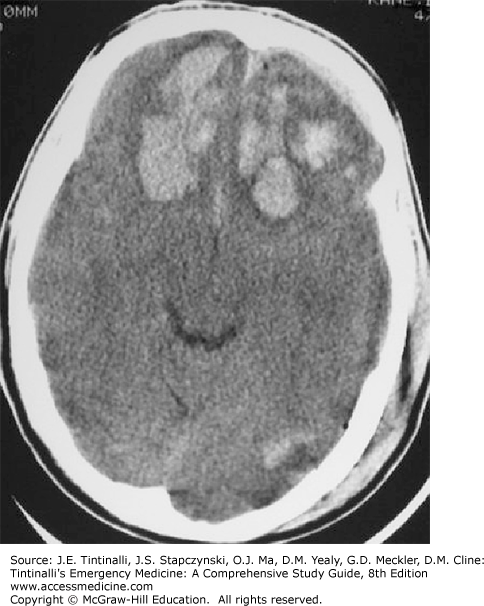
An epidural hematoma (Figure 138-3) is a collection of blood between the inner skull and the dura and can occur from rapid arterial bleeding from the middle meningeal artery or the dural or diploic vasculature.
The classic presentation is a lucid interval after head trauma followed by rapid deterioration. The presence of a bi-convex hyperdense extra-axial lesion that does not cross the suture lines is indicative of an epidural hematoma on CT.10 The long-term prognosis depends on the preoperative GCS and the extent of other underlying brain injury,11 but is generally good if surgical evacuation can be undertaken in a timely manner.
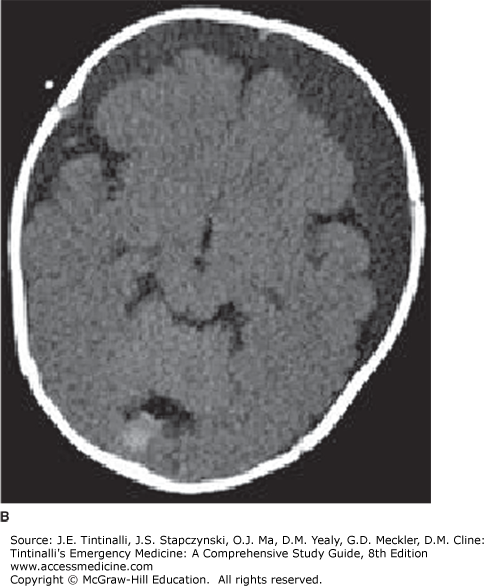
Subdural hematomas (Figure 138-4), located between the arachnoid and the internal dural layer, are more common than epidural hematomas, particularly in infants and younger children. Subdural hematomas are caused by tearing of the subdural veins, are often extensive and bilateral (80% of cases), are frequently associated with underlying brain injury, and have a worse prognosis than epidural hematomas.
Radiographically, a subdural hematoma appears as a crescent-shaped fluid collection with the concavity facing the brain surface. Immediately after the injury, the subdural hematoma appears more dense (brighter white) than adjacent brain tissue. Due to the metabolism of blood products within the hematoma, its radiographic appearance changes over time. In the subacute phase (1 to 3 weeks after injury), the hematoma progressively assumes the same density of the brain tissue and can thus be difficult to recognize. Flattening of the sulci and the presence of a mass effect are indirect evidence of the presence of a subdural hematoma. Subsequently, in the chronic phase, the hematoma appears as a hypodense fluid collection, with a density similar to cerebrospinal fluid.10 In infants, loss of gray-white matter differentiation and diffuse hypodensity has been described with subdural hematoma.7
Cerebral contusions (Figure 138-5) are located in the cortex underlying the area of direct impact of a significant force (coup lesions) or on the opposite side (contrecoup lesions) where the brain has struck the cranial surface.
The severity ranges from minor CT findings in an asymptomatic patient to severe brain edema. On CT, the presence of ill-defined hyperdense areas within the cortex of the frontal and temporal lobe represent parenchymal contusions.
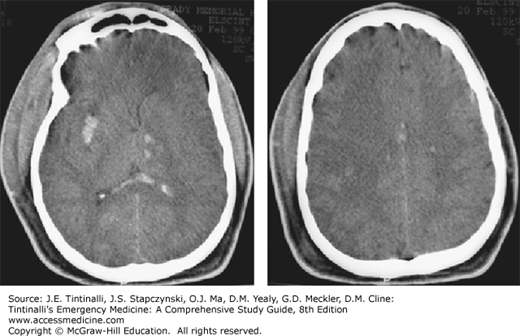
Traumatic subarachnoid hemorrhage is often associated with significant trauma and diffuse axonal injury (Figures 138-6 and 138-7). Infants more commonly present with diffuse injury and cerebral edema compared to adults because developmental differences render them susceptible to rotational and deceleration forces. Clinically, the child with diffuse axonal injury presents with a profoundly depressed level of consciousness. Radiographic findings on CT may be minimal in the acute setting. MRI is more sensitive in the detection of diffuse axonal injury, which can be both hemorrhagic and nonhemorrhagic.10