
Hand Injuries
David Q. Bell and Douglas Doehrman
Hand injuries account for 5% to 20% of emergency department (ED) visits (1). The outcome depends on accurate assessment of the injury, appropriate initial management, and prompt recognition of those injuries that require immediate specialty consultation or outpatient referral.
An understanding of the anatomy and terminology of the hand is crucial for the evaluation and treatment of hand injuries. The surfaces of the hand and digits are referred to as dorsal, palmar, ulnar, and radial. The palmar surface anatomy is shown in Figure 41.1. Finger motion is described as extension, flexion, abduction, and adduction. Motion is related to the midline of the long finger. The thumb can perform opposition to touch the pads of all the fingers.
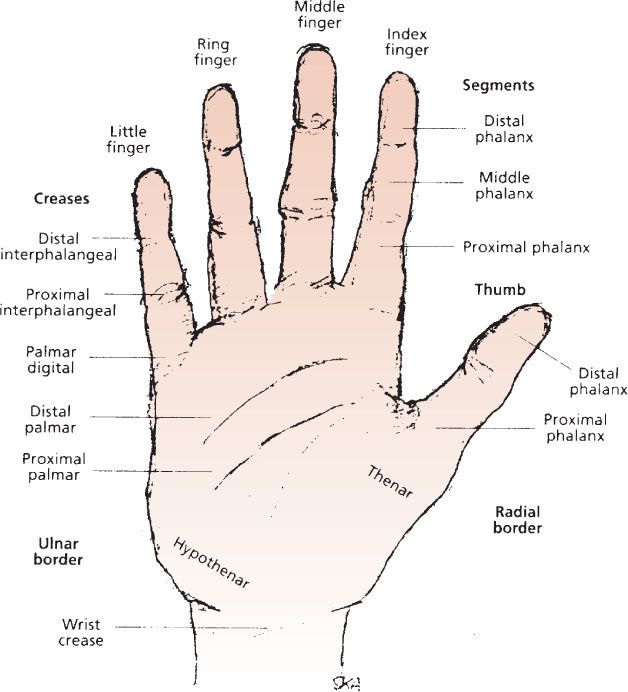
FIGURE 41.1 Palmar (volar) surface anatomy.
Muscles that control hand motions are divided into flexors and extensors, each of which may be intrinsic or extrinsic to the hand. The intrinsic muscles have their origins and insertions within the hand. The thenar muscles and adductor pollicis are tested by flexing, adducting, and abducting the thumb. The four dorsal and three palmar interossei originate from the lateral metacarpals and insert on the base of the proximal phalanges and extensor expansion (Fig. 41.2). Motor function of the lumbricals and interossei is tested by placing the hand on a flat surface and moving each finger from side to side. The hypothenar muscles are tested by adducting the little finger.
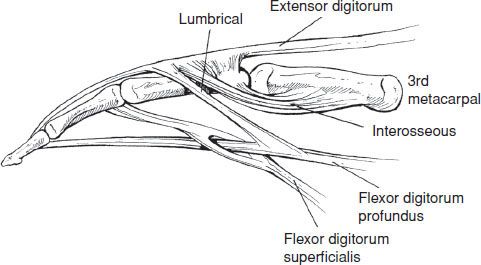
FIGURE 41.2 Musculotendinous anatomy of the finger.
The extrinsic muscles have their origins in the forearm. The extensor tendons pass under the extensor retinaculum at the wrist. The extensor tendons produce extension of the fingers by their dorsal attachments on the metacarpals and phalanges. Because there are many interconnections between the extensors, care must be taken in evaluating suspected extensor tendon injuries. Normal movement may be preserved via these interconnecting bands. The extrinsic finger flexors enter the hand via the carpal tunnel. The flexor pollicis longus of the thumb is tested by flexing the thumb against resistance. All four fingers have two flexors. The flexor digitorum superficialis (FDS) attaches to the base of the middle phalanx. The flexor digitorum profundus (FDP) attaches at the base of the distal phalanx. The FDS and FDP tendons of each finger are tested individually by flexing the distal interphalangeal (DIP) joint and the proximal interphalangeal (PIP) joint against resistance with the other fingers held in extension. It is important to test both FDS and FDP function in each finger individually to avoid missing an isolated injury.
The median, radial, and ulnar nerves provide the sensory and motor innervation to the hand. The sensory innervation of the hand is detailed in Figure 41.3. The median nerve supplies motor function to the extrinsic flexors of the hand, the intrinsic thenar muscles, and the first and second lumbricals. The ulnar nerve innervates the flexor carpi ulnaris, the ulnar portion of the FDP, and all the remaining intrinsic muscles of the hand. The radial nerve innervates those muscles of the forearm that provide extension of the wrist and digits, as well as extension and abduction of the thumb.
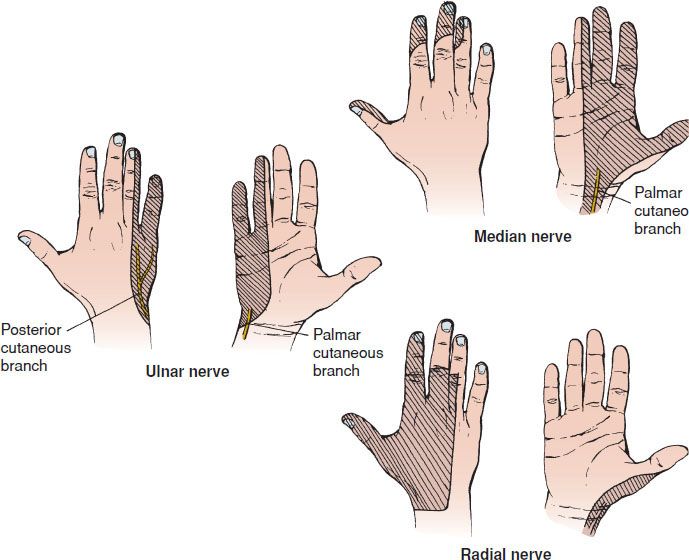
FIGURE 41.3 Sensory innervation of the hand.
The arterial supply to the hand is provided by the radial and ulnar arteries. The radial artery terminates where the deep palmar arch and the ulnar artery forms the superficial palmar arch. Extensive collateralization occurs between the two vessels. The four common digital arteries arise from the superficial palmar arch where they divide to form the proper digital arteries.
The thick palmar skin is tightly adherent to the deep fascia of the palm. The dorsal skin of the hand is thin and supple with little underlying adipose or fibrous tissue. These qualities cause edema from hand injuries to be more pronounced on the dorsal surface.
Knowledge of fingertip and nail bed anatomy is essential when evaluating distal finger injuries (eFig. 41.1).
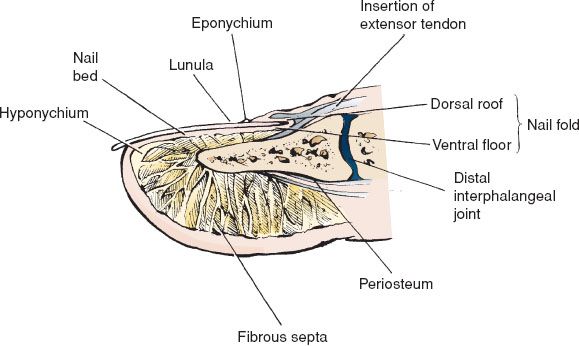
eFIGURE 41.1 Fingertip and nail bed anatomy.
CLINICAL PRESENTATION
Patients with acute hand injuries present with varying degrees of pain, swelling, and loss of function. Injuries resulting from repetitive motions and systemic or bone diseases usually present more insidiously with chronic waxing and waning symptoms (see Chapter 145).
Patients with metacarpal injuries generally present with pain, swelling, and limitation of movement. Finding the place of maximal tenderness or deformity will help localize the area of injury. In patients with a metacarpal head fracture, axial compression of the extended digit causes severe discomfort. In patients with a metacarpal base fracture, movement of the wrist or longitudinal compression exacerbates the pain. Metacarpal fractures 2 through 5 are classified together. They are divided into head, neck, shaft, and base fractures. First metacarpal fractures are classified separately as shaft fractures and extra-articular or intra-articular base fractures.
Patients with phalangeal injuries present with varying degrees of pain, limited mobility, and deformity of the involved digit.
Hand lacerations range from clean, superficial wounds to severely contaminated crush injuries or amputations. Associated tendon injuries may cause a partial or complete loss of motor function, and injury to surrounding nerves may result in loss of both motor and sensory function.
Patients with fingertip injuries may present with a minor laceration or a severe injury with significant tissue loss or destruction.
DIFFERENTIAL DIAGNOSIS
Metacarpal injuries include fractures, dislocations, or combinations of the two. If an injury is associated with an open wound, the possibility of infection of the underlying structures should be considered (see Chapter 147). The differential diagnosis of acute phalangeal injuries includes fractures, fracture–dislocations, and ligamentous injuries.
The diagnostic challenge of hand lacerations lies in the detection of underlying injuries that may threaten the function of the hand. Tendon lacerations and injuries to bones, joints, nerves, and arteries must be excluded by examination, radiography, and direct exploration of the wound. Older wounds must be evaluated for the possibility of a developing deep space infection. Wounds that do not heal or have persistent pain with movement should be evaluated for an occult foreign body.
ED EVALUATION
Evaluation and treatment of potentially life-threatening injuries should precede any evaluation of the hand. Once evaluation and treatment have been accomplished, assessment of the hand can begin. Direct pressure should be used to control bleeding. In rare instances when direct pressure is not sufficient, careful and intermittent use of a tourniquet will usually gain control of the bleeding and allow adequate visualization of the wound. Blind clamping of bleeding vessels should be avoided, because adjacent nerves and tendons may be injured.
A focused history is essential. Important historical information includes the patient’s age, dominant hand, occupation, prior hand injuries, previous tetanus immunization, and past medical history. Details of the traumatic event should include time and mechanism of the injury, position of the hand during the accident, and treatment administered before arrival.
All dressings should be removed to completely expose the hand. Rings should be removed, because swelling may create a tourniquet effect. The location and type of wounds, skin loss, ecchymosis, pallor, swelling, and the resting attitude of the digits should be noted. The normal resting cascade of the fingers reveals progressive flexion of the digits from the index to the little finger. The normal resting cascade is generally symmetric.
Alterations in the resting cascade may indicate an underlying tendon injury. For example, a flexor tendon injury may appear as an extended digit because of unopposed extensor tone, and an extensor tendon injury may reveal a flexion deformity. The hand should also be observed during passive flexion and extension of the wrist. With wrist extension, the fingers naturally assume a flexed posture. With wrist flexion, the fingers will passively extend (2). This method may be particularly helpful in evaluating children or uncooperative patients. Emergency physicians may misdiagnose up to 35% of tendon injuries based on clinical examination alone (3). Bedside ultrasound has been shown to aid in the detection of tendon injuries (4).
The hand should be carefully palpated to identify areas of tenderness, deformity, and crepitus. In patients with phalangeal or metacarpal fractures, the presence of rotational malalignment must be sought. Rotational deformity may be diagnosed by having the patient make a fist. Normally, all of the fingers point to a single spot on the scaphoid (eFig. 41.2).
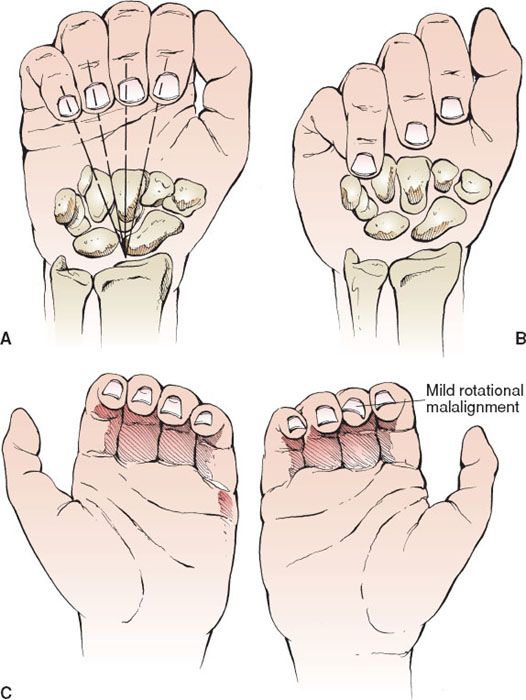
eFIGURE 41.2 Clinical signs of rotational malalignment. A: Normally, all fingers point to the same spot on the scaphoid when making a fist. B: With rotational malalignment, the affected finger does not point to the scaphoid. C: Loss of the usual parallel relationship of the finger nails with rotational malalignment. (Redrawn from Simon RR, Koenigsknecht SJ. Emergency Orthopedics: The Extremities. 3rd ed. Norwalk, CT: Appleton and Lange; 1995:64.)
Nerve integrity is assessed by testing both sensory and motor functions. Sensation should always be evaluated and documented before the administration of any anesthetic agent. Digital nerve sensory function is best assessed by two-point tactile discrimination. The volar lateral aspects of the digits are lightly stroked in a longitudinal direction at the two points. Comparison with the opposite hand may be helpful. Motor function of the median nerve is tested by touching the thumb to the little finger and elevating the thumb of the pronated hand as the hand is lying on a flat surface. Radial nerve function is checked by extending the wrist and fingers. Ulnar function is tested by spreading the fingers apart against resistance. Emergency physicians may fail to identify up to 55% of nerve injuries (3).
In young children or uncooperative patients, it can be difficult to accurately perform two-point tactile discrimination. In these circumstances, nerve integrity can be assessed by testing for the presence of sympathetically mediated skin wrinkling and skin sweating. Soaking the hand in warm water for 30 minutes should cause wrinkling of the normally innervated skin. Skin sweating can be assessed by stroking the digit with a smooth object (such as the barrel of a pen). Less resistance (shown by loss of sweating) should be noted over the denervated area.
Vascular integrity of the hand is evaluated by looking for pallor, noting skin temperature, assessing capillary refill, and palpating the ulnar and radial arteries at the wrist (2). The Allen test is utilized to evaluate the patency of the radial and ulnar arteries and the palmar arches. The test is performed by having the patient clench the fist to exsanguinate the hand while the examiner occludes the radial and ulnar arteries. When the hand is blanched, pressure over one of the arteries is released. Normal hand color should return in 3 to 5 seconds. The test is repeated, releasing the other artery.
Testing for tendon integrity is another important aspect of the hand examination. When evaluating finger lacerations, the digit should be moved through a full range of motion against light resistance. A tendon laceration may be proximal or distal to the skin wound depending on the position of the hand when the injury occurred. Partial tendon lacerations may have full function, so these lacerations are easily missed. If there is any concern about the possibility of a foreign body or injury to a deep structure, the wound should be evaluated under bright lighting with a dry field. A bloodless field is obtained by first emptying the veins. The veins are emptied by elevating the extremity and inflating a proximally placed blood pressure cuff above systolic pressure. The blood pressure cuff may be left in place for up to 20 minutes as the wound is explored. A dry field can be obtained in individual digits by placing a sterile glove on the injured hand, cutting off the tip of the glove on the injured finger, and rolling the end of the cut glove proximally to simultaneously exsanguinate and tourniquet the finger.
Radiographs of the hand should be obtained whenever the mechanism might result in fracture, joint instability, or a retained foreign body. If a thumb injury is suspected, posteroanterior (PA) and lateral views of the thumb should be obtained, because the thumb is not adequately visualized on standard hand radiographs. If there is suspicion of a foreign body despite negative plain radiographs, ultrasonography, computed tomography, or magnetic resonance imaging may be required to visualize the object (5).
KEY TESTING
• Assess sensation and motor function in the distribution of the medial, ulnar, and radial nerves. Document two-point discrimination when possible.
• Examine wounds in a clean bloodless field through passive range of motion to evaluate for tendon injury.
• Assess both flexor digitorum superficialis and flexor digitorum profundus integrity.
• Evaluate and document vascular integrity of hands and digits.
• Evaluate for rotational deformity.
ED MANAGEMENT
ED management of hand injuries includes application of ice and elevation of the extremity to reduce swelling. The liberal use of analgesics is also recommended. IV antibiotics are indicated for tendon lacerations, open fractures, dislocations, and severely contaminated or infected wounds. Tetanus immunization should be updated appropriately. Open wounds should be covered with a sterile, moist gauze dressing pending radiographs, surgical consultation, or wound closure. Suspected fractures should be temporarily immobilized with a bulky hand dressing or a splint while awaiting radiographs, reduction, or surgical consultation.
The patient’s disposition depends on the nature and severity of the injury. A hand surgeon should evaluate the patient in the ED when there is an irreducible dislocation, any vascular injury with ischemia, or grossly contaminated open wounds. The remainder of most fractures, tendon, nerve, and soft tissue injuries can be splinted and seen on a prioritized basis. There are regional variations in the aggressiveness with which hand surgery consultants perform primary repair of injuries in the ED.
Anesthetic Techniques
Anesthesia for the evaluation and repair of hand injuries can be provided by a local infiltration digital nerve block or a regional nerve block at the wrist. A hematoma block is useful for the reduction of metacarpal fractures (6). Lidocaine without epinephrine should be used in 2% concentration for nerve blocks and in 1% or 2% concentration for infiltration. Lidocaine with epinephrine can be safely used for digital blocks. Lidocaine with epinephrine has the advantages of providing improved hemostasis and a longer duration of anesthesia than lidocaine alone (7).
A digital block is performed by injecting 2 to 3 mL of local anesthetic at the medial and lateral aspects of the base of the proximal phalanx. Infiltration of the proximal dorsal surface of the digit is also required to anesthetize the dorsal digital nerve. Complete anesthesia usually requires 5 to 10 minutes. Bupivacaine may be a more appropriate agent for digital nerve blocks. It can provide anesthesia for up to 8 hours and is ideal for situations where prolonged anesthesia is preferred (8). Circumferential infiltration of the digit is not recommended, because circumferential infiltration may result in distal necrosis. Small randomized controlled studies have demonstrated that a single volar injection method achieves similar anesthesia with less patient discomfort. A 25-gauge needle should be injected at the volar metacarpophalangeal (MCP) skin crease while the physician is slightly pinching the proximal aspect of the proximal phalanx. The needle should be advanced until it hits the bone then retracted 1 to 2 mm; 2 to 3 cc of anesthetic should be injected (9).
Regional nerve blocks at the wrist can anesthetize the median, ulnar, and radial nerves. A median nerve block is performed by injecting 5 mL of local anesthetic 1 cm proximal to the distal wrist flexion crease, radial and deep to the palmaris longus tendon, or deep to the ulnar aspect of the flexor carpi radialis tendon in those individuals lacking a palmaris longus tendon. An ulnar nerve block is accomplished by injecting 5 mL of local anesthetic 1 cm proximal to the distal wrist flexion crease just radial and deep to the flexor carpi ulnaris tendon. The ulnar artery at this level lies in close proximity to the ulnar nerve. Aspiration before injection is important to avoid intravascular injection of the anesthetic. The dorsal sensory branch of the ulnar nerve is blocked by subcutaneous infiltration of anesthetic just distal to the ulnar styloid. A radial nerve block is performed by subcutaneous infiltration of 5 mL of anesthetic agent just distal to the radial styloid. Ultrasound is a useful adjunct to performing forearm nerve blocks and is within the scope of practice for an appropriately trained emergency physician to perform (9). A hematoma block is performed by injecting a local anesthetic into the hematoma surrounding a fracture. A 27-gauge needle is inserted over the fracture site. When blood is aspirated into the syringe, indicating correct needle placement, 5 to 10 mL of anesthetic is injected. Ten minutes are often required before complete anesthesia is obtained with regional and hematoma nerve blocks.
Metacarpal Neck Fractures
Most commonly seen in the fifth metacarpal (i.e., boxer fracture), neck fractures are usually the result of striking an object with a closed fist. Metacarpal neck fractures are easily reduced, but reduction may be difficult to maintain. Because metacarpals 2 and 3 are relatively fixed and immobile, reduction of these fractures must be nearly anatomic. Any volar angulation will project the metacarpal head into the palm and impair grip strength. Greater angulation is acceptable in metacarpals 4 and 5. These digits have greater mobility, and they can move dorsally without impairment of grip strength. Most hand surgeons will allow up to 40 degrees of angulation in fractures of the fifth metacarpal neck and 20 degrees of angulation in fractures of the fourth metacarpal neck. In contrast, as little as 10 degrees of angulation is unacceptable for metacarpals 2 and 3. Even minor rotational deformity can lead to impaired grip strength and requires referral to hand surgery for possible surgical correction.
The technique for reduction of metacarpal neck fractures is the same regardless of which metacarpal is fractured. Surgical consultation is recommended before reduction of metacarpals 2 and 3, because some surgeons prefer operative fixation. After adequate anesthesia has been obtained, the MCP and PIP joints are flexed to 90 degrees. Pressure is applied to the PIP joint in a dorsal direction to force the metacarpal head into its normal position. Stabilizing volar pressure should be applied with the physician’s other thumb just proximal to the fracture site (Fig. 41.4). If reduction is difficult, longitudinal distraction may be needed to disimpact the fracture before successful reduction can be accomplished.
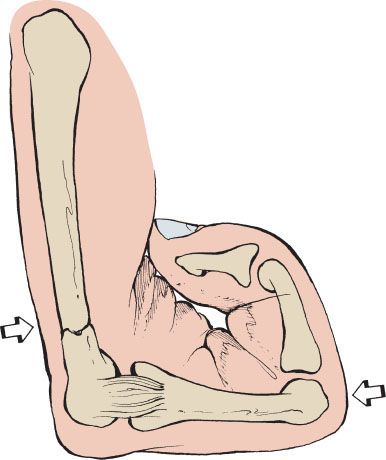
FIGURE 41.4 The 90–90 method of reduction for metacarpal neck fractures.









