TEG graph and annotation.
The reaction time (R-time) depicts the time for fibrin strands to form. It is decreased in hypercoagulable states such as pregnancy. A prolonged R-time may reflect decreased or dysfunctional coagulation factors leading to a delay in the formation of thrombin or fibrin. Consideration should be given to administer FFP for correction. A prolonged R-time may also reflect heparin activity, and this may be further evaluated using a heparinase cup that will remove the heparin effect on the sample.
The maximum amplitude (MA) represents clot strength with the amplitude of pin oscillation increasing with clot strength (Figure 21.1). The major contributors to clot strength are platelets (80–90%) and fibrinogen (10–20%), which binds the platelets together. Therefore, MA gives an indication as to the function of platelets present in the sample. A low MA value is indicative of insufficient platelet–fibrin clot formation due to poor platelet function, low platelet count, or low fibrinogen levels or function. The most common treatment of a low MA in a bleeding patient is transfusion of platelets. The amount of platelets required to reverse bleeding depends on the magnitude of the abnormality and on the patient’s overall status.
Accepted non-pregnant reference ranges for R-time are 4–8 minutes and for MA, 55–73 mm. Studies on pregnant women reflect the hypercoagulable state of pregnancy; R-time values are shorter and MA values are higher, but further work is needed to define pregnancy values.
A platelet function analyzer (PFA-100) can also measure platelet function. This tests platelet activation and aggregation. Experience in obstetrics is limited and expert advice in the use and interpretation of samples is essential.
Clinical example of the use of TEG
A 24-year-old primigravida presented to labour ward with PV bleeding at 24 weeks’ gestation. Her blood pressure was 150/110 and scans revealed fetal demise. Bleeding from venepuncture sites raised the clinical suspicion of DIC. TEG (Figure 21.2) was used as a rapid laboratory assessment and confirmed the presence of DIC. A prolonged R-time indicated a decrease in coagulation factors. A markedly reduced MA indicated reduced platelet activity. The concurrent blood tests revealed a PT of 24, aPTT of 42.7 and fibrinogen < 0.6 g/L. Renal function was impaired, with creatinine 182 μmol/L.
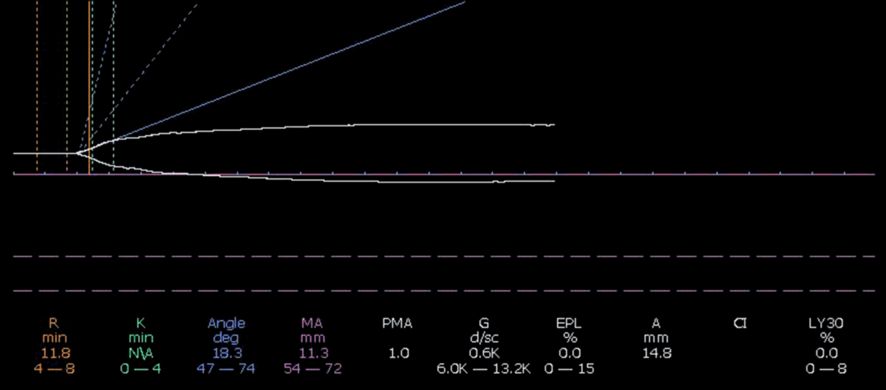
TEG at presentation.
Four units of red cell concentrate, four units of FFP, three units of cryoprecipitate and two adult doses of platelets were infused. A repeat TEG (Figure 21.3) showed a marked improvement in the haemostatic profile. Blood tests confirmed the improvement with a PT of 14, aPTT of 35 and fibrinogen of 35 g/L.
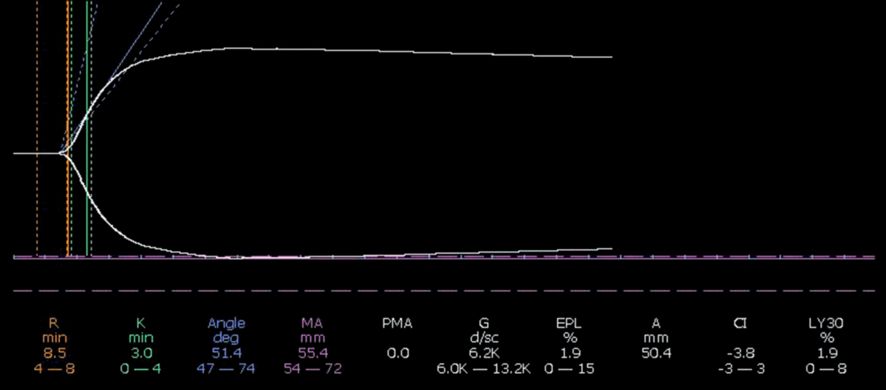
TEG after correction with blood products.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






