1. Relevant American Society of Anesthesiologists standards
a. Basic Standards for Preanesthesia Care
Approved 1987, last amended 2010.11
In summary, these standards apply to all patients who receive anesthesia care. These standards require the following: review of the patient record, patient interview and focused exam, preoperative testing and consultation when needed, and a check of the surgical consent. Under exceptional circumstances, these standards may be modified. In that case, the circumstances requiring the modification should be documented in the chart.
b. Standards for Basic Anesthetic Monitoring
Approved 1986, last amended 2011.11
In summary, the basics include the monitoring of oxygenation, ventilation, circulation, and temperature, and require the presence of qualified anesthesia personnel to perform these tasks. These standards apply to all anesthesia care, although, in emergency circumstances, appropriate life support measures take precedence. These standards are not intended for application in the care of the obstetric patient in labor. However, they do apply for procedures occurring in labor and delivery operating rooms.
c. Standards for Postanesthesia Care
Approved 2004, last amended 2009.11
In summary, these standards apply to postanesthesia care in all locations. All patients who have received general anesthesia (GA), regional anesthesia, or monitored anesthesia care for operative procedures shall receive appropriate postanesthetic management. Furthermore, a member of the anesthesia team will manage patient care during transport to the postanesthesia care unit (PACU) and, after arrival, reevaluate the patient and give a verbal report to the PACU nurse.
2. Relevant American Society of Anesthesiologists Practice Guidelines
a. Practice Guidelines for Obstetric Anesthesia
Approved 1999, last amended 2006, revisions in progress, 2014.12
These guidelines have been systematically developed to assist the practitioner and patient in making decisions about anesthetic care. Their purpose is to enhance the quality of anesthetic care for obstetric patients, improve patient safety by reducing the incidence of anesthesia-related complications, and increase patient satisfaction. The guidelines focus on the anesthetic management of pregnant patients during labor, nonoperative delivery, operative delivery, and selected aspects of postpartum care and analgesia (i.e., neuraxial opioids for postpartum analgesia after neuraxial anesthesia for CD). The intended patient population includes, but is not limited to, intrapartum and postpartum patients with uncomplicated pregnancies or with common obstetric problems. The guidelines do not apply to patients undergoing surgery during pregnancy, gynecologic patients, or parturients with chronic medical disease (e.g., severe cardiac, renal, or neurologic disease). These guidelines do not address postpartum analgesia for vaginal delivery, analgesia after tubal ligation, or postoperative analgesia after GA for CD.
The current recommendations include:
(1) Perianesthetic evaluation
(a) “Examination of the airway, heart and lungs, consistent with the ASA Practice Advisory on Preanesthesia Evaluation.”
(b) “Recognition of significant anesthetic or obstetric risk factors should encourage consultation between the obstetrician and the anesthesiologist. A communication system should be in place to encourage early and ongoing contact between obstetric providers, anesthesiologists, and other members of the multidisciplinary team.”
(c) “The fetal heart rate (FHR) should be monitored by a qualified individual before and after administration of neuraxial analgesia for labor. Continuous electronic recording of the FHR may not be necessary in every clinical setting and may not be possible during initiation of neuraxial analgesia.”
(d) “A routine platelet count is unnecessary in the healthy parturient before neuraxial anesthesia.”
(e) “A type and screen or cross-match should be ordered on an individual basis, depending on risk factors and ‘local institutional policies.’”
(2) Aspiration prophylaxis
(a) “The oral intake of modest amounts of clear liquids may be allowed for uncomplicated laboring patients. The uncomplicated patient undergoing delivery may have modest amounts of clear liquids up to 2 h before the induction of anesthesia. However, patients with additional risk factors for aspiration (e.g., morbid obesity, diabetes) or patients at increased risk for CD (e.g., nonreassuring FHR) may have further restrictions of oral intake, determined on a case-by-case basis.”
(b) “Solid foods should be avoided in laboring patients.” Recommendations are consistent with the ASA Practice Guidelines for Preoperative Fasting stating, “the patient undergoing elective surgery (e.g., scheduled CD or PPTL) should undergo a fasting period for solids of 6–8 h depending on the type of food ingested (e.g., fat content).”12
(c) “Before surgical procedures, practitioners should consider the timely administration of nonparticulate antacids, H2-receptor antagonists, and/or metoclopramide for aspiration prophylaxis.”
(3) Anesthetic care for labor and vaginal delivery
(a) “Patients in early labor (i.e., < 5 cm dilation) should be given the option of neuraxial analgesia when this service is available. Neuraxial analgesia should not be withheld on the basis of achieving an arbitrary cervical dilation, and should be offered on an individualized basis. Patients should be reassured that the use of neuraxial analgesia does not increase the incidence of CD.”
(b) “Patient-controlled epidural analgesia (PCEA) may be used to provide an effective and flexible approach for the maintenance of labor analgesia.” The Task Force notes that the use of “PCEA may be preferable to continuous infusion techniques for providing fewer anesthetic interventions, reduced dosages of local anesthetics, and less motor blockade than fixed-rate continuous epidural infusions. PCEA may be used with or without a background infusion.”
(c) “Combined spinal-epidural techniques may be used to provide effective and rapid onset of analgesia for labor.”
(4) Anesthetic choices for cesarean delivery
(a) “Equipment, facilities, and support personnel available in the labor and delivery operating suite should be comparable to those available in the main operating suite.”
(b) “The decision to use a particular anesthetic technique for CD should be individualized, based on several factors. These include anesthetic, obstetric, or fetal risk factors (e.g., elective vs. emergency), the preferences of the patient, and the judgment of the anesthesiologist.”
(c) “Neuraxial techniques are preferred to GA for most CD. An indwelling epidural catheter may provide equivalent onset of anesthesia compared with initiation of spinal anesthesia for urgent CD. If spinal anesthesia is chosen, pencil-point spinal needles should be used instead of cutting-bevel spinal needles.”
(d) “However, GA may be the most appropriate choice in some circumstances (e.g., profound fetal bradycardia, ruptured uterus, severe hemorrhage, severe placental abruption). Uterine displacement (usually left displacement) should be maintained until delivery regardless of the anesthetic technique used.”
(e) “Intravenous [IV] fluid preloading may be used to reduce the frequency of maternal hypotension after spinal anesthesia for CD. Although fluid preloading reduces the frequency of maternal hypotension, initiation of spinal anesthesia should not be delayed in order to administer a fixed volume of IV fluid.”
(f) “IV ephedrine and phenylephrine are both acceptable drugs for treating hypotension during neuraxial anesthesia. In the absence of maternal bradycardia, phenylephrine may be preferable because of improved fetal acid–base status in uncomplicated pregnancies.”
(g) “Pencil-point spinal needles should be used instead of cutting-bevel spinal needles to minimize the risk of postdural puncture headache.”
(5) Postpartum tubal ligation
(a) “For postpartum tubal ligation [PPTL], the patient should have no oral intake of solid foods within 6–8 h of the surgery, depending on the type of food ingested (e.g., fat content). Aspiration prophylaxis should be considered.”
(b) “Both the timing of the procedure and the decision to use a particular anesthetic technique (i.e., neuraxial vs. general) should be individualized, based on anesthetic risk factors, obstetric risk factors (e.g., blood loss), and patient preferences. However, neuraxial techniques are preferred to GA for most PPTLs.”
(c) “The anesthesiologist should be aware that gastric emptying will be delayed in patients who have received opioids during labor, and that an epidural catheter placed for labor may be more likely to fail with longer postdelivery time intervals.”
(d) “If a PPTL is to be performed before the patient is discharged from the hospital, the procedure should not be attempted at a time when it might compromise other aspects of patient care on the labor and delivery unit.”
(6) Management of obstetric and anesthetic emergencies
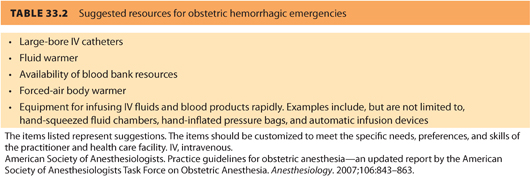
(a) “Institutions providing obstetric care should have resources available to manage hemorrhagic emergencies [see Table 33.2]. In an emergency, the use of type-specific or O negative blood is acceptable.”
(b) “In cases of intractable hemorrhage when banked blood is not available or the patient refuses banked blood, intraoperative cell-salvage should be considered if available.”
(c) “Labor and delivery units should have personnel and equipment readily available to manage airway emergencies, to include a pulse oximeter and qualitative carbon dioxide detector, consistent with the ASA Practice Guidelines for Management of the Difficult Airway. Basic airway management equipment should be immediately available during the provision of neuraxial analgesia [see Table 33.3]. In addition, portable equipment for difficult airway management should be readily available in the operative area of labor and delivery units [see Table 33.4]. The anesthesiologist should have a preformulated strategy for intubation of the difficult airway. When tracheal intubation has failed, ventilation with mask and cricoid pressure or with a laryngeal mask airway [LMA] or supraglottic airway device (e.g., Combitube, Intubating LMA [Fastrach]) should be considered for maintaining an airway and ventilating the lungs. If it is not possible to ventilate or awaken the patient, an airway should be created surgically.”


(d) “Basic and advanced life-support equipment should be immediately available in the operative area of labor and delivery units. If cardiac arrest occurs during labor and delivery, standard resuscitative measures should be initiated. In addition, uterine displacement (usually left displacement) should be maintained. If maternal circulation is not restored within 4 min, CD should be performed by the obstetric team.”
b. Practice Guidelines for Preoperative Fasting
Approved in 1999, last amended in 2010.12
The ASA Practice Guidelines for Obstetric Anesthesia reference the older (1999) version of this document when addressing the topic of fasting in the obstetric patient (see preceding text); however, there have been no changes in the recommendations between the original and revised version.
c. Practice Guidelines for Postanesthetic Care
Approved 2001, last amended 2012.12
(1) These guidelines update the literature, but provide no change to the 2001 recommendations for care of all patients following anesthesia care.
(2) Patient assessment and monitoring; prophylaxis and treatment of nausea and vomiting; treatment for emergence and recovery; antagonism of the effects of sedatives, analgesics, and neuromuscular blocking agents; and the protocol for discharge are addressed.
d. Practice Guidelines for the Prevention, Detection, and Management of Respiratory Depression Associated with Neuraxial Opioid Administration
Approved 2008.12
Respiratory depression following neuraxial opioid administration is an important cause of perioperative morbidity and mortality. These guidelines apply to management of patients on labor and delivery. These guidelines incorporate (but are not limited to) the following recommendations.
(1) Prevention
(a) The anesthesiologist should “conduct a focused history and physical examination before administering neuraxial opioids.” Particular attention should be directed “toward signs, symptoms, or a history of sleep apnea, co-existing diseases or conditions (e.g., diabetes, obesity), current medications (including preoperative opioids), and adverse effects following opioid administration.”
(b) “The lowest effective dose of neuraxial opioids should be administered to minimize the risk of respiratory depression.”
(c) “Parenteral opioids or hypnotics should be cautiously administered in the presence of neuraxial opioids.”
(d) “The concomitant administration of neuraxial opioids and parenteral opioids, sedatives, hypnotics, or magnesium requires increased monitoring (e.g., intensity, duration, or additional methods of monitoring).”
(2) Detection
(a) “All patients receiving neuraxial opioids should be monitored for adequacy of ventilation (e.g., respiratory rate, depth of respiration [assessed without disturbing a sleeping patient]), oxygenation (e.g., pulse oximetry when appropriate), and level of consciousness.”
(i) “For single-injection neuraxial lipophilic opioids (e.g., fentanyl), monitoring should be performed for a minimum of 2 h after administration. Continual monitoring (i.e., repeated regularly and frequently in steady rapid succession) monitoring should be performed for the first 20 min after administration, followed by monitoring at least once per hour until 2 h has passed. After 2 h, frequency of monitoring should be dictated by the patient’s overall clinical condition and concurrent medications.”
(ii) “For continuous infusion or PCEA with neuraxial lipophilic opioids, monitoring should be performed during the entire time the infusion is in use. Monitoring should be continual for the first 20 min after initiation, followed by monitoring at least once per hour until 12 h has passed. From 12 to 24 h, monitoring should be performed at least once every 2 h. After 24 h, monitoring should be performed at least once every 4 h. After discontinuation of continuous infusion or PCEA with neuraxial lipophilic opioids, frequency of monitoring should be dictated by the patient’s overall clinical condition and concurrent medications.”
(iii) “For single-injection neuraxial hydrophilic opioids (e.g., morphine, not including sustained-or extended-release epidural morphine), monitoring should be performed for a minimum of 24 h after administration. Monitoring should be performed at least once per hour for the first 12 h after administration, followed by monitoring at least once every 2 h for the next 12 h (i.e., from 12 to 24 h). After 24 h, frequency of monitoring should be dictated by the patient’s overall clinical condition and concurrent medications.”
(iv) “For continuous infusion or PCEA with neuraxial hydrophilic opioids, monitoring should be performed during the entire time the infusion is in use. Monitoring at least once every hour should be performed for the first 12 h after initiation, followed by monitoring at least once every 2 h for the next 12 h. After 24 h, monitoring should be performed at least once every 4 h. After discontinuation of continuous infusion or PCEA, frequency of monitoring should be dictated by the patient’s overall clinical condition and concurrent medications.”
(v) “For sustained-or extended-release epidural morphine, monitoring at least once every hour should be performed during the first 12 h after administration, and at least once every 2 h for the next 12 h (i.e., from 12 to 24 h). After 24 h, monitoring should be performed at least once every 4 h for a minimum of 48 h.”
(vi) “Increased monitoring (e.g., intensity, duration, or additional methods of monitoring) may be warranted in patients at increased risk of respiratory depression (e.g., unstable medical condition, obesity, obstructive sleep apnea, concomitant administration of opioid analgesics or hypnotics by other routes, extremes of age).”
(3) Management/treatment
(a) “For patients receiving neuraxial opioids, supplemental oxygen should be available.”
(b) “Supplemental oxygen should be administered to patients with altered level of consciousness, respiratory depression, or hypoxemia and continued until the patient is alert and no respiratory depression or hypoxemia is present.”
(c) “Routine use of supplemental oxygen may increase the duration of apneic episodes and may hinder detection of atelectasis, transient apnea, and hypoventilation.”
(d) Reversal agents should be available. Noninvasive positive-pressure ventilation is an option to improve ventilation status.
e. Practice Guidelines for Management of the Difficult Airway
Approved 2002, last amended 2012.12
This updated document presents updated evidence and literature, but the recommendations remain unchanged from the 2002 document.
(1) The recommendations state: “the preoperative airway evaluation should include an airway history and physical exam and appropriate additional evaluation when appropriate.”
(2) “Basic preparation for a potential difficult airway case includes informing the patient, presence of a readily available portable cart containing necessary equipment, and the availability of additional staff for assistance.”
(3) “Facemask oxygenation is imperative prior to airway management and supplemental oxygen is needed throughout the intubation process.”
(4) Strategies for intubation and extubation of the difficult airway are given as well as suggestions for follow-up with the patient.
3. Relevant American Society of Anesthesiologists Practice Advisories
a. Practice Advisory for Preanesthesia Evaluation
Approved 2001, last amended 2010.12
This Advisory is an update of the original document, providing new scientific information, but no changes in the recommendations. It discusses the timing of the preanesthetic evaluation and content of that exam. Although routine preop tests are not necessary, selective tests may help in patient assessment and management. Specific tests and timing of tests should be individualized.
(1) On preanesthesia pregnancy testing, it states, “Patients may present for anesthesia with early undetected pregnancy.” The Task Force believes that the literature is inadequate to inform patients or physicians on whether anesthesia causes harmful effects on early pregnancy.
(2) “Pregnancy testing may be offered to female patients of childbearing age and for whom the result would alter the patient’s management.”
b. Practice Advisory for Intraoperative Awareness and Brain Function Monitoring
Approved 2006.12
This document defines consciousness, GA, depth of anesthesia or depth of hypnosis, recall, amnesia, and intraoperative awareness.
(1) Its stated purpose is to identify risk factors that may be associated with intraoperative awareness. The risk factors pertinent to obstetrics include CD, emergency surgery, reduced anesthetic doses in the presence of paralysis, planned use of muscle relaxants during the maintenance phase of GA, total IV anesthesia, and the planned use of nitrous oxide-opioid anesthesia.
(2) To reduce the frequency of unintended intraoperative awareness, the advisory suggests avoiding equipment malfunction or misuse by using a checklist.
(3) The document states, “Intraoperative monitoring of depth of anesthesia, for the purpose of minimizing the occurrence of awareness, should rely on multiple modalities, including clinical techniques (e.g., checking for clinical signs such as purposeful or reflex movement) and conventional monitoring systems (e.g., electrocardiogram, blood pressure, HR, end-tidal anesthetic analyzer, capnography). The use of neuromuscular blocking drugs may mask purposeful or reflex movements and adds additional importance to the use of monitoring methods that assure the adequate delivery of anesthesia.”
(4) “It is the consensus of the Task Force that the decision to use a brain function monitor should be made on a case-by-case basis by the individual practitioner for selected patients (e.g., light anesthesia).”
c. Practice Advisory for the Prevention, Diagnosis, and Management of Infectious Complications Associated with Neuraxial Techniques
Approved 2009.12
This document identifies patients who are at increased risk for infectious complications with neuraxial techniques, looks at ways to reduce their risk, and how to intervene should infectious complications arise.
(1) To reduce the risks associated with neuraxial techniques, consider alternative options for patients at high risk, administer preprocedure antibiotic therapy for patients with known or suspected bacteremia, consider the evolving medical status of the patient, and avoid a lumbar puncture in a patient with a known epidural abscess.
(2) Use aseptic techniques when preparing equipment (e.g., ultrasound) and performing the procedure. Aseptic technique includes removing jewelry (e.g., rings and watches), hand washing, wearing sterile gloves, wearing a cap, wearing a mask that covers the nose and mouth, and consideration for changing the mask between cases.
(3) For skin preparation, use individual packets of antiseptics, use chlorhexidine (preferably with alcohol), and allow adequate drying time before the procedure. Use sterile drapes and sterile occlusive dressings at the catheter insertion site. Consider using bacterial filters for extended continuous epidural infusions, limit the disconnection and reconnection of neuraxial delivery systems, and consider removing unwitnessed accidentally disconnected catheters. Remove catheters as soon as no longer clinically necessary.
(4) To diagnose infection, the ASA advisory states, “Daily evaluation of patients with indwelling catheters for early signs and symptoms (e.g., fever, backache, headache, erythema, and tenderness at the insertion site) of infectious complications should be performed throughout their stay in the facility. To minimize the impact of an infectious complication, promptly attend to signs or symptoms.”
(5) If an infection is suspected, (a) remove an in situ catheter and consider culturing the catheter tip, (b) order appropriate blood tests, (c) obtain appropriate cultures, and (d) if an abscess is suspected or neurologic dysfunction is present, imaging studies should be performed, and consultation with other appropriate specialties should be promptly obtained.
(6) Treatment includes appropriate antibiotic therapy, appropriate consultation, and possible laminectomy.
4. Relevant American Society of Anesthesiologist Statements, Positions, and Protocols
a. Statement on Nonoperating Room Anesthetizing Locations
Approved 1994, last amended 2013.11
The updated title now calls this a statement (not a guideline, which is appropriate because it does not meet the definition of an evidence-based document).
(1) In summary, these guidelines apply to all anesthesia care involving anesthesiology personnel for procedures in locations outside an operating room, such as in birthing rooms in labor and delivery.
(2) These are minimal guidelines for equipment and staffing for nonoperating room settings, except where they are not applicable to an individual patient or care setting.
b. Optimal Goals for Anesthesia Care in Obstetrics
Approved 2007, amended 2010, ASA/ACOG review in progress in 2014.11
This is a joint statement from ASA and ACOG that discusses the optimal goals for availability of equipment, qualified physicians, other personnel (e.g., obstetric, anesthesia, and neonatal resuscitation providers) for elective and emergent obstetric cases involving GA and neuraxial anesthesia, as well as the timing of these cases. It emphasizes the importance but is not limited to:
(1) “Availability of anesthesia and surgical personnel to permit the start of a cesarean delivery within 30 minutes of the decision to perform the procedure.”
(2) “Because the risks associated with trial of labor after cesarean delivery (TOLAC) and uterine rupture may be unpredictable, the immediate availability of appropriate facilities and personnel (including obstetric anesthesia, nursing personnel, and a physician capable of monitoring labor and performing CD, including an emergency CD) is optimal.” When resources are not available, the patient should be informed of the potential increased risk and management options. “The definition of immediately available personnel and facilities remains a local decision based on each institution’s available resources and geographic location.”
(3) “Persons administering or supervising obstetric anesthesia should be qualified to manage the infrequent but occasionally life-threatening complications of major neuraxial anesthesia such as respiratory and cardiovascular failure, toxic local anesthetic convulsions, or vomiting and aspiration. Mastering and retaining the skills and knowledge necessary to manage these complications require adequate training and frequent application.”
(4) “A qualified physician with obstetric privileges to perform operative vaginal or cesarean delivery should be readily available during administration of anesthesia. Readily available should be defined by each institution within the context of its resources and geographic location.”
(5) “Availability of equipment, facilities, and support personnel equal to that provided in the surgical suite.”
(6) “Personnel other than the surgical team should be immediately available to assume responsibility for resuscitation of the depressed newborn. The surgeon and anesthesiologist are responsible for the mother and may not be able to leave her care for the newborn even when a regional anesthetic is functioning adequately.”
(7) “In larger maternity units and those functioning as high-risk centers, 24-hour in-house anesthesia, obstetric and neonatal specialists are usually necessary.”
c. Statement on Pain Relief during Labor
Approved 1999, last amended 2010, ASA/ACOG joint review in progress 2014.11
(1) This joint ASA/ACOG statement says that “labor results in severe pain for many women. There is no circumstance where it is considered acceptable for an individual to experience untreated severe pain, amenable to safe intervention, while under a physician’s care. In the absence of a medical contraindication, maternal request is a sufficient medical indication for pain relief during labor.”
(2) “Pain management should be provided whenever medically indicated.” Women should not be denied anesthesia services based on “their insurance or inadequate nursing participation.”
d. Guidelines for Neuraxial Anesthesia in Obstetrics (previously titled: Guidelines for Regional Anesthesia in Obstetrics)
Approved 1988, last amended 2013.11
Neuraxial anesthesia is an updated term for regional anesthesia, thus the name change. This document (and its recommendations) is called “Guidelines for Neuraxial Anesthesia in Obstetrics,” but it functions like an ASA statement. The document also references four other ASA documents: The Standards for Basic Anesthetic Monitoring, Standards for Postanesthesia Care, the Guidelines for Perinatal Care, and an ASA House of Delegates opinion document on the Anesthesia Care Team. These “guidelines” are nevertheless important because they apply to the use of neuraxial anesthesia or analgesia for the parturient during labor and delivery.
(1) In summary, “They are intended to encourage quality patient care, but cannot guarantee any specific patient outcome. Because the availability of anesthesia resources may vary, members are responsible for interpreting and establishing the guidelines for their own institutions and practices.”
(2) There are 10 “guidelines” that review location requirements, physician privileging, monitoring, and IV requirements. Also, physicians with obstetric privileges “should remain readily available” who are capable of performing an emergent operative delivery. Other personnel for emergencies and resuscitation equipment should also be available.
(3) It states, “Qualified personnel, other than the anesthesiologist attending the mother, should be immediately available to assume responsibility for resuscitation of the newborn.”
e. Statement on Regional Anesthesia
Approved 1983, last amended 2012.11
This document states in part that “regional anesthesia involves diagnostic assessment, the consideration of indications and contraindications, the prescription of drugs, and the institution of corrective measures and treatment in response to complications.” Medical and technical expertise involved in performing regional anesthesia is part of the practice of medicine and are best performed by a skilled anesthesiologist.
f. Definition of “Immediately Available” when Medically Directing
Approved 2012.11
(1) “A medically directing anesthesiologist is immediately available if s/he is in physical proximity that allows the anesthesiologist to return to re-establish direct contact with the patient to meet medical needs and address any urgent or emergent clinical problems. These responsibilities may also be met through coordination among anesthesiologists of the same group or department.”
(2) “Differences in the design and size of various facilities and demands of the particular surgical procedures make it impossible to define a specific time or distance for physical proximity.”
g. Statement on Nonobstetric Surgery during Pregnancy
Approved by ASA-2009, Review by ASA/ACOG in progress in 2014.11
This is a joint ASA/ACOG statement.
(1) “Due to the difficulty of conducting large-scale randomized clinical trial in this population, there are no data to allow for specific recommendations.”
(2) In general, “no currently used anesthetic agents have been shown to have any teratogenic effects in humans when using standard concentrations at any gestational age.”
(3) Fetal heart rate monitoring may assist in maternal positioning and cardiorespiratory management, and may influence a decision to deliver the fetus.
(4) Consensus recommendations state that pregnant woman, regardless of gestational age, should never be denied surgery. Delay elective surgical cases until after delivery. If possible, delay urgent cases until the second trimester.
(5) General guidelines for fetal monitoring for previable and viable fetuses are given, although the decision to use fetal monitoring should be individualized.
h. Statement on the Role of Registered Nurses in the Management of Continuous Regional Analgesia
Approved 2002, last amended 2013.11
(1) This document states that experienced registered nurses, under medical supervision, can participate in managing patients with regional anesthesia catheter techniques in all settings, including labor and delivery.
(2) This includes beginning, adjusting, and discontinuing catheter infusions, administering physician prescribed analgesic boluses through the catheter, using aseptic technique while replacing empty medication syringes and bags with new prefilled syringes and bags, monitoring the patient for analgesic efficacy, side effects and treating related side effects, monitoring the catheter insertion site, and removing the catheter.
5. Relevant American Society of Anesthesiologist Committee Opinions
Proposed by the Agency for Healthcare Research and Quality (AHRQ).
a. Comparative Effectiveness of Interventions to Decrease Cesarean Births11
(1) The House of Delegates requested that the ASA Committee on Obstetric Anesthesia explore the interventions used for decreasing the CD rate.
(2) Neuraxial anesthesia does not increase the risk of CD.
(3) Dysfunctional labor and macrosomia are more likely risk factors for operative delivery. These factors also increase labor pain, patient request for analgesia, and epidural use.
(4) Epidural analgesia does not mask the symptoms of uterine rupture during a TOLAC. Adequate pain relief from an epidural may encourage patients to choose and then complete a TOLAC, therefore helping decrease the repeat CD rate.
b. Nitrous oxide for labor analgesia11
(1) The use of nitrous oxide for labor analgesia is common in other countries, but rare in the United States.
(2) Further studies are needed to study the efficacy of nitrous oxide for labor analgesia and the reasons for maternal satisfaction with use. Reductions in pain scores appear to be similar to those seen with systemic opioids.
(3) Adverse effects include mild maternal hypoxemia, maternal drowsiness, possible neurotoxic effects, and environmental pollution.
(4) Nitrous oxide has no effect on uterine activity.
(5) If nitrous oxide analgesia is planned, then patient consent and use of appropriate protocols is warranted.
IX. American College of Obstetricians and Gynecologists
Official website: www.acog.org
A. As ACOG documents are revised and replaced, their identifying numbers and web addresses change. Some documents are deleted, such as the Practice Bulletin No. 49, 2003 on Dystocia and Augmentation of Labor and the Committee Opinion No. 276, 2002, “Safety of Enoxaparin (Lovenox) in Pregnancy.” The best way to find up-to-date ACOG documents is through the lists of Practice Bulletins and Committee Opinions on the official website. This also gives access to the latest documents from this organization. Members have free online access to all ACOG documents via the ACOG official website. Categories for the documents are listed on the left side of the home page under the heading “For Physicians.”
B. Nonmembers have free online access only to the Committee Opinions and Patient Safety checklists in that location.
Nonmembers can purchase ACOG Practice Bulletins (labeled Compendium of Selected Publications) in hard copy or CD or ROM9, and the Guidelines for Perinatal Care13 in hard copy or e-book via the ACOG Bookstore (see ACOG home page store site on left side of the home page).
Specific ACOG documents are listed by the approval year or the year of last revision (not reaffirmation) based on the more recent document.
C. The ACOG Committee on Obstetric Practice is responsible for obstetric-related ACOG Committee Opinions, Practice Bulletins, and the Guidelines for Perinatal Care.
1. This committee is made up of obstetricians and includes an obstetric anesthesiologist whose input is solicited in those areas that impact obstetric anesthesia. This liaison anesthesiologist is appointed by the ASA and serves as Chairman of the ASA Committee on Obstetric Anesthesia.
2. The relevant ACOG documents include Practice Bulletins, Committee Opinions, and portions of the Guidelines for Perinatal Care that concern the practice of obstetric anesthesia (see Table 33.5). Revised documents are altered to fit updates. Reaffirmed documents are unchanged.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







