Fig. 65.1
Intra-operative microscopic image showing posterior inferior cerebellar artery (PICA) inferior to glossopharyngeal nerve (CN IX) and deep to vagus nerve (CN X)
Tumors
The first description of glossopharyngeal neuralgia by Weisenberg was caused by a cerebellopontine angle tumor [2]. Other neoplastic causes include laryngeal and nasopharyngeal carcinomas, tongue and oropharyngeal cancers, and skull base tumors that can compress the jugular foramen and foramen ovale [1].
Infectious and Inflammatory Processes
Parapharyngeal abscesses can compress the distal glossopharyngeal nerve. Causative inflammatory processes include multiple sclerosis, Paget’s disease, and Sjogren’s syndrome [1].
Anatomic Variants
Occipital-cervical developmental malformations and calcified stylohyoid ligaments can cause compression upon the glossopharyngeal nerve. Calcified stylohyoid ligaments, as well as elongated styloid processes, can cause glossopharyngeal compression, known as Eagle syndrome.
Diagnosis
No specific test can establish a diagnosis of glossopharyngeal neuralgia. This condition has been mistakenly diagnosed as trigeminal neuralgia or geniculate neuralgia [1]. One difference between the two conditions includes the side of the face that is affected; glossopharyngeal neuralgia more commonly affects the left side, whereas trigeminal neuralgia more commonly affects the right side [3]. The differential diagnosis also includes superior laryngeal neuralgia, affecting the vagus nerve, and nervus intermedius neuralgia, which affects the facial nerve. Patients may benefit from evaluation by an otolaryngologist to exclude other causes of glossopharyngeal neuralgia.
Topical anesthesia can help the clinician to identify specific trigger zones and can also help to establish a diagnosis of glossopharyngeal neuralgia, if the patient’s pain is relieved after a nerve block [1]. Imaging studies can help to identify anatomic causes of glossopharyngeal neuralgia. For example, CT can identify an elongated styloid process causing Eagle syndrome [1]. MRI can also help to identify blood vessels, tumors, or infectious and inflammatory processes that are causing glossopharyngeal neuralgia.
Treatment
Conservative Management
Non-surgical, conservative measures remain the first-line treatment of glossopharyngeal neuralgia. Pharmacologic agents include carbamazepine, oxcarbazepine, gabapentin, pregabalin, and tricyclic antidepressants. Opioids are not effective in alleviating glossopharyngeal pain.
For the vagoglossopharyngeal variant, atropine is the first-line medication for treatment by preventing cardiac sequelae [12]. In addition, carbamazepine can address both the cardiac and neurologic symptoms.
Extra-oral glossopharyngeal nerve blocks have recently been used to treat glossopharyngeal neuralgia [13]. Non-neurolytic agents include local anesthetics, steroids, and ketamine. Neurolytic agents include phenol, alcohol, and glycerol. Singh et al. concluded that this treatment modality works best when combined with pharmacologic agents [13].
Surgical Management
Singleton and Dandy were the first neurosurgeons to describe intracranial sectioning of the glossopharyngeal nerve [14, 15]. In 1977, Laha and Janetta treated the underlying cause of glossopharyngeal neuralgia by performing microvascular decompressions [16].
Microvascular decompression (MVD) of the glossopharyngeal and vagus nerves remains the surgery of choice in the treatment of glossopharyngeal neuralgia, with the highest success rate of any surgical modality [17] (Fig. 65.2). In a series of 217 patients, Patel et al. [18] reported complete pain relief without the need for medication in 58% of patients after an average period of 4 years [18].
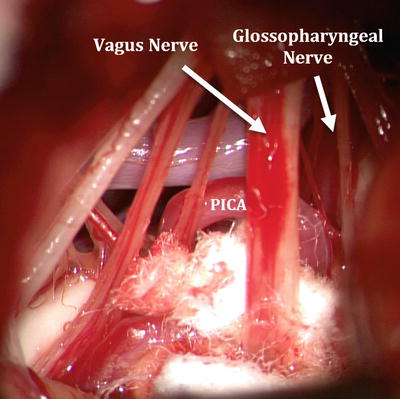
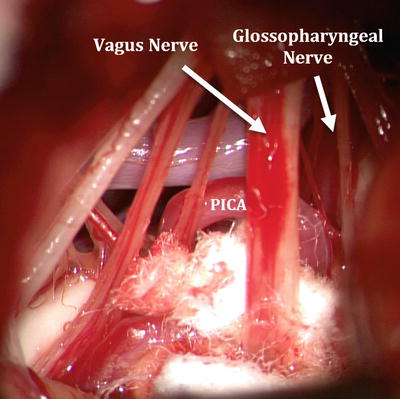
Fig. 65.2
Intra-operative microscopy demonstrating cotton plegets placed between vagus nerve (CN X), PICA, and glossopharyngeal nerve (CN IX)
Eagle syndrome , caused by elongation of the styloid process, is treated by minimally invasive resection of the styloid process [19].
Rhizotomy of the glossopharyngeal nerve can be a safe alternative surgical procedure when microvascular decompression fails [1]. If an offending blood vessel cannot be identified, the surgeon can section the glossopharyngeal and vagus nerves [17, 20]. Potential complications, however, include dysphagia and vocal cord paralysis, which result from damage to the recurrent laryngeal branch of the vagus nerve [21]. Other open surgical procedures include radiofrequency ablation of the glossopharyngeal nerve and balloon compression.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





