Chapter 53 Geriatric Considerations in Emergency Nursing
Older adults, particularly those 75 years and older, use emergency department (ED) services more than any other group. However, many times this vulnerable patient group is treated using guidelines that were tested in the general adult population and this may lead to poor clinical outcomes. The ED is the greatest source of hospital admissions in older adults; according to the National Center for Health Statistics, about 15% of all visits to the ED result in hospital admission.1 Most hospital admissions via the ED result from an inadequate transition linked to either a prior hospitalization or a visit to the ED.1 This chapter provides content to increase awareness about the vulnerability of older adults presenting to the ED and guidelines to improve clinical outcomes.
Age-Related Changes Affecting Vulnerability
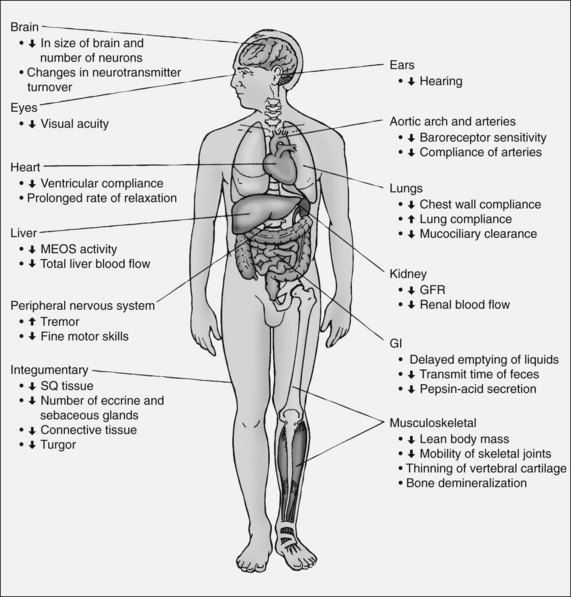
Older patients discharged home from the ED are at significant risk for adverse outcomes such as functional decline, return to the ED, hospitalization, and death.1,2 Age-related physiologic changes affect all organ systems (Fig. 53-1), which potentially has important implications in clinical management of patients in the ED.
Knowledge of these physiologic changes is important in caring for this vulnerable population in the ED3 (Table 53-1).
TABLE 53-1 AGE-RELATED PHYSIOLOGIC CHANGES
| AGE-RELATED CHANGES | CLINICAL CONSIDERATIONS | NURSING INTERVENTIONS |
|---|---|---|
| Cardiovascular system | ||
| Respiratory system | ||
| Renal system | ||
• Certain antibiotics administered in the ED may require renal dosing. Estimate creatinine clearance as a measurement of renal function rather than serum creatinine (normal value does not mean normal renal function because age-related loss of muscle mass affects serum creatinine) • Monitor oxygen saturation, cardiac rhythm, vital signs, and cognition for mental status changes in patients being treated for dehydration or fluid overload • Fluid resuscitation should be slower than for younger patients | ||
| Liver | ||
| Neurologic system | ||
| Musculoskeletal | ||
BP, Blood pressure; CO2, carbon dioxide; ED, emergency department; H2O, water; NH3, ammonia; PaO2, partial pressure of oxygen in arterial blood.
Age-related changes in pharmacokinetics that predispose older adults to adverse drug events are described in Table 53-2.3
TABLE 53-2 AGE-RELATED PHARMACOKINETIC CHANGES
| PHARMACOKINETIC PARAMETER | Age-related change | OTHER FACTORS EXERTING EFFECT |
|---|---|---|
| Absorption—impacts uptake of the drug into tissue | ||
| Distribution—tissue into which the free form of the drug is distributed | ||
| Metabolism—chemical change that renders the drug active or inactive | ||
| Excretion—removal of drug by elimination | ||
| Pharmacodynamics—physiologic response to a drug |
CYP 450, cytochrome P450; GI, Gastrointestinal; H2O, water.
Adapted from Rice, K. L., & Winterbottom, F. (2010). Gerontological alterations and management. In L. D. Urden, K. Stacy, & M. E. Lough (Eds.), Critical care nursing (6th ed.). St. Louis, MO, Mosby.
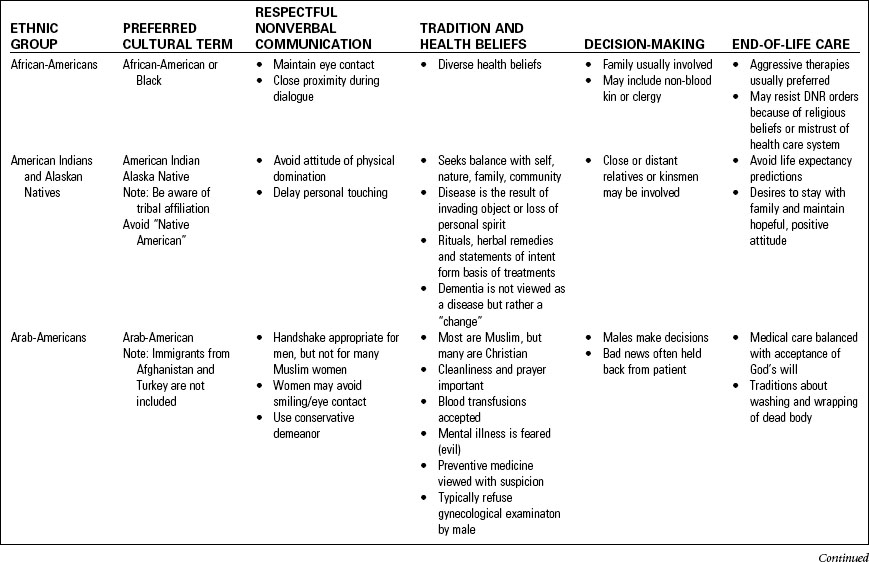
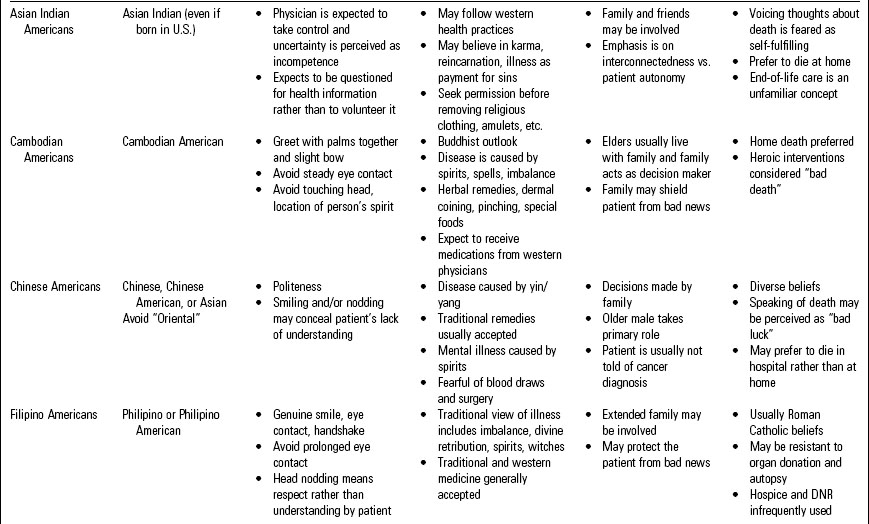
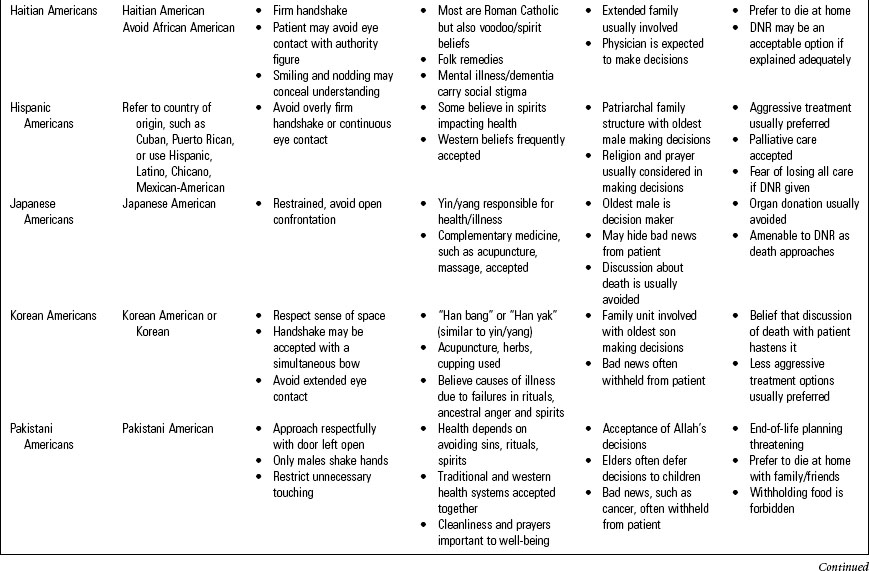
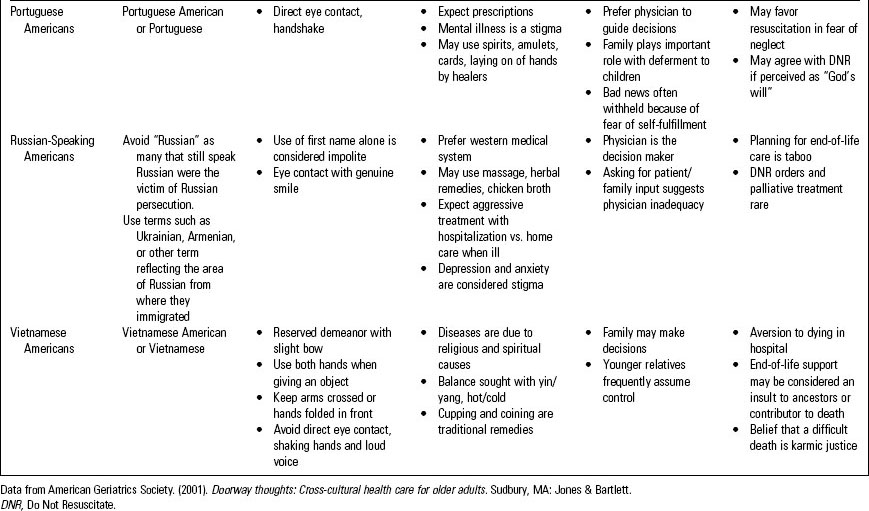
Cross-Cultural Issues in the Elderly
• Elderly persons within every ethnic group can differ greatly.
• Individual preferences may differ from those of persons of shared cultural heritage.
• Differences between ethnic groups differ widely regarding:
Table 53-3 describes cross-cultural issues for 15 ethnic groups4; however, never make assumptions about a patient based on a cultural or ethnic label.
Quality Indicators for Older Adult Emergency Care
In 2009 the Society for Academic Emergency Medicine and the American College of Emergency Physicians identified three conditions as having quality gaps in the care that older adults receive in the ED.5 These conditions include cognitive impairment, pain management, and transitional care.
Table 53-4 describes quality indicators associated with cognitive impairment, pain management, and transitional care.
TABLE 53-4 QUALITY INDICATORS FOR OLDER ADULT EMERGENCY CARE
ED, Emergency department.
a van Zyl, L. Y., & Davidson, P. R. (2003). Delirium in hospital. An underreported event at discharge. Canadian Journal of Psychiatry, 48, 555–560.
Pain Management5
• Pain is a common chief complaint in the ED, with approximately 75% reporting moderate or severe pain.
• Unrelieved acute pain is associated with poor clinical outcomes, including functional decline and an increased risk for developing delirium.
Transitional Care from the Nursing Home5
• More than 2.7 million nursing home residents visit an ED each year. Therefore it is critical that communication channels are open between the ED and nursing home to optimize clinical outcomes.
• Nursing home residents are frequently transported to and from the ED without essential information.
Primary Assessment of the Geriatric Patient
Pain
The International Association for the Study of Pain defines pain as “an unpleasant sensory and emotional experience associated with actual or potential tissue damage.”7 Acute pain has rapid onset with limited duration usually related to apparent pathology. Chronic pain persists for long periods of time and may not be related to disease process. Among older community dwellers, more than 50% report living with pain while at least 85% of nursing home residents experience some form of pain.8 The high prevalence of chronic and acute pain in older adults necessitates adequate pain assessment in the ED. Pain management is considered a quality indicator in managing older adults in the ED (Table 53-4).
Pain Assessment
• Pain is not part of the aging process.
• Involve family members in all aspects of assessment and planning.
• Assessment may be challenging because of multiple concurrent disease processes.
• Patient report is the most reliable evidence.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree