Genitourinary Injuries
Hunter Wessells
I. Introduction
Approximately 10% of trauma patients sustain a genitourinary (GU) injury, with the kidney most commonly involved. The mechanism of injury, physical findings, and urinalysis alert the evaluating physician to the probability of such injuries and guide the initial evaluation.
Hematuria is the hallmark of GU injury and can originate from injury anywhere along the GU tract. However, substantial urologic injury can exist in the absence of blood in the urine.
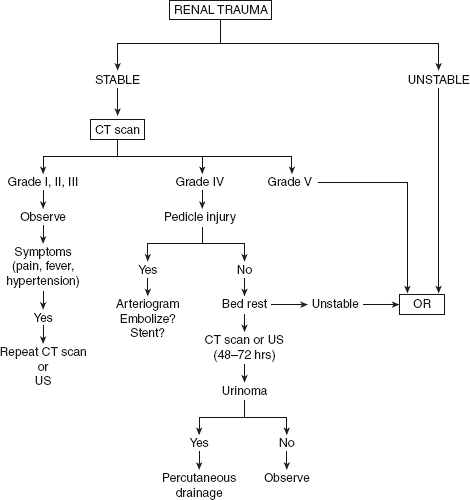
II. Hematuria (Fig. 30-1)
Hematuria is either microscopic (presence of blood noted only with the aid of microscope or urine dipstick) or macroscopic (visible presence of blood).
Any degree of macroscopic hematuria warrants GU evaluation of the upper urinary tract. Degree of macroscopic hematuria does not correlate with degree of injury.
Microscopic hematuria may indicate injury or infection. Testing of the initial aliquot of urine is important as hematuria can clear quickly and be missed.
Guidelines to further evaluate based on microhematuria include:
Proximity of penetrating injuries
Children less than 15 years of age with >30 RBC/high power field
Adults with blunt trauma, microhematuria and
any recorded systolic blood pressure <90 mm Hg
rapid deceleration injuries (e.g., falls from great heights)
selected patients with high risk mechanism (e.g., straddle injury, flank blow) or multiple coexistent injuries
III. Imaging Techniques
Retrograde urethrogram (RUG)
Performed primarily in male patients to evaluate for urethral injury after straddle injury, pelvic fracture, or penetrating mechanism.
To perform, place patient in 30-degree oblique position with upper leg straight and lower leg flexed slightly forward. Insert Foley catheter into the meatus and partially inflate balloon – with 2 to 3 cc of water – to occlude urethra. Stretch penis to straighten anterior urethra. Slowly inject undiluted contrast with plain film or fluoroscopic images at 10 cc intervals.
Evidence of contrast extravasation or occlusion of the urethra implies urethral injury. With these findings, do not place a urinary catheter until urologic consultation is done.
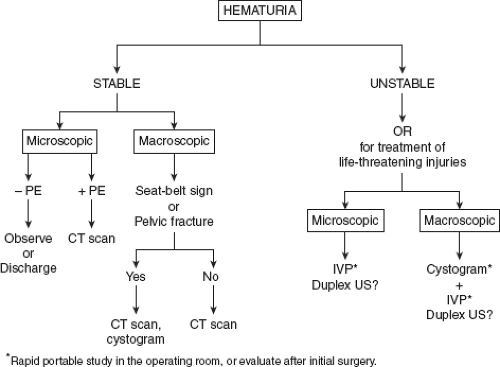
Figure 30-1. Hematuria workup. PE, flank mass, flank pain, lower rib fractures, spine fracture, hypotension (even transient).
Cystography
Plain film cystogram. With urinary catheter in bladder, obtain a scout film. Fill bladder with 350 cc of 30% dilute sterile contrast and obtain a filled bladder AP film. After seeing the view with a distended bladder, drain the bladder entirely and obtain a postdrainage AP film. Many small bladder injuries are appreciated only on postdrainage films. It is important to differentiate intraperitoneal versus extraperitoneal bladder rupture since the management differs.
CT cystography. Preferred method of imaging. The study requires a Foley catheter and a complete fill scan after gravity instillation of 30% contrast at 30 cm H2O height to tolerance in awake patients or to 350 cc in unresponsive patients. Postdrainage scans are not required with CT.
CT scan during the excretion phase following intravenous injection of contrast is not sufficient to exclude bladder injury.
Renal Trauma CT Scan
This is the best method to evaluate and stage injury to the kidneys and ureters.
Examine the early (venous) phase from the diaphragm to the ischial tuberosities to assess vascular and parenchymal integrity of the kidney.
Examine the 10 minute delayed phase to detect urinary contrast extravasation from kidney, renal pelvis, or ureter.
Arteriography
The arteriogram is selectively used in the setting of renal trauma to delineate the vascular integrity of the kidney, particularly in the setting of suspected renal arterial thrombosis or segmental renal arterial injury.
Arteriography followed by stenting or embolization may be therapeutic in cases of thrombosis or bleeding.
One-shot intravenous pyelography (IVP)
Much less commonly used now with wide CT availability, this can be rapidly obtained, especially in patients being taken directly to the OR prior to radiologic investigations.
The purposes of the one-shot IVP are to assess for major renal injury or contrast extravasation and to demonstrate and document contralateral renal function.
It has limited utility during the initial resuscitation and should not delay the transport of a patient to the operating room (OR). Its primary use is as an intraoperative study. Hypotension will limit the effectiveness of the study and is best performed when the patient is normotensive.
To perform, give 2 cc/kg (or 150 cc) of 50% contrast given as an IV bolus followed by a single-shot flat plate film 10 minutes later.
Ultrasound
Ultrasound can rapidly outline the kidney parenchyma and surrounding tissues and provide evidence that an additional study may be necessary.
The imaging study of choice in the evaluation of testicular injuries.
Useful in the evaluation of the transplanted kidney.
IV. Renal Injuries (Fig. 30-2)
Mechanism and diagnosis
In the United States, approximately 80% of renal injuries are the result of blunt trauma and 20% penetrating trauma.
Suspect renal injury in patients with hematuria or a mechanism of injury or physical findings suggestive of renal trauma (Section II).
Significant renal injury can exist in the absence of hematuria—specifically, major injury to the renal pedicle or transection of the ureteropelvic junction (UPJ).
Staging of renal trauma is by CT or intraoperative findings.
Treatment
Nonoperative management is common for hemodynamically stable patients with grade I to IV renal injuries.
Operative exploration is indicated in unstable patients and those with renal hilar or pedicle injuries (selected vascular grades IV and V).
If the patient is explored for other reasons prior to appropriate imaging evaluation, examine the retroperitoneum for evidence of expanding or pulsatile hematomas, the presence of which should prompt renal exploration. A one-shot IVP can be performed prior to renal exploration to document function of the contralateral side should nephrectomy become necessary.
The treatment of nonpulsatile, nonexpanding retroperitoneal hematomas found at the time of exploratory laparotomy is controversial. Generally, watch these if they are the result of blunt trauma. Explore all retroperitoneal hematomas from penetrating trauma, irrespective of the zone.
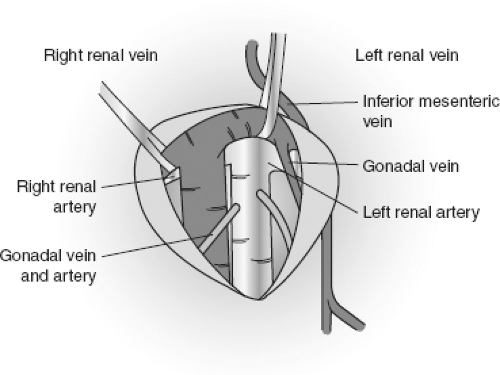
Early vascular control of the injured renal unit maximizes chances of renal unit salvage, best accomplished through a midline transperitoneal approach. Incision of the mesentery just medial and inferior to the inferior mesenteric vein allows exposure of the right- and left-sided renal vessels (Fig. 30-3). Alternatively, reflection of the ipsilateral colon allows exposure of the hilum, but avoids entry into Gerota’s fascia before controlling the renal vessels.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree