CHAPTER 60
Genitofemoral Nerve Block
Perhaps because much of its path is intra-abdominal, the genitofemoral nerve (GFN) nerve is an under-recognized cause of abdominal and pelvic pain.
INDICATIONS
• The diagnosis and treatment of:
![]() Groin pain
Groin pain
![]() Inguinal pain, especially after inguinal hernia repair using mesh and/or staples
Inguinal pain, especially after inguinal hernia repair using mesh and/or staples
![]() Pelvic pain
Pelvic pain
![]() Suprapubic pain (mimicking interstitial cystitis)
Suprapubic pain (mimicking interstitial cystitis)
![]() Vaginal or penile pain
Vaginal or penile pain
• Used with ilioinguinal and iliohypogastric nerve blocks for inguinal herniorrhaphy
• Used with femoral nerve block for saphenous vein stripping
• Used to diagnose genitofemoral neuralgia
RELEVANT ANATOMY
Genitofemoral Nerve
• Branch of the L1 and L2 nerve root
• Pierces the psoas muscle at the level of the third and fourth lumbar vertebra behind the ureter and divides into 2 branches (Figures 60-1 and 60-2)
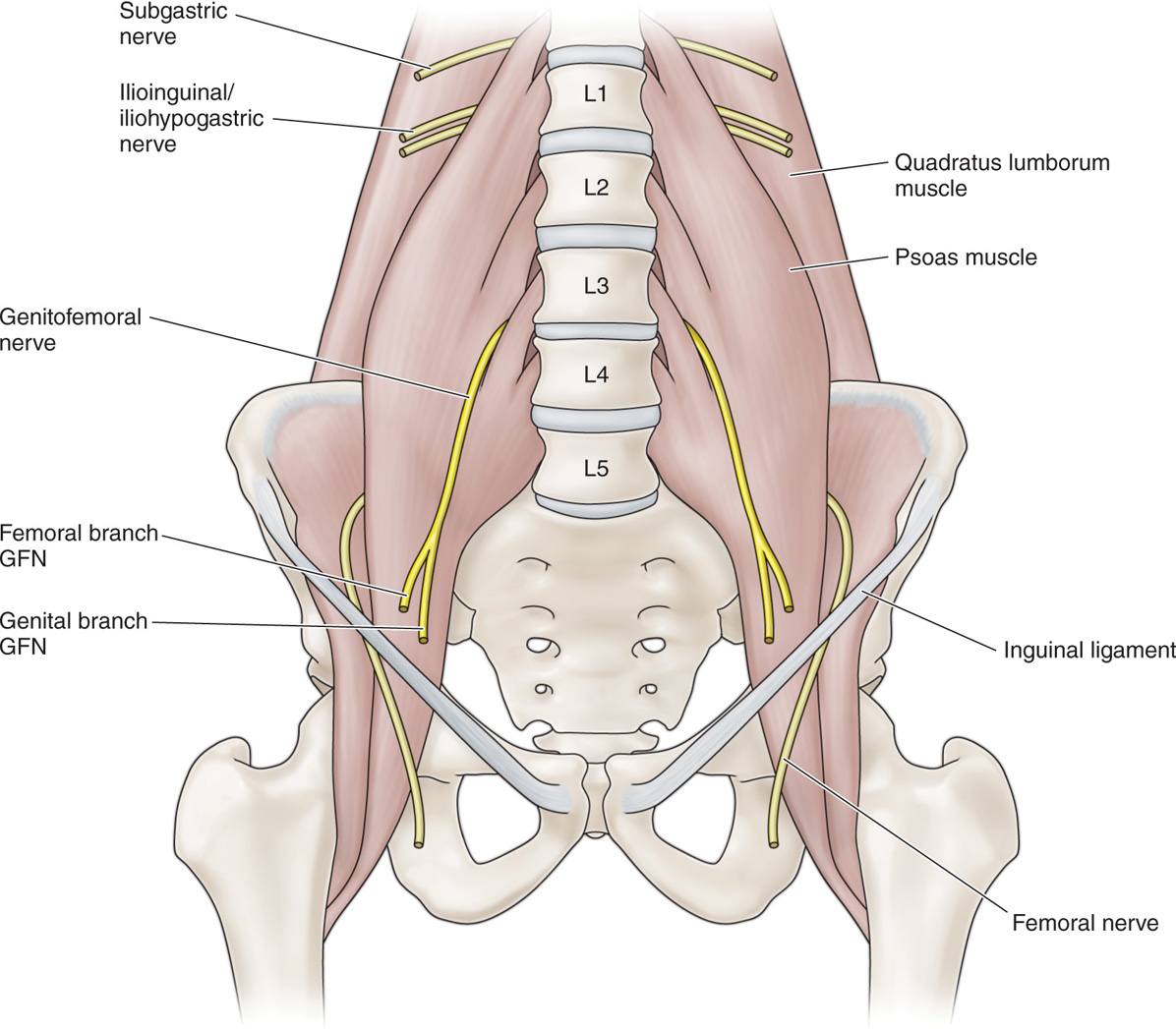
Figure 60-1. Drawing of genitofemoral nerve.
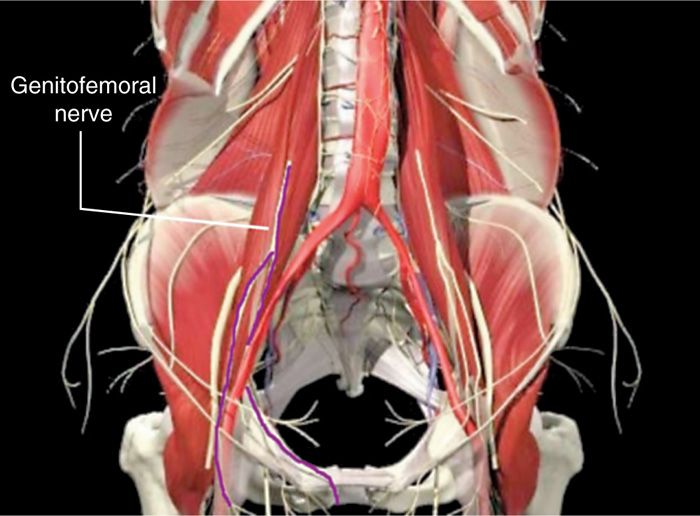
Figure 60-2. Anatomy of genitofemoral nerve.
![]() The genital branch provides the efferent and afferent components of the cremasteric reflex
The genital branch provides the efferent and afferent components of the cremasteric reflex
![]() The femoral branch, which supplies the anterior skin in the femoral triangle
The femoral branch, which supplies the anterior skin in the femoral triangle
![]() Accompanies the external iliac artery in the femoral sheath lateral to the artery
Accompanies the external iliac artery in the femoral sheath lateral to the artery
![]() The genital branch, which travels along the medial pelvic ring, enters the inguinal canal through the deep (ventral) inguinal ring in 97% of patients,1 passing lateral to the pubic tubercle
The genital branch, which travels along the medial pelvic ring, enters the inguinal canal through the deep (ventral) inguinal ring in 97% of patients,1 passing lateral to the pubic tubercle
![]() In males, the genital branch travels through the inguinal canal within the spermatic cord and supplies the cremaster muscle and the scrotal skin.
In males, the genital branch travels through the inguinal canal within the spermatic cord and supplies the cremaster muscle and the scrotal skin.
![]() In females, the genital branch travels with the round ligament and supplies sensation to the mons pubis and labia majora.2
In females, the genital branch travels with the round ligament and supplies sensation to the mons pubis and labia majora.2
BASIC CONCERNS AND CONTRAINDICATIONS
• Large volumes of local anesthetic are often used for blind anesthetic blocks for surgery, but diagnostic injections need to be low volume.
• Contraindications
Absolute
![]() Infection
Infection
![]() Severe anxiety to needle sticks
Severe anxiety to needle sticks
![]() Severe scarring over entire area to be injected
Severe scarring over entire area to be injected
![]() Coagulopathy
Coagulopathy
Relative
![]() Psychogenic pain
Psychogenic pain
![]() Inability to communicate with the patient
Inability to communicate with the patient
![]() Anticoagulant or nonaspirin antiplatelet therapy (for the superficial injections, there is little risk of bleeding, since these are small gauge needles)
Anticoagulant or nonaspirin antiplatelet therapy (for the superficial injections, there is little risk of bleeding, since these are small gauge needles)
Because of its intra-abdominal as well as abdominal wall location, the genitofemoral nerve can be injured by conditions such as:
• Psoas abscess
• Postoperative intra-abdominal scarring
• Any laparoscopic abdominal procedures
• Transpsoas lateral interbody fusion3
• Femoral branch
![]() Trauma to the groin
Trauma to the groin
• Genital branch
![]() Inguinal hernia repair, especially mesh repairs, when the mesh is secured to the Poupart ligament at the symphysis pubis4,5
Inguinal hernia repair, especially mesh repairs, when the mesh is secured to the Poupart ligament at the symphysis pubis4,5
Pain pathology is usually distal; however, occasionally it is necessary to address the nerve proximally at L1.
PREOPERATIVE CONSIDERATIONS
• Informed consent and proper explanation of risks, complications, and benefits must be performed.
• Anticoagulation does not necessarily need to be stopped for the peripheral injections, but anticoagulation needs to be held for the psoas and transforaminal injections.
Fluoroscopic Views
• Although the proximal genitofemoral nerve is not visualized fluoroscopically, the genital branch can be located fluoroscopically at the pubic tubercle (Figures 60-3 and 60-4).

Figure 60-3. Fluoroscopic imaging of GFN location at pubic tubercle.

Figure 60-4. Fluoroscopic imaging of peripheral nerve stimulator directed GFN injection at pubic tubercle. (Used with permission from Andrea Trescot, MD.)
• The psoas muscle shadow can be visualized fluoroscopically (Figures 60-5 and 60-6).
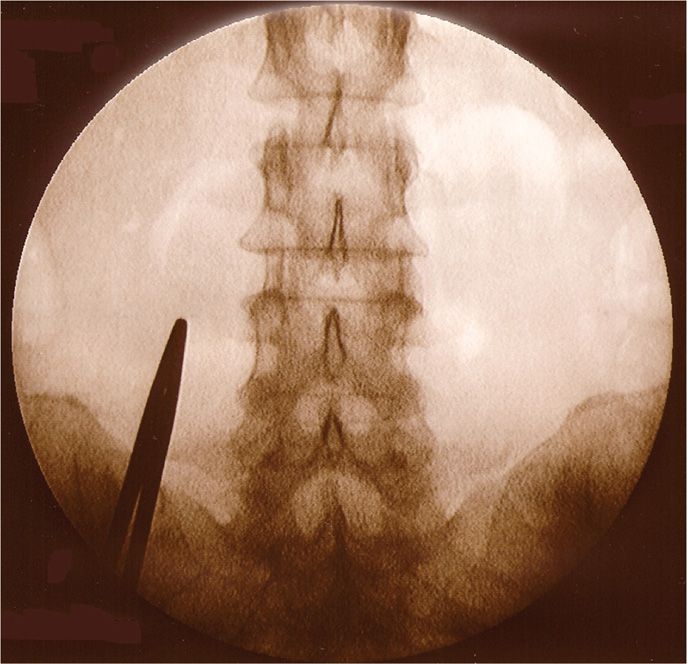
Figure 60-5. Fluoroscopic imaging of psoas shadow. (Used with permission from Andrea Trescot, MD.)
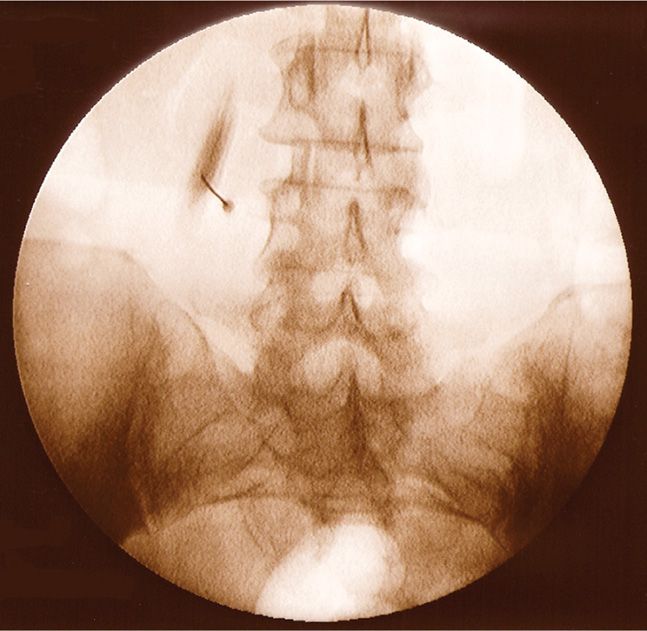
Figure 60-6. Fluoroscopic imaging of psoas injection with contrast in the muscle. (Used with permission from Andrea Trescot, MD.)
• A transforaminal approach at L1 and/or L2 can be used to address the nerve proximally (Figure 60-7).

Figure 60-7. Fluoroscopic imaging of the L1 foramen. (Used with permission from Andrea Trescot, MD.)
Equipment
• Peripheral injection
![]() 30-gauge needle for subcutaneous infiltration
30-gauge needle for subcutaneous infiltration
![]() 25- or 22-gauge Quincke needle
25- or 22-gauge Quincke needle
![]() 3-cc Luer lock syringe for local anesthetic
3-cc Luer lock syringe for local anesthetic
![]() Sensory nerve stimulator with alligator clip or other connections for grounding ECG pad and needle
Sensory nerve stimulator with alligator clip or other connections for grounding ECG pad and needle
• Psoas injection
![]() 30-gauge needle for subcutaneous infiltration
30-gauge needle for subcutaneous infiltration
![]() 22-gauge Quincke needle
22-gauge Quincke needle
![]() Sensory nerve stimulator with alligator clip or other connections for grounding ECG pad and needle
Sensory nerve stimulator with alligator clip or other connections for grounding ECG pad and needle
• Transforaminal injection
![]() 30-gauge needle for subcutaneous infiltration
30-gauge needle for subcutaneous infiltration
![]() Blunt-tipped needle and introducer (22 gauge Whitacre or Epimed)
Blunt-tipped needle and introducer (22 gauge Whitacre or Epimed)
![]() 3-cc Luer lock syringe for local anesthetic
3-cc Luer lock syringe for local anesthetic
![]() Extension tubing
Extension tubing
![]() Sensory nerve stimulator with alligator clip or other connections for grounding ECG pad and needle
Sensory nerve stimulator with alligator clip or other connections for grounding ECG pad and needle
Medications
• Local anesthetic
• Depo-steroid
• Nonionic contrast for psoas and transforaminal approach
Technique
Diagnostic Injection (anterior blind approach)
The patient is placed supine with a pillow under the knees.
• Anatomic landmarks
![]() Pubic tubercle
Pubic tubercle
![]() Inguinal ligament
Inguinal ligament
![]() Inguinal crease
Inguinal crease
![]() Femoral artery
Femoral artery
• There are two sites of injection
![]() At the inguinal ring
At the inguinal ring
![]() At the pubic tubercle
At the pubic tubercle
• Use of a peripheral stimulator improves accuracy and allows for low volume diagnostic injections (ideally less than 2 cc total volume).
• Note: Injections of the ilioinguinal nerve at the inguinal ring may also anesthetize the GFN, but ilioinguinal injections at the ASIS will not affect the GFN.
Diagnostic Injection (anterior fluoroscopic approach)
• The pubic tubercle is identified by palpation and then fluoroscopy.
• The GFN lies just lateral to the pubic tubercle (Figure 60-3).
• Use of a peripheral stimulator improves accuracy (Figure 60-4) and allows for low-volume diagnostic injections (ideally less than 2 cc total volume).
Diagnostic Injection (transpsoas approach—blind or image-guided)
The patient is placed prone and the L3 or L4 transverse process identified approximately 5 cm from the midline (by landmarks, fluoroscopy, or CT).6
• For the blind approach, a 22-gauge subarachnoid needle is advanced between the L3 and L4 transverse processes, using a loss-of-resistance technique to identify the anterior surface of the psoas. 10 cc of local anesthetic is then injected.
• Fluoroscopically, the psoas muscle is identified at the level of L3 (Figure 60-5). A 22-gauge subarachnoid needle is advanced into the body of the muscle, and 1 cc of nonionic contrast injected to confirm the intramuscular positioning (Figure 60-6). The needle is then advanced to just anterior to the muscle, using a loss of resistance technique. 2 cc of local anesthetic is then injected (less if a nerve stimulator is used).
• Using CT guidance, the entry site just above the L4 transverse process is identified. IV contrast is injected to opacify the ureters, and a 22-gauge 5-in Quincke or Chiba needle advanced through the muscle onto the surface of the muscle.
Diagnostic Injection (transforaminal approach)
By addressing the nerve at its most proximal site, it is possible to anesthetize the nerve proximal to any pathology.
• Identify the L1 vertebral body, and align the upper endplate using fluoroscopic image.
• Identify the pedicle and the nerve foramen below it from an AP or oblique view (Figure 60-7).
• Advance a blunt-tipped needle into the foramen (see Chapter 22 for complete details)
![]() Use of a peripheral stimulator will facilitate identification of the nerve.
Use of a peripheral stimulator will facilitate identification of the nerve.
![]() Stimulation of the posterior lumbar area reflects stimulation of the cluneal nerve, which exits from the same foramen. In that case, the needle needs to be repositioned more anteriorly.
Stimulation of the posterior lumbar area reflects stimulation of the cluneal nerve, which exits from the same foramen. In that case, the needle needs to be repositioned more anteriorly.
![]() Nonparticulate steroid, and real-time injection of contrast are expected to decrease the risk of transforaminal injection of the radicular artery, which has been associated with spinal cord infarct, paralysis, and death.
Nonparticulate steroid, and real-time injection of contrast are expected to decrease the risk of transforaminal injection of the radicular artery, which has been associated with spinal cord infarct, paralysis, and death.
Neuroablation
• If there was excellent but only temporary relief with the peripheral or transforaminal diagnostic injections, cryoneuroablation can be used to kill the nerve (see Chapter 79).
![]() For the peripheral technique, the cryo probe is placed on the pubic tubercle (Figure 60-8) under fluoroscopic control. The built-in peripheral stimulator is used to find the nerve.
For the peripheral technique, the cryo probe is placed on the pubic tubercle (Figure 60-8) under fluoroscopic control. The built-in peripheral stimulator is used to find the nerve.

Figure 60-8. Cryoneuroablation of the genitofemoral nerve at the pubic tubercle. (Used with permission from Andrea Trescot, MD.)
![]() An ultrasound GFN cryoneuroablation technique has also been described.7
An ultrasound GFN cryoneuroablation technique has also been described.7
![]() For the transforaminal technique, the cryo probe is placed just inside the foramen (Figure 60-9). The built-in peripheral stimulator is used to find the nerve.
For the transforaminal technique, the cryo probe is placed just inside the foramen (Figure 60-9). The built-in peripheral stimulator is used to find the nerve.

Figure 60-9. Cryoneuroablation of the genitofemoral nerve at the L1 foramen. (Used with permission from Andrea Trescot, MD.)
• Although pulsed radiofrequency treatment has been described for several peripheral nerves, in the US it is not a covered procedure.
• Heat radiofrequency lesioning on the anterior surface of the psoas has been described, but was not successful.6
• Phenol injections, 4%, have been described for a variety of peripheral nerves, including the GFN.8 The use of 7% phenol in myelographic contrast via a transpsoas approach has been described.6 Absolute alcohol has also been used for peripheral neuralgia.
POSTPROCEDURE FOLLOW-UP
Evaluate the patient immediately after the procedure for presence of sensory block and pain relief secondary to local anesthetic effect. Patient should be evaluated by subsequent telephone or office follow-up for potential complications as well as significance and length of time of pain relief, including evaluation of the effect from the deposteroid.
POTENTIAL COMPLICATIONS AND PITFALLS
• Since the diagnostic block, radiofrequency, or cryoanalgesia procedures are primarily subcutaneous (at least for the distal approaches), they are associated with few complications. There is a chance of hematoma and postinjection ecchymosis.
• The transpsoas injection is retroperitoneal, but the possibility of peritoneal penetration and colon perforation exists.
• Destruction of surrounding non-nerve tissue is a complication of phenol and absolute alcohol.
CLINICAL PEARLS
• Genitofemoral nerve blocks at the pubic tubercle are relatively simple procedures that can provide near complete pain relief, at least temporarily, if the diagnosis is correct.
• These injections can be diagnostic or therapeutic. The patients with positive diagnostic but not therapeutic effects are candidates for an ablation procedure using cryoneuroablation, pulsed radiofrequency lesioning or phenol/alcohol.
• Pressure should be applied to the injection site for prevention of hematoma and ecchymosis, especially for large cannula procedures such as cryoneuroablation.
• Absolute alcohol and phenol injections should only be utilized for pain patients with limited lifespan who suffer from intractable genitofemoral neuralgia.
• The success of the diagnostic procedure is most dependent on accurate placement of the nerve stimulation needle.
• If patients present with genitofemoral pain and do not get relief from a diagnostic block, then consider L1 or L2 nerve root pathology. Also consider pudendal nerve pathology in refractory cases.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






