| Viral | • Hepatitis –A, B, D, E • Herpes simplex virus • Cytomegalovirus • Epstein–Barr virus • Herpes varicella zoster • Adenovirus |
| Drugs and toxins | • Acetaminophen • Carbon tetrachloride • Sulfonamides • Tetracycline • Isoniazid • NSAIDs • Rifampicin • Valproic acid • Disulfiram • Amanita phalloides • Bacillus cereus toxin • Herbal supplements |
| Vascular | • Budd–Chiari Syndrome • Shock liver • Right heart failure • Veno-occlusive disorder |
| Metabolic | • Acute fatty liver of pregnancy • HELLP syndrome • Wilson disease • Reye syndrome • Galactosemia • Hereditary fructose intolerance • Tyrosinemia • Alpha-1 antitrypsin deficiency |
| Miscellaneous | • Primary graft failure/dysfunction of transplanted liver • Autoimmune hepatitis |
Presentation
Classic presentation
- Typically patients present with nonspecific symptoms:
- Fatigue
- Malaise
- Anorexia
- Abdominal pain
- Jaundice.
- Fatigue
Critical presentation
- Patients can present with:
- Hypotension due to generalized systemic inflammatory response
- Coagulopathy
- Encephalopathy with progression to coma and brain herniation (Table 38.2).
- Hypotension due to generalized systemic inflammatory response
Table 38.2. Grading of hepatic encephalopathy
Diagnosis and evaluation
- Diagnosis
- Diagnosis is made based on clinical presentation and laboratory findings. Consider the tests listed below (though many will not be reported back within a few hours of the ED stay).
- Chemistry: Acetaminophen level, alpha-1 antitrypsin level, alpha-1 antitrypsin phenotype, ammonia level, amylase, lipase, ceruloplasmin, cholesterol, comprehensive metabolic panel, magnesium, phosphorus, gamma-glutamyl-transferase (GGT), lactate dehydrogenase (LDH), lactic acid, uric acid, pregnancy screen.
- Immunology: Mitochondrial M2 Ab IgG, anti-nuclear Ab screen (ANA, IgG), smooth muscle Ab, IgG, IG heavy chain quantitation, alpha fetoprotein tumor marker.
- Hematology/coagulation: Antithrombin III activity assay, CBC, D-dimer, factor V, VII, and VIII, fibrinogen, MOCHA (markers of coagulation hemostatic activation), PT, PTT, INR.
- Microbiology/infectious disease: CMV antibody total (anti-CMV Ab), CMV antibody IGM, IgG, Coxsackie B virus Abs, Epstein–Barr virus Ab profile, hepatitis A Ab total and IgM, hepatitis B DNA quantification, hepatitis B diagnostic profile, hepatitis C Ab, herpes simplex virus DNA by PCR, HIV antigen Ab combo, rapid plasma reagin test.
- Urine: Urine sodium, urine creatinine, 24-hour urine copper level, toxicology drug screen especially acetaminophen, urinalysis.
- Imaging: Abdominal ultrasound (US) with Doppler, noncontrast head CT, abdomen MRI with and without contrast, transthoracic US.
- Diagnosis is made based on clinical presentation and laboratory findings. Consider the tests listed below (though many will not be reported back within a few hours of the ED stay).
- Prognosis
- Three possible outcomes:
- Spontaneous survival without liver transplantation (>40%)
- Orthotopic liver transplantation (25%)
- Death (33%).
- Spontaneous survival without liver transplantation (>40%)
- The shorter the interval between jaundice and the development of hepatic encephalopathy the higher the likelihood of spontaneous survival.
- King’s College Criteria:
- Used to determine prognosis and need for transplant.
- If the patient satisfies any of the following criteria, they most likely will require a liver transplant to survive.
- Acetaminophen-induced disease:
- Arterial pH <7.3
or all of the following:
- grade III or IV encephalopathy
- Prothrombin time >100 seconds
- Serum creatinine >3.4 mg/dL (301 micromol/L).
- Arterial pH <7.3
- All other causes of hepatic failure:
- Prothrombin time >100 seconds (INR>6.5)
or any three of the following:
- Age <10 years or >40 years
- Etiology: non-A, non-B hepatitis, halothane hepatitis, idiosyncratic drug reactions
- Duration of jaundice before onset of encephalopathy >7 days
- Prothrombin time >50 seconds
- Serum bilirubin >18 mg/dL (308 micromol/L).
- Prothrombin time >100 seconds (INR>6.5)
- Used to determine prognosis and need for transplant.
- Three possible outcomes:
Critical management
- Progression of disease can be quite rapid; patients should be transferred to a transplant center as soon as possible.
- Critical care management as needed for cardiovascular, pulmonary, and infectious complications and other comorbidities.
- Acetaminophen toxicity
- Prognosis and treatment decisions can be based on Rumack–Matthew nomogram (Figure 38.1).
- It is important to remember that the nomogram is based on a single ingestion and may not apply if the time of ingestion is unknown or in the cases of multiple ingestions.
- N-Acetylcysteine (NAC):
- NAC should always be given in acetaminophen toxicity except for rare occasions.
- NAC is indicated for all levels where toxicity is possible.
- Given the limitations of the nomogram, NAC should be administered if there is any doubt of the amount or time of ingestion(s). Furthermore, NAC may be beneficial even late after ingestion.
- Watch for anaphylactoid reaction with IV NAC. Typically, this reaction will be abated by decreasing the rate of infusion, administering antihistamines, and providing supportive care. If the reaction is severe, stop the infusion, treat with antihistamines, and consider restarting after the symptoms improve.
- NAC should be continued until the end of the protocol and until evidence of severe liver injury resolves (usually when AST and ALT are <1000).
- NAC should always be given in acetaminophen toxicity except for rare occasions.
- Prognosis and treatment decisions can be based on Rumack–Matthew nomogram (Figure 38.1).
- Management of complications related to liver failure
- Neurological
- Frequent neurological checks; worsening hepatic encephalopathy may be due to progression to cerebral edema.
- Minimize sedation to avoid confusing drug effects with clinical deterioration. When needed, choose short-acting agents.
- Management of hepatic encephalopathy:
- Grade III encephalopathy requires intubation for airway protection.
- Consider CT scan to evaluate for cerebral edema and rule out other causes of altered mental status; however, remember that a normal scan does NOT rule out cerebral edema.
- Herniation is unlikely with ammonia levels <150 micromol/L.
- Consider intracranial monitoring in the following patients:
- Grade III and higher encephalopathy
Markedly elevated ammonia levels
- Unlike with chronic hepatic failure, lactulose has not been proven to have any long-term benefit in acute fulminant hepatic failure
- Grade III encephalopathy requires intubation for airway protection.
- Management of cerebral edema/elevated intracranial pressure (ICP)
- Goals ICP <20 mmHg and CPP >60 mmHg (CPP = MAP − ICP). Even if no ICP monitoring available, it is important to manage grade III and higher encephalopathy as if ICP is known to be elevated.
- Basic management:
- Sedation and muscle relaxation as needed
- Keep environment calm with little stimulation
- Position HOB at 30–45 degrees
- Keep head in midline position to allow the jugular veins to drain
- Minimize other adjuncts to care such as suctioning or laying supine for turns
- Consider specific treatments to prevent elevated ICP during intubation (i.e., IV lidocaine and muscle relaxants)
- Avoid hypoventilation. Hyperventilation is not necessary and may cause cerebral vasoconstriction leading to cerebral ischemia.
- Correct hyponatremia
- Control fever and seizures
Osmotic therapy:
- Indicated for severe intracranial hypertension defined as sustained ICP>20–25 mmHg for >5–10min
- Mannitol
- Avoid if serum osmolality >320 mOsm/L or with renal failure.
- Can cause renal toxicity.
- Avoid if serum osmolality >320 mOsm/L or with renal failure.
- Hypertonic saline
- May be better osmotic agent than mannitol.
- No diuretic properties.
- No renal toxicity.
- Goal Na = 145–155 mmol/L.
- Careful when discontinuing hypertonic saline; wean to avoid abrupt drop in sodium and rebound cerebral edema.
- May be better osmotic agent than mannitol.
- Consider mild hypothermia for refractory cases:
- Goal 32–33°C
- Control shivering
- Burst suppression on EEG/phenobarbital coma.
- Goal 32–33°C
- Coagulopathy:
- Typically, clinically important bleeding infrequent despite coagulopathy.
- FFP for elevated INR with acute bleeding or prior to procedure.
- Vitamin K may be administered for elevated INR without acute bleeding.
- Give cryoprecipitate if fibrinogen <100 mg/dL.
- If actively bleeding, attempt to maintain platelet count >50 000. In the absence of bleeding, maintain platelet count >10 000.
- Consider activated recombinant factor VII in refractory cases (use only if placing an intracranial monitor).
- Typically, clinically important bleeding infrequent despite coagulopathy.
- Goals ICP <20 mmHg and CPP >60 mmHg (CPP = MAP − ICP). Even if no ICP monitoring available, it is important to manage grade III and higher encephalopathy as if ICP is known to be elevated.
- Frequent neurological checks; worsening hepatic encephalopathy may be due to progression to cerebral edema.
- Hypoglycemia
- Maintain blood glucose >70 mg/dL (3.9 mmol/L).
- Administer dextrose in the form of bolus and drip as needed.
- Bolus dextrose 50%, 50 mL via IV push.
- Start a drip since most of these patients will require a continuous glucose source – D5W, D10W, or D20W and titrate rate to goal blood glucose >70 mg/dL (3.9 mmol/L).
- Check blood glucose every 30 minutes until the goal is reached.
- Maintain blood glucose >70 mg/dL (3.9 mmol/L).
- Renal failure
- Renal failure occurs in up to 50% of cases, even more frequently in acetaminophen toxicity.
- Avoid nephrotoxins.
- Management of hypervolemia is crucial to reducing cerebral edema.
- In most cases continuous renal replacement therapy is indicated.
- Avoid intermittent hemodialysis as some evidence suggests rapid fluid shifts lead to brain herniation.
- Renal failure occurs in up to 50% of cases, even more frequently in acetaminophen toxicity.
- Neurological
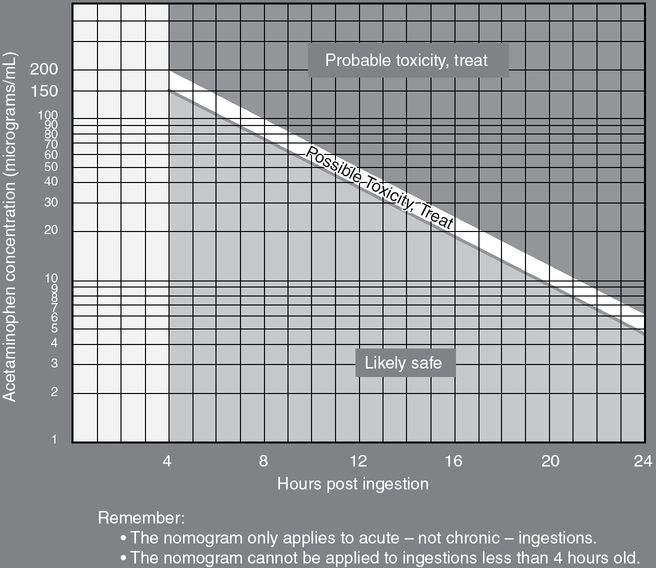
Figure 38.1. Rumack–Matthew nomogram. (Courtesy of Dr. Graham Walker.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




