Sagittal T1 weighted MRI image demonstrating an ACL tear (Raukar)
Although the ACL can be reconstructed after injury, stabilizing the knee and decreasing “giving way” episodes, reconstruction does not protect patients from developing secondary osteoarthritis (OA) as a direct result of articular cartilage injury sustained at the time of ACL damage. Women, in particular, are at greater risk than men for developing OA of the knee after ACL injury and may develop OA at an earlier age, often 10 years after the initial injury. ACL injury and the subsequent development of osteoarthritis can be life altering; therefore, prevention of ACL injury is crucial. Effective prevention programs incorporate strengthening of the muscles and ligaments that support the knee and protect the ACL and posterior cruciate ligament (PCL) and stretching exercises, balance training, plyometrics, and an emphasis on learning and practicing appropriate and safe landing positions (i.e., landing with both hips and knees flexed, on the balls of the feet, the so-called light as a feather landing).
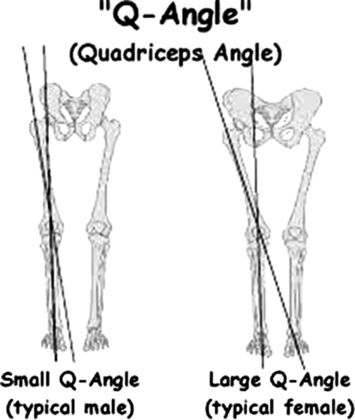
The Q Angle (Becker)
Other Knee Injuries
The anatomic lower extremity alignment in women that predisposes them to ACL injuries (i.e., internal rotation of the hip and valgus stress of the knee with external rotation of the tibia) also creates excessive force on the patellofemoral joint, increasing women’s risk of patellofemoral subluxation (Arom et al. 2013). The Q angle is the angle formed by a line drawn from the anterior superior iliac spine to the center of the patella and a line drawn from central patella to the tibial tubercle, measured and subtracted from 180 degrees (Figure 8.2). Women have an increased Q angle (17 degrees vs. 14 degrees in men) placing them at greater risk for patellofemoral subluxation (Waterman et al. 2012) because of the direct effect of this angle on the force vector of the quadriceps. There is some controversy about the relative impact of the Q angle, which is measured statically when the athlete is at rest and may not accurately reflect active alignments and stresses on the knee during sports. While the static and active alignment of women’s lower extremities as well as their relatively more lax connective tissue seem to be responsible for their increased risk of patellofemoral subluxation and anterior knee pain syndromes, the incidences of patellar dislocation and knee dislocation do not differ by sex (Iguchi 2014). These injuries always result from a significant impact, rather than the repetitive trauma that leads to anterior knee pain or patella subluxation. Furthermore, knee dislocation leads to vascular compromise and peroneal nerve injury more frequently in men (Natushara 2014), most likely reflecting the increased shearing forces associated with the dislocating trauma that is the usual cause of this injury (Peskun et al. 2012).
Women are more prone to sustain ACL injuries, with a female:male ration of 7:1.
The acute care provider must maintain a high level of suspicion for ACL injury when a female athlete presents with an acutely swollen knee after landing a jump or performing a rapid change of direction while running (“a cutting maneuver”). This risk is higher if she has sustained a prior ACL injury.
Delays in diagnosis, stabilization, and treatment may result in significant knee stiffness and loss of Range of Motion, which must be addressed prior to surgical reconstruction.
Women suspected of having an ACL tear should ice their knee, limit weightbearing, and urgently follow up with their orthopedic surgeon.
Ankle/Foot
Sports-related injuries of the foot and ankle are often multifactorial. Differences between men and women in the neuromuscular control of landing mechanisms also affect the loading stresses of the foot and ankle. This variable loading mechanism is believed to underlie the increased risk of fifth metatarsal fractures and Achilles tendon ruptures in men. Overall, men sustain more ankle sprains than women; nevertheless, in specific sports, such as basketball, women are four times more likely than men to sustain type 1, but not type 2 or 3 ankle sprains, syndesmotic injuries, or ankle fractures (Lynch, 2002). Surprisingly, although kinesthetics vary across sports, men demonstrate no sport-specific increase in the risk of ankle injury. Sex hormones do not seem to play a role in women’s propensity for ankle sprains. While rising estradiol levels increase women’s ankle joint laxity, there is no established correlation between phase of the menstrual cycle and risk of injury.
One of the most common pathologies of the foot is hallux valgus, a painful syndrome caused by the lateral deviation of the great toe (Hecht and Lin 2014; Perera 2011). Women are twice as likely as men to have hallux valgus. The pathogenesis is complex but seems to be related to wearing shoes with a small toe box (Nguyen et al. 2010). The incidence of hallux valgus deformity has been reported in as many as 48% of women who wear “fashion” shoes, as compared to 16% to 33% of shoe-wearing men and 2% of the unshod. Interestingly, even in barefoot populations, hallux valgus deformity is more common in women than in men (Shine 1965; McLennan 1966).
Upper Extremity
Almost no data compare male and female athletes’ upper extremity injury rates. The sex differences in ACL injury rate patterns have not been demonstrated for upper extremity injuries. Upper extremity injury rates by sex appear to reflect the kinesthetics and motor tasks associated with particular sports and their attendant risks. For example, sports involving a repetitive overhead throwing motion such as softball and baseball consistently demonstrate a high incidence of shoulder or elbow injury (Bigliani 1997; Kvitne et al. 1995). While a single traumatic event in any sport may cause injury, repetitive overuse more commonly leads to failure and damage of one or more of the musculoskeletal structures of the upper extremity.
Case
A 17-year-old woman who is right-hand dominant presents to the ED with an obvious right shoulder deformity. She was pitching a softball game and suddenly felt her shoulder “lock.” Since then, she has been holding her arm close to her side, adducted, with her shoulder externally rotated.
Clinical Questions
How should you approach the work up in this patient?
What are the sex-specific elements in diagnosis and management that you should consider?
Shoulder
Fewer sex-specific differences have been reported for the shoulder than for the knee. The shoulder is the most commonly dislocated joint; the estimated incidence rate for shoulder dislocation is 23.9 per 100,000 (Zachilli 2010). When describing shoulder dislocations, health care providers generally use the location of the humeral head (e.g., anterior vs. posterior). Other classification systems are more useful for identifying the mechanism of instability. Using these descriptors, shoulder dislocations can be described in three ways:
Traumatic dislocations are more common in men (71.8%) and demonstrate unidirectional instability; atraumatic dislocations are more common in women with multidirectional instability patterns (Zachilli 2010). Sports that put repetitive strain on the shoulder joint such as softball, swimming, volleyball, and gymnastics are associated with the greatest rates of shoulder dislocation among women athletes.
In the United States, the prevalence of shoulder instability (including dislocation and subluxation) in athletes has been documented for both men and women. The overall incidence rate is 23.9 per 100,000 person-years with male incidence at 34.90 per 100,000 person-years, and occurs 2.64 times more frequently in men than women (Zacchilli 2010).
The shoulder is a complex ball and socket joint: The humeral head sits on a shallow glenoid that is deepened by a collagenous labrum and capsule and supported by surrounding soft tissues. Dynamic stabilizers of the glenohumeral joint include the rotator cuff muscles, the scapulo-thoracic muscles, and the long head of the biceps tendon. Static stabilizers include the bony anatomy, the fibro-cartilaginous labrum, and the glenohumeral joint capsule. Shoulder instability variances between the sexes can be attributed to static restraints (collagen elasticity due to the action of hormones), dynamic restraints (altered stabilizer muscle firing patterns), and differences in proprioception. Multidirectional instability is characterized by symptomatic global laxity of the glenohumeral joint and is believed to be more prevalent in women. Female athletes are thought to have greater glenohumeral instability than their male counterparts (Borsa et al. 2000) because their shoulders demonstrate more anterior glenohumeral joint laxity, less anterior joint stiffness, and more joint hypermobility (Cameron 2010). It is important to note that pre-injury measurements of shoulder laxity may not reflect true dynamic instability or a predisposition to dislocation.
Women have decreased proprioceptive responsiveness in their shoulder joints, which causes a slowing of the reactive contraction of the supporting muscles, increasing the risk of structural damage to the shoulder in response to stress (Blasier et al. 1994; Blasier 1992). When compared to nonathletic subjects, both male and female athletes participating in overhead throwing sports displayed greater joint stiffness; these studies suggest that conditioning and training decrease joint laxity. Shoulder joint laxity is also asymmetric; anterior and posterior laxity differs and this variance is found in men and women (Comstock 2013; McFarland et al. 1996). This directional asymmetry is nonspecific and demonstrates no consistent pattern: It is not known whether this asymmetry plays a role in injury risk for either sex.
Labral tears, particularly tears of the superior aspect of the labrum that involve the biceps anchor, are common in athletes who throw overhand. Burkhart and Morgan proposed that the superior labrum tears from anterior to posterior, so-called SLAP lesions, are caused by a ‘‘peel-back’’ mechanism in these athletes, resulting from the increased strain at the biceps anchor during the late cocking phase of the throw when the shoulder is at maximum external rotation (Burkhart & Morgan 1998). Kuhn et al. showed an increased incidence of SLAP lesions in male baseball pitchers, supporting the peel-back theory (Kuhn et al. 2005). Shoulder injuries are prevented primarily by engaging in specific stretching and strengthening exercises of the rotator cuff and proper warm-up routines prior to strenuous shoulder activity. The risk for labral tears seems to be sports specific: No available data indicate sex-specific differences.
The majority of rotator cuff injuries suffered by overhead throwing athletes involve articular-sided partial-thickness tears of the rotator cuff, which are caused by acute tensile overload, repetitive microtrauma, or both (White et al. 2014; Burkhart et al. 2003). This pattern of injury is commonly found postero-superiorly, at the junction of the infraspinatus (IS) and supraspinatus (SS) tendon insertions (Jobe 1995; Walch et al. 1992; Minachi 2002). As women get older, the risk of rotator cuff injuries involving the IS and SS tendons increases. The most common etiologies of rotation cuff–related pain or injury for both men and women are subacromial impingement syndromes or repetitive microtrauma. This form of rotator cuff injury, which is strongly correlated with aging, is much more common in women, especially those in the 55- to 59-year-old group (Jobe 1995).
Elbow
Most elbow injuries in athletes are due to repetitive overuse from overhead activities, throwing, or elbow weight-bearing sports such as gymnastics. Depending on the specific nature of the athlete’s sport, these injuries occur in predictable anatomic locations. For example, for both sexes, an increased incidence of injuries has been reported in the capitellum as a result of repetitive trauma in upper extremity weight-bearing activities (Baker et al. 2010). During the late cocking and acceleration phases of the throwing motion, tremendous valgus stress is placed on the elbow joint. The resulting distractive forces along the medial aspect of the elbow create tensile stress for structures such as the ulnar collateral ligament (UCL), common flexor tendon, and ulnar nerve. The radio-capitellar joint is subjected to compressive forces, and the postero-medial joint, particularly the humeral-olecranon articulation, experiences shear forces. These biomechanics often lead to a constellation of elbow injuries in the throwing athlete that are often referred to as the “valgus overload syndrome” (Cain et al. 2003; Chen et al. 2001). Injuries include UCL sprains or tears, common flexor tendon inflammation or tear, ulnar neuritis, and osteoarthritic changes of the ulnohumeral joint (Anderson et al. 2010).
Most women have shorter upper extremities than men, an increased valgus-carrying angle, decreased upper extremity strength, and increased ligamentous laxity in the elbow (Ireland and Ott 2004). However, because of the excessive stress placed on the elbow during the overhand pitching motion of baseball as opposed to softball, which is pitched underhand, severe elbow injuries, such as UCL tears, remain more common in male athletes. Elbow dislocations are the result of trauma and are not the result of ligamentous laxity or structural anatomic differences in the elbow between the sexes. Trauma is more common in men; therefore, elbow dislocations are more common in men. Men tend to have stronger and larger upper extremity musculature; therefore, elbow dislocations in women can result from less forceful injuries such as falling on an outstretched hand. The incidence rate ratio of elbow dislocations males:females is 1.02 (5.26 per 100,000 for males and 5.16 per 100,000 for females) (Stoneback et al. 2012).
Hand and Wrist
Contact injuries in sports such as ice or field hockey or lacrosse can result in fractures of the hand or wrist. Overuse injuries to the wrist are common in gymnastics, golf, weightlifting, racquet sports, and bicycling. In gymnastics, the upper extremity becomes a weight-bearing limb; studies have found the incidence of wrist pain in gymnasts to be as high of 73% (Diffiori 1996). The differential diagnosis in chronic wrist pain in any athlete includes triangular fibrocartilage tears, ulnar impaction syndrome, dorsal wrist ganglion, dorsal wrist capsulitis, and carpal instability. Other possible sources of wrist pain are hamate fracture, carpal tunnel syndrome, tendinitis, and ulnar nerve compression. This constellation of injuries appears to be sports specific; no consistent data demonstrate sex-based differences in incidence or prevalence of these hand and wrist injuries.
Musculoskeletal Pain Syndromes
Pain is a common presenting complaint for patients seeking treatment in an Emergency Department; one study found that 40.6% of patients who presented to the ED with a musculoskeletal complaint had a non-acute, low-severity problem (Naturshara 2014). In 2004, 13.8% of the 110 million ED visits were directly attributable to a primary musculoskeletal disorder; more than one-third of these visits were categorized as either semi-urgent or nonurgent (McCraig 2006), including visits for “chronic pain.” Back pain is one of the most common chief complaints of patients presenting to the ED (Pitts, 2006), and a majority of those patients are women. Patients with chronic neck or low back pain who have no inciting trauma, no systemic symptoms, and no significant changes in neurologic findings do not require acute evaluation or intervention. Neither plain films nor CT scans nor MRIs are of demonstrated benefit in the ED or acute care setting.
Chronic regional pain syndrome (CRPS), also known as reflex sympathetic dystrophy, is a known occasional sequela of orthopedic trauma, including fractures and crush injuries. Surprisingly, it can also be seen after minimal injuries and after minor procedures, including needlesticks. Patients with CPS often present with pain out of proportion to the inciting injury, such as patients with limb ischemia from peripheral vascular disease. They can present at any time after their event. Unfortunately, the cause of the pain has not been elucidated and treatment is challenging. CRPS is much more common in women, with a prevalence ratio of 4:1 females:males (Field 2013).
Contractures are a permanent tightening of soft tissue caused by fibrosis, specifically, fibrosis of ligaments, tendons, and muscles. Histologically, contractures are characterized by inflammation, myofibroblast proliferation, and dense scar formation. Examples of contractures include Dupuytren’s (contractures of the palmar fascia), Ledderhose (contractures of the plantar fascia), and adhesive capsulitis (contractures of the glenohumeral joint capsule). Classically associated with alcoholism, these conditions can also be the result of diabetes, trauma, and chronic phenytoin use. Men are primarily affected by Dupuytren’s and Ledderhose’s contractures, while women have a higher incidence of adhesive capsulitis. Dupuytren’s contracture is reported to be up to nine times more common in men than in women.
Case
A 17-year-old woman has been training for the past six months to make the varsity high school track team. She has been running six to seven miles per day, six days a week, and biking on the seventh day. She has not changed her diet and eats as much as she did before she started training, but her parents report she is strict about limiting her fat intake. She states she is “the most athletic that she has ever been.” She presents with a four-week history of progressive right leg pain that initially started at the end of one of her runs but now occurs as soon as she starts to run. She even feels the pain when she walks up and down stairs; the pain is impinging on her lifestyle. Physical exam reveals bony point tenderness along the mid-shaft of her tibia on the right. There is no warmth or erythema suggestive of cellulitis or infection. The patient states she is not sexually active; however, her last menses was three months prior to this presentation. A urine pregnancy test was negative.
Clinical Questions
How would you approach the work up in this patient?
What do you do if radiographs are negative?
What are the sex- and gender-specific elements in diagnosis and management that you should consider?
Are there specific referrals that should be made, and to whom?
Athlete Energy Imbalance
Athletic energy imbalance (AEI), which was formerly known as the female athlete triad, was first described by Drinkwater in 1984 and defined by the American College of Sports Medicine in 1993. The definition has evolved and is currently defined as low energy availability, menstrual disturbance, and low bone mineral density (Nazem and Ackerman 2012). Menstrual irregularity can include hypothalamic primary or secondary amenorrhea, luteal phase deficiency, or oligomenorrhea; disordered eating may include anorexia or bulimia or, most frequently, an inadequate number of calories consumed relative to the athlete’s expenditure. The most common self-imposed dietary restriction is limiting consumption of fat. These athletes will also have inadequate bone mass that can span a spectrum from osteopenia to osteoporosis. Since each of the three AEI entities is a continuum of deficiency and pathology, the triad of AEI can be seen in both competitive and recreational athletes. While insufficient caloric consumption with a negative effect on bone health is most common in women, it can also be seen in men.
AEI can produce morbidity and even mortality in relatively young women (Torrsveit 2005). The long-term effects are often not appreciated or diagnosed until they become irreversible. There is a severe deficiency in health care practitioners’ knowledge, understanding, recognition, and diagnosis of AEI. In one study, an unacceptably large proportion of physicians were unable to name all three components (Troy et al. 2006). In addition, health care workers, coaches, and team physicians may consider athletes with AEI to be “healthy,” as their diet may not appear abnormal and their physical appearance may conform to societal norms for an athletic woman who is “cut” or “toned.” Often these athletes are not appropriately screened for components of the triad. However, health care providers, trainers, and coaches must assess caloric intake in relationship to known training expenditure. Athletes are frequently unwilling to address this condition, even after having sustained an injury, because their low body weight may make them successful in their sport. This condition is most often seen in a population of athletes who engage in a high level of competition from a young age, particularly in sports where leanness or a slender appearance affects performance, such as gymnastics, ice skating, cycling, and track.
It was once believed that the three components of this condition were separate entities with some interrelationship: The energy deficiency resulting from disordered eating could be associated with the development of menstrual disturbances; these hormonal disturbances might contribute to bone loss. It is now believed that each component of the triad is deeply interrelated with the other components: Relative low caloric intake results in both menstrual dysfunction and bone loss. The bone loss seen with AEI represents a low bone turnover state, in contrast to the accelerated bone resorption seen with estrogen deficiency. Markers of bone formation normalize in the face of increased caloric intake or decreased caloric expenditure before menses resume.
The reproductive and skeletal deficits are the result of a relative lack of energy from disordered eating in the face of increased energy expenditure. Energy availability is the difference between dietary energy intake and energy expenditure. In animal studies, reducing caloric intake by more than 30% consistently caused infertility and skeletal demineralization (Merry and Holehan 1979). The resting metabolism of the young adult is 30 kcal·kg−1 FFM·d−1. Usually, when energy requirements are not met, hunger is triggered; however, in the athlete practicing dietary restriction, the energy deficit produced by exercise does not necessarily trigger hunger or that athlete does not respond to that hunger. When the energy available to young female athletes is reduced by more than 33% from 45 to less than 30 kcal·kg−1 FFM·d−1, a cascade is triggered with attendant effects on sports performance and bone demineralization (Loucks and Heath 1994). Acute care practitioners must be aware of AEI to identify these patients, mostly female athletes, when they present for an injury or other complaint. If possible, these patients should be counseled on appropriate caloric intake, apprised of the athletic and health implications of AEI, asked to keep a food log, and encouraged to share this food log with their sports nutritionist or family physician.
Menstrual irregularity is the second part of the triad and is theorized to arise from decreased production of GnRH by the hypothalamus (hypothalamic amenorrhea). The effects of primary or secondary amenorrhea, oligomenorrhea, and luteal phase deficiency on the hormonal profile are different. The end result, though, is reproductive dysfunction with an altered cholesterol profile.
The third arm of this condition, low bone mass, typically manifests as a stress fracture (or fatigue fracture). Stress fractures occur in athletes whose long bones are subjected to the cumulative effects of repeated microtrauma, without time for bone healing; healing is particularly impaired in athletes whose bone metabolism has slowed. Both bone microtrauma and slowed bone metabolism are seen in patients with athlete energy imbalance. For those athletes with normal bone mineralization, stress fractures are seen when the athletes rapidly change their training regimen or increase their intensity of activity; stress fractures are also seen in female military cadets (Cosman et al. 2013). Female athletes who present to the ED should be specifically asked about their menses, caloric intake, and exercise regimen; if there is evidence of amenorrhea, they should be referred to a gynecologist.
The young menstruating female should gain 2% to 4% of bone mass annually; unfortunately, the amenorrheic female loses 2% of her bone mineral density (BMD) per year. Even if a normal menstrual cycle is achieved after a period of menstrual irregularity, BMD rarely fully recovers (Rose 2001). Most women achieve 95% of their peak bone mass by age 18; unless other health conditions intervene, bone mass remains relatively stable from age 30 until menopause. Those who do not achieve optimal peak bone mass are more likely to sustain fragility fractures at an earlier age. Thus, BMD gained during adolescence is essential for adult skeletal health (Skolnick 1993). Bone mineral density is measured against a standard that has been developed by sampling normal, healthy women of similar age.
In 1993, an international consensus conference sponsored by what is now known as the International Osteoporosis Foundation and the American National Osteoporosis Foundation (Anonymous 1993) defined osteoporosis as: “A systemic skeletal disease characterized by low bone mass and micro-architectural deterioration of bone tissue with a consequent increase in bone fragility and susceptibility to fracture.” This definition has persisted. In 1994, this definition was operationalized by the World Health Organization (WHO, 1994). Osteoporosis was defined as a BMD more than 2.5 standard deviations below the mean value of young health women while osteopenia was defined as 1.0 standard deviation below this norm. Patients with osteopenia and osteoporosis have an increase in the rate of fractures that doubles with each standard deviation in their BMD below normal (Treasure and Serpell 2001).
The true prevalence of athlete energy imbalance is unknown. Two studies compared female athletes in particular classes of sports to an age-matched population of elite female athletes in “thin build” sports. Thirty-one percent of the elite female athletes in these sports had eating disorders, as compared to 5.5% of the control population (Byrne and McLean 2002). Twenty-five percent of female elite athletes in endurance sports, aesthetic sports, and weight-class sports had clinical eating disorders as compared to 9% of a control population of women. The percentage of eating disorders was even more pronounced in collegiate gymnasts with whom the prevalence of eating disorders can be as great as 62% (Rosen and Hough 1988). Menarche is often delayed in female athletes. Secondary amenorrhea has a prevalence of 2% to 5% in the general population but has a reported prevalence of up to 65% in long-distance runners (Dusik 2001). Female athletes who participated in “lean sports” had a higher rate of menstrual dysfunction (24.8%) than those that participated in so-called non-lean sports (13.1%).
In general, exercise increases bone mineral density. AEI reverses this positive effect of exercise because of relatively inadequate caloric intake and nutritional deficiencies. Repetitive, sub-threshold stress on bones that are abnormally weak because of demineralization and that are not allowed adequate healing and remodeling time increases fracture risk. Stress fractures account for 20% of all injuries in sports medicine clinics (Fredericson et al. 2006) (Figure 8.3).
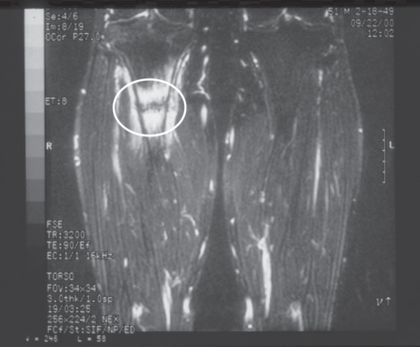
Area of increased metabolic activity and fracture line is highlighted (Raukar)
Stress fractures in athletes are seen most frequently in the tibia, femoral neck, metatarsals, and pubic rami and are four to ten times more common in women than in men. Fatigue or stress fractures are typically seen in women with low bone mass who have recently changed (usually increased) their training regimen. Women, especially runners, who sustain stress fractures of their tibia have been found to have lower extremity muscles that fatigue more quickly than those without fractures. Muscle fatigue results in additional stress being placed on the bone. The hip adduction and hindfoot eversion, seen more commonly in female runners, increase the risk of fatigue fractures, especially of the tibia.
The female athlete who presents to the ED with a stress fracture should be referred to an orthopedist, not only for management of her stress fracture but also for an investigation of her overall bone health.
Patients with a history and physical examination findings consistent with stress fractures should be evaluated with plain radiographs. However, these radiographs may be misleading, as no gross fracture may be noted; in more advanced phases of stress fracture, periosteal reaction will eventually be seen. If there is significant concern, and plain radiographs are unremarkable, the bone can be further evaluated with magnetic resonance imaging to demonstrate the fracture.
The athlete presents with injury, pain, disability, and decreased performance. Stress fractures in female athletes are generally an indicator of athlete energy imbalance. The clinician should initiate a frank discussion with the patient in the acute care setting at the time of injury, as this interaction may provide a teachable moment. These patients should immediately limit their weight bearing and follow-up with an orthopedist as soon as possible. The urgency of follow-up is especially important for athletes with suspected stress fractures of the femoral neck which, if not treated properly, can progress to become displaced fractures requiring extensive surgical intervention with concomitant severe pain, disability, and loss of function. Identification and treatment of patients with athlete energy imbalance require a high index of suspicion, an awareness of the presentation and diagnostic approach, appropriate acute management of the fracture, and focused referral to initiate a multidisciplinary intervention addressing the underlying root causes and setting the athlete on a course to improve his or her bone health. These athletes are at high risk for developing fragility fractures at an early age. Early diagnosis, treatment, and referral are imperative to assure their long-term bone health and physical well-being.
Women are more prone to stress (fatigue) fractures
All women with stress fractures should be asked about their menses, dietary restrictions, and exercise/training regimen
Stress fractures are not always apparent on plain radiographs. If an athlete presents for acute care having increased her training regimen and subsequently developed bony point tenderness, even if radiographs are negative, she should be treated as a stress fracture and should not return to training or play until further evaluation. Evaluation should be urgent for suspected stress fractures of the femoral neck, which usually require prophylactic surgical stabilization.
If a stress fracture is suspected or diagnosed in the ED, the patient will require follow up with their primary care provider, an orthopedist, and a gynecologist if the athlete is female. Patients should limit weight bearing until orthopedic evaluation.
The patient should be encourage to keep a food log and this should be shared with a nutritionist or their primary care provider.
Clinical Questions
How would you approach the work up in this patient?
What specifically do you have to consider in a man with an osteoporotic fracture?
What are the gender-specific elements in management and disposition that you should consider?
Are there specific referrals that should be made and to whom?
For those patients who are discharged with an osteoporotic fracture, can interventions be started in the ED that will decrease their future fracture risk?
Low-Impact Fractures
Osteoporosis is defined as a generalized metabolic bone disease characterized by both decreased bone density and poor bone quality (NIH Consensus Statement 2000). Osteoporosis leads to an increase in the frequency of fractures of the hip, humerus, spine, and wrist. Osteoporosis is a global public health problem affecting more than 200 million people worldwide. In the United States, osteoporosis is considered a major health threat for almost 44 million Americans, almost 55% of the population older than age 50 – 10 million with osteoporosis and another 34 million with osteopenia or low bone mass. Once considered a disease only of women, research has demonstrated that men are also at significant risk of developing osteoporosis. Men currently represent approximately 20% to 40% of patients with osteoporosis (Roger et al. 2011). Men with osteoporosis tend to be older than osteoporotic women and are more likely to develop osteoporosis as a result of another health condition or disease; thus, these men have bleak survival outcomes.
Bone is dynamic: It is in a constant state of resorption and regeneration. Peak bone mass has accumulated in most people by the age of 30. After 30, bone resorption occurs at a faster rate than bone formation. The bony micro-architecture deteriorates, changing the protein structure and content of bone, reducing the overall bone mineral density (BMD) and bone strength resulting in an increased risk of low-impact fractures. Osteoporosis is caused by (a) inadequate peak bone mass formation during adolescence, (b) excessive bone resorption after menopause or as a result of a chronic health condition and the treatment for that condition (e.g., COPD treated with chronic prednisone), or (c) a combination of the two. Low-impact fractures are most common in the spine, hip, proximal humerus, and distal radius. Low-impact fractures of these bones are indicators of clinical osteoporosis. Acute care providers must recognize the acute injuries that signify a presentation of osteoporosis and must be prepared to intervene in these patients as they have a markedly elevated risk for future fractures.
Nearly 2 million osteoporosis-related fractures occur each year in the United States. According to the National Osteoporosis Foundation, by the year 2025 more than 3 million Americans will suffer osteoporosis-related fractures. In the United States, the rates of hip and wrist fragility fractures are equal with an annual incidence of 300,000 each. The lifetime risk for an osteoporotic fracture of any bone requiring clinical attention is equal to the risk of cardiovascular disease, at about 40% (Kanis 2002). In women, the risk of hip fracture is more than the collective risk of uterine, ovarian, and breast cancer; in men, the incidence of an osteoporotic fracture is equal to the risk of sustaining a myocardial infarction and exceeds the risk of lung and prostate carcinoma combined (Binkley 2009). Osteoporotic fractures cost $19 billion annually. Between 1995 and 2009, the rate of hospitalization for osteoporosis-related injury and illness increased by 55%; 67% of these patients presented to EDs. Ninety percent were at least 65 years old, and 89% were women, who sustained these injuries at a rate six times greater than men (Russo 2009). In 2006 in the United States, hospitalization for injuries sustained as a result of osteoporosis exceeded $2.4 billion. Hip fractures were the most expensive osteoporotic injury and required the longest hospital stay. Although the majority of osteoporotic fractures occur in women, men have higher rates of fracture-related mortality. Outcomes after osteoporotic hip fractures requiring surgical repair are worse for men (Abrahamsen et al. 2009).
In patients with osteoporosis, fractures of the femoral neck, proximal humerus, and distal radius occur as the result of falls from standing. Even minimal trauma such as sneezing, rolling over in bed, bending over to perform activities of daily living, or falling out of a chair cause osteoporotic vertebral compression fractures. About 700,000 vertebral fractures are diagnosed annually in the United States. It is important to remember that most of these are incidental findings seen on X-rays obtained for other reasons. Elders in the United States are staying more active as they age and are sustaining more significant trauma. The acute care practitioner must remember that low bone mass can lead to more significant fractures than might have been anticipated from the mechanism of injury. Conversely, elders, especially women, with fractures from minimal trauma are likely to have osteoporosis.
Osteoporosis is diagnosed by measuring bone mineral density using dual-energy X-ray absorpitometry (DEXA) or quantitative CT (qCT) of the spine, hip, and/or forearm. The World Health Organization (WHO) defines osteoporosis as a bone mineral density that is 2.5 standard deviations or more below the mean peak bone mass, which is the bone mass of an average, young, healthy adult. Reference ranges for DEXA scans are sex based. The National Osteoporosis Foundation recommends BMD testing for all women age 65 and older and all men age 70 and older. Patients with significant risk factors should have their first DEXA scan at age 50. Risk factors (summarized in Table 8.1) include low body weight, history of prior fracture, family history of osteoporosis, smoking, excessive alcohol intake, and long-term use of certain medications, such as corticosteroids. However, a clinical diagnosis can be made in individuals who sustain a low-trauma or fragility fracture, such as a fall from standing height.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







