Chapter 6 Forensics
Basics of Forensics
Forensics pertains to the law and more specifically to the scientific analysis of evidence. While the roots of forensics date back to ancient Greece, it has evolved into a specialized field.1 Types of evidence include any object or asset belonging to a patient, any foreign material removed from the clothing or body of a patient, and any organ or tissue removed from a patient that is used for information before a court to prove or disprove a fact. Evidence can establish the facts, connect a person or persons to a crime or potential crime, or link a person’s action to the outcome of an event. Evidence can be touched or seen and is perceptible by the senses.2 Dr. Edmond Locard, a French scientist, developed the techniques that are considered to be the cornerstone of modern forensic sciences. During World War I, after evaluating stains on uniforms and clothing, Locard identified the location where French soldiers and prisoners died. Locard’s exchange principle was thus formed by applying the scientific method and logic to criminal investigations.3 Locard personally did not reference an exchange principle but did observe that “it is impossible for a criminal to act, especially considering the intensity of a crime, without leaving traces of this presence.”4 Based on these observations, the term “principle of exchange” first appeared in the publication Police and Crime-Detection in 1940.4
Evidence Classifications
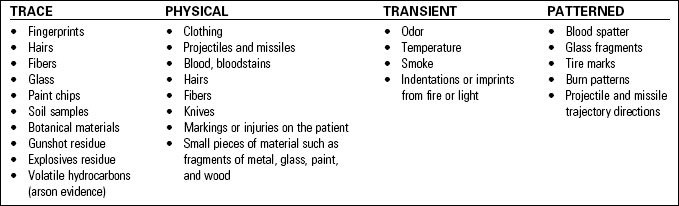
• Trace evidence is normally caused by objects or substances coming in contact with one another (no matter how slight the contact), resulting in a minute sample left on the contact surfaces.
• Physical evidence is any evidence that is a physical object. Facts or issues are proven based on demonstrable physical characteristics that can establish that a crime has been committed. Physical evidence can also provide a link between a crime and its victim or the perpetrator. It can conceivably include all or part of any object.
• Transient (conditional) evidence is any evidence that is temporary in nature.
• Patterned evidence occurs when there is physical contact between persons or objects.
Table 6-1 provides examples of the various types of evidence.
Uses of Forensic Evidence
• Medical-legal cases: A medical treatment situation with legal implications is defined as a medical-legal case. Medical-legal considerations are a significant part of the process of making many patient care decisions, including determining definitions and policies for the treatment of mentally incompetent people and minors, performing sterilization or therapeutic abortion, and providing care to terminally ill patients. Medical-legal considerations, decisions, definitions, and policies provide the framework for informed consent, professional liability, and many other aspects of current practice in the health care field.5 Suspicious deaths or crime-related injuries are viewed as medical-legal cases.
• Mass casualty incidents: An event where institutional resources are overwhelmed by the number or severity of victims or the resources consumed to care for these individuals. This determination will vary by facility.
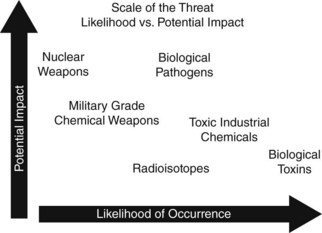
• Terrorism or weapons of mass destruction: As defined by the Federal Bureau of Investigation, weapons of mass destruction would include5:
Evidence Collection and Preservation
Collection and Management Principles
• Always wear gloves during the handling of all evidence collection. Change gloves often while the evidence is collected. Hospital personnel should wear the proper personal protective equipment (PPE).
• DO NOT cut through tears, rips, and holes, if possible.
• Check for blood, bloodstains, body fluids, gunshot residue (GSR), or trace elements. Minimize the handling of potential evidence as much as possible prior to packaging.
• Place all evidence collected in a paper bag or in a cardboard evidence box. Label the evidence box with the patient’s name, medical record number, date, and signature or initials of the collector (see Fig. 6-2).

Fig. 6-2 Firearm evidence box (A) and Gunshot Residue Kit (B) used by law enforcement personnel.
(Photos courtesy of J. Eckes.)
• Bag each item of clothing upon removal independently. Place each article in a separate paper bag to prevent cross-contamination (see Fig. 6-3).
• Secure all evidence retrieved and place in a designated location identified within the institution until retrieved by the appropriate investigating agency. A file cabinet with ventilation holes easily converts to a locked evidence storage locker. Access to this locker should be limited to those knowledgeable about chain of custody procedures.
• For questions concerning the collection, preservation, and documentation of evidence obtained from a deceased patient, refer to the investigating law enforcement agency, the medical examiner’s or coroner’s office, and institutional policy and procedure.
• Questions involving living patients should be directed to the appropriate investigating law enforcement agency.
• If the patient is pronounced dead on arrival to the emergency department (or shortly thereafter) and is not resuscitated:
• Notify the investigating law enforcement agency and the medical examiner’s or coroner’s office.
• Place paper bags over both of the patient’s hands. This will preserve any potential evidence that could be under the patient’s nail beds or on the hands.
• Wrap bullets in gauze to preserve trace evidence and place in a peel-pack, cup, or envelope. Do not touch bullets with metal instruments.
Wounds
• Observe the size, shape, and character of the wound. Create a diagram and describe all characteristics in detail.
• Avoid incising or cutting through the wound.
• Identify the presence or absence of any residue around gunshot wounds.
• Identify the number of wounds (holes) observed as well as location of the wounds. DO NOT identify or document the wound as an entrance or exit wound.
• Place a marker at the site of all wounds when taking radiographs to assist in the identification of location of projectiles or trajectory of projectiles. Place the marker to one side of the wound and not directly in or on the wound.
• Place paper bags over both hands, if there is consideration or knowledge of a weapon having been fired. If it is unknown at the time of admission whether a weapon has been fired, place bags over hands in preparation of crime scene investigator’s evaluation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree