Bronchial Blockers
• Bronchial blockers: May require longer to position & more intraop repositioning
• Univent tracheal tube (provides CPAP, but cannot ventilate while isolating the lung)
• Fogarty catheter (sm. size makes useful in pedi cases)
• No lumen for deflation, CPAP, or suction
• Wire-guided endobronchial blocker (WEB)
• Small lumen for deflation, CPAP, or suction
• Insertion loop: One-time use
Physiology of One-lung Ventilation
• One-lung ventilation in lateral position
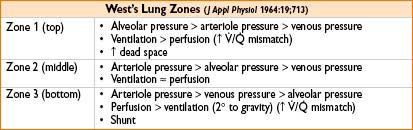
• Gravity causes ↑ blood flow to dependent (bottom) lung
• Pulmonary shunt ↓ as dependent lung is being oxygenated
• Lateral positioning with open chest
• ↑ blood flow to dependent lung
• ↓ effective compliance in dependent lung
• ↓ FRC
• Altered V./Q. (↑ perfusion, ↓ ventilation-dependent lung)
↓ oxygenation, ↓ CO2 elimination
• Hypoxic pulmonary vasoconstriction (HPV)
• Vasoconstriction of pulm arteries in presence of hypoxia → redirecting blood to alveoli with higher O2 tension
• Improves V./Q. matching → better gas exchange
• Inhibited by vasodilators (e.g., nitroprusside, nitroglycerine) alkalemia, hypocarbia, volatile anesthetics, PEEP
• Risk of hypoxemia in 1 lung ventilation
• V./Q. impairment
• ↓ HPV
• Worse typically at 10–30 min (absorption atelectasis—remaining alveolar O2 depleted)
Anesthesia with One Lung
• Invasive monitoring
• Arterial line—preferably dependent radial artery
• CVP (± for uncomplicated VATS/wedge/lobe in healthy pt)
• Pulmonary artery catheterization in selected pts
→ Monitor PA, Pcw for left heart filling pressures
→ PA catheter usually floats to the R side
→ Often not in best monitoring position (i.e., not in West zone 3)
Risks: Dysrhythmias, PA rupture
No proven improvement in outcomes with routine use
• Fiberscopic verification tube/blocker placement
• Tidal volume 6–8 mL/kg; plateau pressure <25 cm H2O; peak pressure <35 cm H2O
• Smaller TV ↑ risk atelectasis
• Larger TV ↑ shunting to nonventilated lung, ↑ risk barotraumas
• ↑ ventilation rate modestly (10%) to allow EtCO2 35 mm Hg
• Oxygen 100%
• Maximal PaO2
• Possible absorption atelectasis
• Limit time on 1-lung ventilation
• ↑ incidence of hypoxemia with:
• Right lung deflation
• Supine position
• Normal preop spirometry (no intrinsic PEEP)
• Management of hypoxemia
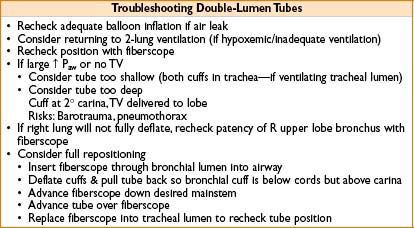
• Recheck proper tube position with fiberscope (see later)
• CPAP 5–10 cm H2O to nonventilated lung
<5 cm H2O generally ineffective
>10 cm H2O may reinflate nonventilated lung
• Consider PEEP to ventilated lung
May worsen hypoxemia via ↑ blood flow to nonventilated lung
• Return to 2-lung ventilation if serious irreversible hypoxemia
• For pneumonectomy—consider early operative ligation of pulmonary artery
ANESTHETIC TECHNIQUES—SPECIFIC SURGICAL PROCEDURES
Mediastinoscopy
• Preop evaluation
• Airway: Mass effects on trachea, great vessels
• History: CV prob, stroke, SVC syndrome, Lambert–Eaton syndrome
• Complications
• Hemorrhage, pneumothorax, chylothorax, recurrent laryngeal nerve injury, air embolization
• Anesthetic management
• General anesthesia most common
• Vascular access
→ Large bore IVs
→ Arterial line in left radial (right radial subject to innominate artery compression by mediastinoscope)
• Avoid nitrous oxide
• Muscle relaxation
→ Movement ↑ risk of surgical trauma
→ Cough/strain ↑ thoracic venous engorgement
→ Spontaneous ventilation may ↑ risk air embolism
• Postop—must check chest X-ray
Video-assisted Thoracic Surgery (VATS)
• Preop evaluation
• Discuss potential for open thoracotomy
• Complications
• Bleeding, lung injury (air leak)
• Anesthetic management
• General anesthesia most common
• Large-bore IV (consider CVP) access
• Arterial line
• Lung separation (see lung isolation section above)
• Consider slightly lower TV (e.g., 7–8 mL/kg) to ↓ mediastinal shift (improves operating conditions)
• ↑ Ventilation rate 10% (get CO2 absorption with insufflation)
• Muscle relaxation (see “Mediastinoscopy,” above)
• Consider neuraxial anesthetic if ↑ likelihood of conversion to open thoracotomy
• Postop—must check chest X-ray
Pneumonectomy
• Preop evaluation
• See “PFTs/Evaluation of Lung Resectability,” above
• ↑ risk of morbidity with right vs. left pneumonectomy, trauma, massive hemoptysis, history of cardiac disease, >10% preop weight loss
• Optimize treatment of existing pulmonary/cardiac disease
• Encourage smoking cessation
• Complications
• Bleeding, airway (stump) leak, cardiac dysrhythmias (consider role of β-blocker), cardiac herniation through pericardial defect, pulmonary edema, myocardial infarction, intracardiac shunt (can get ↑ R heart pressure, shunting via PFO)
• Anesthetic management
• Arterial catheter, central venous line
• Consider PA catheter
→ May not easily float to nonoperative side
→ Readings may not be reliable (tip not in West zone III)
→ May interfere with surgical procedure
• Airway
→ DLT to nonoperative side or bronchial blocker
→ Risk of intraop dislodgement with either technique
→ Risk of bronchial stump damage with manipulations
• Muscle relaxation
• Limit intraop fluids
• Postop analgesia options
→ Neuraxial opioid ± local anesthetic
→ Intercostal nerve blocks
→ Intrapleural catheter (risk of local anesthetic toxicity)
→ Systemic opioids (transition to IV PCA as tolerated)
Mediastinal Mass Considerations
• Preop eval
• ↑ Risk of tracheobroncheal obstruction with:
→ Orthopnea
→ Large airway compression on imaging
→ Flattened expiratory limb of flow-volume loop on PFTs
• Eval for evidence of superior vena cava syndrome
→ Upper extremity/facial edema (may indicate airway edema)
→ Dilated upper extremity veins
→ Headache, CNS changes
→ Consider preop steroid, diuretic, elevation of head of bed
• History syncope with position or Valsalva suggests
→ Cardiac/PA compression with hypotension
→ Critical tracheobronchial obstruction
→ Consider preop echo to eval for compression
• Consider preop biopsy/treatment to shrink mass (if severe airway/cardiovascular compression)
• Complications
• Acute tracheobronchial compression intraop
→ Highest risk is on transition to positive-pressure ventilation
• Acute cardiac/PA compression with severe hypotension
• Bleeding (esp with SVC syndrome due to venous engorgement)
• Anesthetic management
• Arterial access preinduction
• Large bore/central venous access
• Consider standby cardiopulmonary bypass (femoral) if airway or cardiovascular compression by mass
• Rigid bronchoscope available
• If SVC syndrome:
Consider lower extremity vascular access (more reliable drug/fluid delivery)
Avoid jugular or subclavian lines
• Consider spontaneously breathing fiberscopic exam/intubation if significant airway compression
• Initiate slow, controlled induction
Controlled transition from spontaneous ventilation to positive pressure
Short-duration relaxant desirable to facilitate tracheal intubation
If airway obstruction occurs:
• Attempt lateral positioning to move mass
• Resume spontaneous ventilation if possible
• Attempt to pass tracheal tube beyond obstruction carefully (risk hemorrhage)
• Attempt rigid bronchoscopy to open airway
• Consider cardiopulmonary bypass (femoral)
Smooth emergence & extubation
Cough/straining may worsen airway collapse
May ↑ bleeding (esp if SVC syndrome)
Esophagectomy
• Preop eval
• Nutritional status (↓ serum albumin, total protein)
• Dysphagia (reflux, risk of chronic aspiration)
• Prior chemo/radiation therapy
• Risk for cardiac dysrhythmias, esp supraventricular (consider prophylactic digoxin/β-blocker)
• Consider epidural placement
• Complications
• Gastroesophageal reflux, esophageal leak, respiratory failure, hypotension, cardiac dysrhythmias
• Anesthetic management
• Arterial line, consider central venous line
• Lung isolation for thoracotomy approaches
• Avoid nitrous oxide (expands bowel gas, need high FiO2 with 1-LV)
• Limit fluids
• ↑ Fluids associated with ↑ incidence pulmonary complications
• Avoid vasopressors
• Intraop use or hypotension associated with ↑ incidence GI anastomotic leak
• Consider ↓ drug dosages if pt has ↓ serum albumin
• Consider cricoid pressure at induction
→ May ↓ lower esophageal sphincter tone
→ May impede use intubation LMA
• Monitor glucose closely (esp if on TPN)
• Communicate with surgeon regarding esophageal manipulations (e.g., NG tube, esophageal bougie)
• Intraop hypotension: May be from hypovolemia, surgical compression of heart or great vessels, bleeding
• If postop mechanical ventilation planned
→ Change to standard endotracheal tube at completion of surgery
< div class='tao-gold-member'>









