Intracranial Pressure (ICP)
ICP = cranial (closed space) pressure on brain, CSF, & blood components
• Brain components: Brain mass/cells (80%); blood (10%); CSF (10%)
• Normal range: 0–10 mm Hg; CSF: 150 mL normal volume; 450 mL/d
• Increased ICP can lead to herniation & severe neurologic sequelae
• Acute ↑—shunting of CSF to spinal canal; ventricular compression
• Further ↑—compress brain tissue, mass effect, neuro deterioration
• Severe ↑—Cushing’s triad (↑↑ BP + ↓↓ HR + irreg. resp.)
Herniation—pupil asymmetry, ocular paresis, obtundation, nausea, decerebrate posturing, hemiplegia
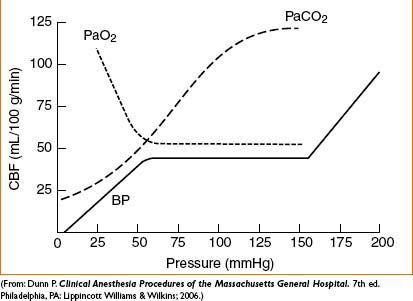
Figure 20-1. Relationship between cerebral blood flow in response to changes in PaCO2 and PaO2.
CRANIOTOMY
Anesthetic Management
General Features
• Mayfield pins & horseshoe headrest both commonly used
• Pinning is highly stimulating
• Anesthesiologist must anticipate (rather than react to) stimulation
• Best to place invasive arterial monitoring before pinning
• May inject pin sites with local anesthetic before pinning
• May need to deepen anesthesia/control BP in anticipation of pinning (may give IV, propofol, nicardipine, or opioid 30 sec prior)
• Airway may be rotated away from anesthesiologist
• Soft bite block should be placed immediately after induction between molars
• Tissue edema from tongue biting can form during surgery
• Can prevent tube kinking from biting or positioning
• Eye protection
• Secure taping of the closed eyelids
• Careful application of ophthalmic ointment recommended to avoid physical & chemical injury of the cornea
• Plan early for IV access (arms out or tucked)
• Decide early on need & site for intraop infusions
• Infuse via visible IV (if possible) to ↓ unnoticed infiltration
• Main times of stimulation: Intubation/pinning/incision/drilling/dural incision
• Avoid coughing/bucking/movement at any time
• Rapid blood loss is possible during any craniotomy
• Immediate postop assessment of neurologic function is crucial
• Inability to perform neuro exam → immediate postop CT imaging
• Avoid routine use of sedative medications (confound postop assessment)
• Opioids: Often used as part of a balanced-anesthesia technique
• Aggressive use of narcotics may lead to delayed emergence
• Give opioid dose early (i.e., induction, pinning, incision)
• Fentanyl = short-acting & titratable (5–10 mcg/kg total dose)
• Hydromorphone = longer-acting, give for postop analgesia
• Morphine = sedating, slow emergence; avoid in intracranial proc.
(Morphine metabolites may accumulate in renal failure)
• Remifentanil (0.1–0.5 mcg/kg/min) & sufentanil (0.1–0.2 mcg/kg/hr can be used as infusions
• Consider intravenous acetaminophen (1 g/6 hrs) for adjunctive analgesia
• Tight control of BP via invasive monitoring
• Fluid resuscitation
• Normal saline is usually the crystalloid solution of choice (can ↑↑ CI → metabolic acidosis)
• Avoid hypotonic or glucose containing fluids (can inc. brain swelling/injury)
• Colloid used as indicated by clinical context
• Periop antibiotics usually indicated
• Anticonvulsant therapy
• Indications for anticonvulsant & steroids vary with each pt
• May potentiate neuromuscular blockers (acute) or antagonize NMB (chronic)
• Anticonvulsant often used if contact with cortical tissue anticipated
• IV phenytoin (dilantin) loading dose: 18 mg/kg in 250 mL NSS at 25 mg/min)
Caution: Rapid bolus dosing of phenytoin may cause significant cardiac arrhythmia, hypotension, & cardiovascular collapse
• Fosphenytoin (a phenytoin prodrug with ↓ side effects) loading dose: 15–20 phenytoin equivalent mg/kg in 250 mL NSS @ 50–100 PE mg/min
• IV levetiracetam (keppra) loading dose: 1000 mg in 100 mL of normal saline over 15–30 min
Underlying renal failure, metabolic syndrome, & baseline meds should be considered prior to anticonvulsant admin
• IV dexamethasone (10 mg bolus, repeat 4 mg q6h) for edema when indicated
• Usually reserved for cases with intracranial lesion, elevated ICP, edema
Induction
• Controlled induction with hemodynamic stability
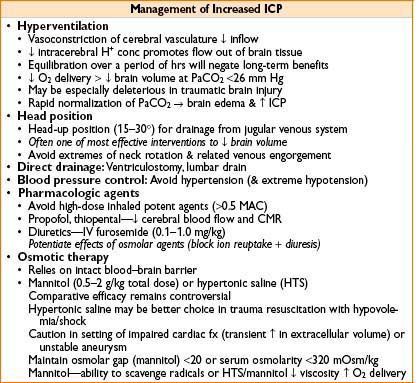
• Moderate hyperventilation in setting of ↑ ICP
• Combination of propofol 1–2 mg/kg, fentanyl 2–4 mcg/kg & nondepolarizing muscle relaxant is one approach
• Rapid, short-acting anti-HTN agents (esmolol, nicardipine) should be available
• Succinylcholine associated muscle fasciculation may result in transient ↑ ICP
• Coughing, bucking, or sympathetic surge during laryngoscopy with ↑ BP may cause sudden & untoward ↑ ICP (can use lidocaine 1 mg/kg to prevent)
• Physiologic manifestations of light anesthesia may be devastating in pts with intracranial aneurysm susceptible to rupture
Maintenance
• May use amnestic dose (0.5–1.0 MAC) of inhalational agent to ↓ brain volume
• Narcotic bolus as needed up to a predetermined estimate of total dose
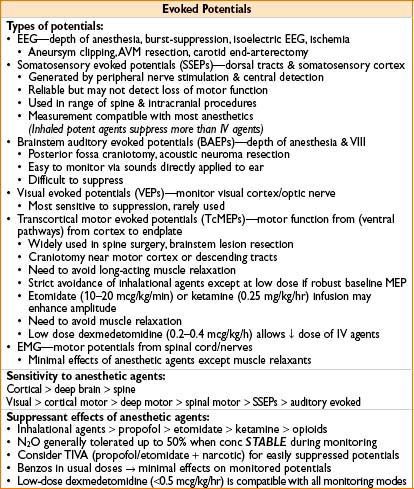
• Consider TIVA if monitoring evoked potentials or if need to ↓ brain volume
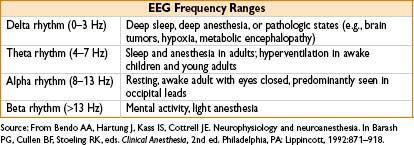
• Consider using a processed EEG monitor to guide TIVA dose
• Common strategy
• Propofol infusion for amnesia & brain relaxation
(Stop infusion once 1° resection complete to expedite emergence)
• Narcotic infusion for analgesia & immobility
(If muscle relaxation contraindicated because of monitoring)
• Provided an appropriate anesthetic depth has been reached, HTN should be liberally treated with labetatol or nicardipine to decrease likelihood for emergence hypertension
• Closely monitor urine output & resuscitate with normal saline
• Monitor glucose & treat glucose >160 mg/dL with insulin
• Hyperglycemia may predispose to or exacerbate neurologic injury
• If not contraindicated by monitoring requirements, maintain muscle relaxation to one twitch with bolus or infusion of nondepolarizing muscle relaxant
• Maintain MAP within 20% of baseline
• N2O may be used with several caveats:
• May complicate EEG or potential monitoring if level not constant
• May ↑ cerebral blood flow & contribute to brain swelling/↑ ICP
• May contribute to pneumocephalus (particularly in posterior fossa proc.) or pneumothorax expansion (esp. in trauma)
• May have deleterious effects on neuronal cells (under investigation)
Emergence
• BP control is critical
• HTN episodes at emergence & postop may cause ↑ bleeding or edema
• Treat with labetalol or nicardipine
• Prophylaxis for nausea/vomiting recommended (ondansetron)
• Avoid promethazine, droperidol, diphenhydramine (can be sedating)
• Emergence should begin after Mayfield pins have been removed
• Time should be allowed (5 min) for head wrapping before extubation
• Extubation: Reaches baseline mental status
• Small boluses of propofol (10–40 mg) or remifentanil (0.2–0.5 mcg/kg) can smooth emergence as can a dexmedetomidine infusion
• Continuous vital sign monitoring during transport
Special Features of Operations Involving the Posterior Fossa
• ↑ ICP commonly a concern (due to obstruction by a posterior fossa mass)
• Consider aggressive treatment of ICP prior to induction
• In severe cases, consider ventriculostomy under local anesthesia
• ↑ ICP may occur if head down during positioning/surgical prep
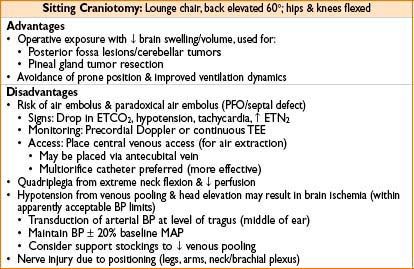
• Prone, head-up position—concern for air embolus
• Potential for postop, compressive pneumocephalus
• Kinking of ETT with neck flexion in pins (MUST place bite block)
• Postextubation macroglossia, tongue ischemia/injury
• Proximity to critical neurologic structures involving regulatory centers
• Brainstem/medulla/pons regulatory centers
• Bradycardia, apnea, rapid swings in BP may occur
• Possibility for new postop deficits
• Small operative window may lead to inc. brain swelling
• Jugular venous drainage/head position
Awake Craniotomy
• Used for resection of tumors (motor or speech cortex) & epileptic foci
• Team approach with emphasis on communication, patience, & experience
• Critical to set pt & surgeon expectations
• Awake with variable sedation versus “asleep → awake → asleep” with LMA/ETT
• Preference varies by center & experience
• Simplest method is to avoid airway instrumentation
• Only period of intense stimulation is opening/drilling/dural incision
• Patient comfort
• Positioning with padding/pillows for optimal comfort
• Vasoactive substances (nitroglycerin) may cause profound headache
• Warming blanket as needed for patient comfort
• Placement of Mayo stand over head to lift drapes off of the awake patient
• Preparation
• IV access, monitors, & arterial line prior to blocks
• Consider bilateral nasal trumpets (28–34 Fr) connected to O2 for airway management
• Topical anesthetic & vasoconstrictors to nares prior to placement
• Consider peripheral nerve blocks
• CNV1—supraorbital, supratrochlear n.
• CNV2—auriculotemporal, zygomaticotemporal n.
• Cervical branches—posterior auricular, greater & lesser occipital n.
• Remifentanil infusion for analgesia during block placement; PONV prophylaxis at start
• Choice of local: Use long-acting ropivicaine 0.375% with 1:200,000 epi
• Bupivicaine in large volume may have increased risk of cardiac toxicity
• Allow for additional local to be infiltrated by surgeons
• Metoprolol prior to block to blunt tachycardia
• Maintenance
• Deeper sedation only during drilling & opening of bone flap
• Minimize sedation just before dural incision
• Monitor CO2—hypercarbia can contribute to brain swelling
• Propofol/remifentanil with spontaneous ventilation
• Dexmedetomidine infusion is a useful adjunct
• Minimal resp. depression, can cause hypotension/bradycardia
• Treat with glycopyrrolate (0.2 mg) if bradycardia is clinically significant
• Load 1 mcg/kg over 15 min & infuse 0.3–1 mcg/kg/hr
• Neuromonitoring
Map functional cortex—usually speech area
Requires continuous patient feedback, communication, contact
< div class='tao-gold-member'>









