CSF Leak Repair
Often performed via endoscopic sinus approach for spontaneous leak with rhinorrhea
• Usually requires intrathecal injection of fluorescein (aids in localization under FESS)
• May place lumbar drain for 48- to 72-hr postop CSF drainage
• CSF opening pressure may be of prognostic utility
• Surgeon may request periop meningococcal meningitis prophylaxis (e.g., ceftriaxone)
Microdirect/Suspension Laryngoscopy
• Performed by otolaryngologist for a range of indications
• Employs specialized laryngoscopes for exposure of anatomy/pathology
• May use robot-assisted techniques & laser devices
• Procedure is highly stimulating for relatively brief periods
• Pts often have difficult airways & significant comorbidities
Indications
• Tumors of larynx, oral cavity, pharynx, hypopharynx
• Biopsy, laser ablation, robot-assisted micro-resection
• Vocal cord surgery
• Resection of vocal cord polyp
• Vocal cord injection for cord paralysis
• Insertion of mechanical larynx (artificial voice box)
• Tracheal stenosis—dilation/ablation of lesions
• Laser ablation/direct chemotherapy of papilloma
Special Considerations
• Preop discussion with surgeon regarding airway management
• Potentially difficult airway
• Prior surgery with scarring or postradiation changes (immobile larynx)
• Supraglottic/laryngeal masses or tracheal abnormalities
• Friable tissue → bleeding
• Positive-pressure mask ventilation may be challenging/impossible
• Airway = operative field & bed = rotated away
• Anesthetic gases may leak to environment/surgeon (open system)
• Intermittent apnea may be required for surgical access
• ETT may distort surgical anatomy & impede surgical access
• Laser ablation may be used (requires ↓ FiO2)
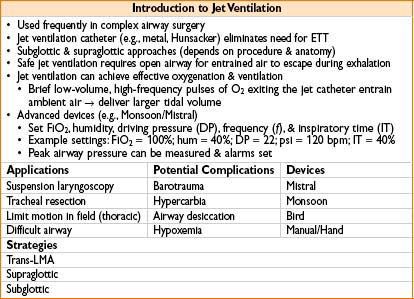
• Use jet ventilation, apneic technique or laser tube
• Fill laser tube balloons with methylene blue saline
• Use airway fire protocol
• Surgeon may desire spontaneous ventilation (assess vocal cord movement)
• Intense but fleeting/intermittent stimulus
• Requires constant communication between surgeon & anesthesiologist
Anesthetic Management
• GA usually indicated (owing to intense procedure stimulus)
• Sedation & spontaneous ventilation in selected cases (with cooperative pts)
• Requires anxiolysis & extensive topicalization with local anesthetic
• Anesthesiologist often induces GA & shares airway management with surgeon
• Surgeon should be present prior to induction of anesthesia
• Airway management includes a variety of options
• ETT (e.g., 5.0–6.0 mm ID) placed under laryngoscopy
• Catheter for subglottic jet ventilation placed under direct visualization (see text box, page 21–5) or jet via specialized laryngoscope
• Intermittent apnea with mask ventilation
• Airway device (if used) may be periodically removed for surgical access
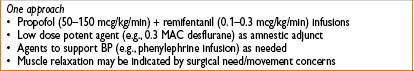
• TIVA technique preferable to inhaled agent
• ↓ OR contamination with inhalation gas
• More consistent depth of anesthesia
• Propofol & titratable, short-acting narcotic often used
• Muscle relaxation must be individualized for each case
• Consider airway management, operating conditions, need for spontaneous ventilation
• Inhalational induction may be considered
Medialization Thyroplasty (Vocal Cord Medialization)
• Procedure performed to treat vocal cord paralysis/bowing
• Partial resection of thyroid cartilage & prosthesis placement
Special Considerations
• Pt cooperation = important component
• Anesthesia best provided with sedation & local injection
• Pt able to phonate on command during surgery
• Vocal cord movement observed under nasopharyngeal laryngoscopy
• Surgical incision similar to partial thyroidectomy
• Dexmedetomidine infusion is an excellent option for cooperative sedation
PROCEDURES ON THE INNER EAR AND MASTOID

Stapedectomy
• Usually light sedation with local anesthesia (GA for selected pts)
• Sedation allows for intraop testing of hearing acuity
• Titrate meds (fentanyl, midazolam, propofol, dexmedetomidine) to allow pt cooperation
• Excessive sedation may lead to disinhibition & movement (precludes safe operating under the microscope)
• Some centers are investigating use of pt-controlled sedation
Myringotomy Tube Placement (Placement of Ear Tubes)
• Very short procedure, usually performed in pediatric pts under mask GA
• IV access not necessary; can use IM analgesics (ketorolac & fentanyl)
TONSILLECTOMY/PAROTIDECTOMY/UVULOPALATOPHARYNGOPLASTY
Tonsillectomy and Adenoidectomy
Indications
• Recurrent infection
• Obstructive sleep apnea due to hypertrophic tonsillar/adenoid tissue
Special Considerations
• Potential for difficult mask/airway—particularly in adults
• Consider oral RAE tube, secure in midline
• Procedure usually indicated owing to recurrent infection
• May be semiurgent even in the setting of active infection
• Short procedure necessitates careful use/titration of muscle relaxants
• Surgeon removal of mouth gag may result in extubation—monitor closely
• “Bring back” tonsil for bleeding common
• Aggressive preinduction volume resuscitation (esp pediatric patients)
• RSI or plan for potentially difficult airway (blood in airway & edema)
• Pediatric patients with sleep study evidence of recurrent hypoxemic episodes may demonstrate increased sensitivity to opiate therapy
• Exogenous opiate requirements to provide effective postop analgesia may be reduced by up to ½ normal per kilogram dosing
• Consider scheduled titration of opioids and extended cardiopulmonary monitoring (including possible overnight admission to monitored, inpatient unit) to increase effective surveillance of postop respiratory events
Parotidectomy
• GA with ETT; consider nasal RAE if deep lobe is to be resected
• Nasal tube precautions (oxymetazoline to nares, gentle dilation, tube sizing)
• Always a risk of significant bleeding with nasal tube placement (afrin & lubricant)
• Facial nerve monitoring; avoid additional muscle relaxation after induction
Uvulopalatopharyngoplasty (UVA)
• Performed for treatment of obstructive sleep apnea
• Airway management: Mask ventilation/intubation may be difficult
• Review sleep study results—apnea/hypopnea index for severity
• Consider RAMP positioning for obese patients
• Pts may require noninvasive ventilation in PACU/floor postop
TRACHEOSTOMY
Indications
• Ventilator-dependent resp failure
• Chronic aspiration
• Airway tumor/injury with airway compromise
• Acute stridor/bilateral vocal cord paralysis
Special Considerations
• If already intubated: Vent settings, O2 & PEEP required, intubation method & difficulty
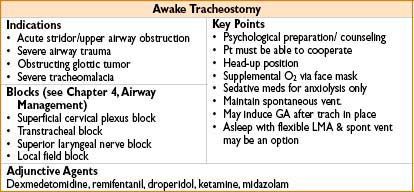
• If not intubated: Consider awake vs. asleep tracheostomy
• If in resp failure/ARDS: May require special ventilator settings
• Conventional OR ventilator limited (consider ICU vent)
• Pt may not tolerate vent, disconnect (loss of PEEP)
• May not tolerate lowered FiO2 during electrocautery
• Considerable bleeding is rare but possible (aberrant vasculature)
Anesthetic Management
• Awake tracheostomy (see box, page 21–5)
• GA: Inhalational or TIVA; muscle relaxation may optimize surgical conditions
• Potential for ETT balloon puncture upon tracheal incision
• Deflate ETT balloon prior to tracheal incision
• Consider advancing ETT (balloon) prior to tracheal incision
• Withdrawal to just above tracheotomy site under direct surgical visualization
• Do not fully extubate until tracheostomy is in place & secured
• If tracheostomy lost, ETT can be quickly readvanced distal to tracheotomy
• Lower FiO2 (<30%) if monopolar cautery to be used after tracheotomy
Management of Existing Tracheostomy
• Does tracheostomy have a balloon/cuff?
• Will positive-pressure vent be required? (Limited with uncuffed tracheostomy)
• Will unusual positioning be required?
• Is tracheostomy <7 d old?
Management of Mature Tracheostomy (>7 d)
• Suction existing cannula
• Denitrogenate with 100% O2 via tracheostomy
• Controlled inhaled induction with potent agent (e.g., sevoflurane) or IV induction
• Exchange tracheal tube with a lubricated, wire-reinforced ETT that has the same inner diameter or one size smaller than tracheostomy tube
• Advance tube such that black markings are positioned at stoma & check for bilateral breath sounds
• Replace tube with clean tracheostomy tube at case completion after resumption of spontaneous ventilation if uncuffed trach
Management of Fresh Tracheostomy
• Fresh tracheostomy (<7–10 d) requires interdisciplinary management
• Should generally not be removed outside OR (no tract)
• Fresh tracheostomy dislodgement = surgical emergency
• Call for surgical support & fiberoptic bronchoscope
• Put sterile gloves on & plug tracheostomy site with finger
• Do not attempt blind replacement of tracheostomy
• Risk of subcutaneous placement, bleeding, & trauma
• Attempt mask ventilation
• Place LMA if failed/difficult mask ventilation
• Attempt intubation across tracheostomy site by laryngoscopy
• Consider fiberoptic intubation if unsuccessful
• Advance ETT balloon past tracheotomy
• If intubation fails & ventilation is adequate, proceed to OR
• Tracheostomy replacement via trans-LMA fiberoptic or videolaryngoscopic guidance may be considered in stable clinical circumstances with experienced personnel
• If above efforts fail, surgical reexploration at bedside


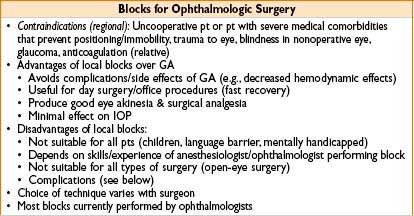
PROCEDURES IN OPHTHALMOLOGY
Special Considerations
• Extremes of age (pediatrics—strabismus repair) (geriatrics—cataract surgery)
• Many ophthalmologists perform regional blocks themselves
• Complications from movement may result in blindness
• Appropriate precautions (see above) for laser surgery
• Access to airway is limited during surgery
Special Medications in Ophthalmologic Population
• Echothiophate for glaucoma
• Acetylcholinesterase inhibitor → prolongs action of succinylcholine
• Systemic effects include bronchospasm, bradycardia, hypertension
• Sulfur hexafluoride gas for retinal detachment
• Pt may have intravitreal gas bubble up to 21 d postop
• Avoid N2O due to potential for catastrophic air expansion
• Consider avoidance of succinylcholine in selected circumstances
• Globe injury → increased intraocular pressure with fasciculation (succinylcholine is not absolutely contraindicated)
• Prolonged contracture of ocular musculature after dosing may interfere with forced duction test (FDT) in strabismus surgery
• Pilocarpine & carbachol
• Drugs that promote efflux of aqueous humor by producing miosis
• Parasympathomimetics (cholinergic agonist)
• Systemic effects = parasympathetic effects (bradycardia)
• Epinephrine
• Systemic effects may lead to tachycardia/angina
• Acetazolamide
• Carbonic anhydrase inhibitor
• Systemic effects include metabolic acidosis, hypokalemia, ↓ ICP
• Timolol
• β-blocker
• Systemic effects include bradycardia, hypotension, bronchospasm
• Oral glycerol side effects: Nausea, vomiting, hyperglycemia
• Mannitol side effects: Volume overload, renal failure
Cataract Surgery: Clear Corneal Phacoemulsification
• Pts often elderly with multiple comorbidities
• Procedures usually <1 hr
• Anesthetic goals
• Akinesia of the eye & eyelid; adequate analgesia & pt cooperation avoidance of oculocardiac reflex
• Sedation with regional block or topicalization = preferred method
• Local infiltration with sedation
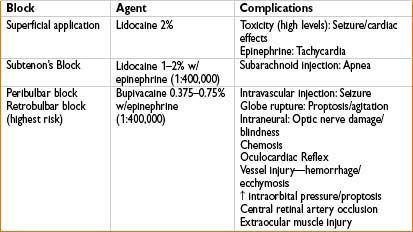
• Regional block with local infiltration & sedation (see table below)
• Provided by surgeon or anesthesiologist
• Brief deepening of anesthesia facilitates block placement
• Options include retrobulbar block; peribulbar block, subtenon’s block
• Block complications: Retrobulbar hemorrhage, globe perforation, optic nerve damage, brainstem anesthesia
• GA for selected pts (complex procedures/unable to cooperate or stay supine)
Strabismus Surgery
• Indication: Reposition muscles to treat ocular malalignment
• Surgery almost exclusively performed in pediatric pts
• ↑ Incidence of postop nausea & vomiting
• ↑ Risk of intraop oculocardiac reflex (see box below)
• Usually performed under GA with ETT
• Nondepolarizing muscle relaxation may aid diagnostic utility of FDT & surgical operating conditions
Other Procedures
• Repair of ruptured globe
• Frequently emergent procedure with aspiration risk concerns (full stomach, head & associated injuries)
• Commonly requires GA with ETT
• Consider LMA in select circumstances (pts often have full stomach)
• Emphasis on control of intraocular pressure (succinylcholine may ↑ IOP)
• Avoid coughing or bucking during induction & intubation
• Intraocular surgery: Enucleation, vitrectomy, corneal transplantation, glaucoma decompression, repair retinal detachments
• Control of eye movement & intraocular pressure critical
• GA preferred
• Intraocular epinephrine may be used to aid papillary dilatation
• Monitor for systemic effects
• Detachment repair injects intraocular air or sulfur hexafluoride gas
• Avoid N2O or discontinue well before injection
• Avoid N2O for subsequent surgery within 3 wks

Peribulbar Block (25–27 gauge, 25 mm needle)
• Safer (needle inserted outside of extraocular muscle cone), but slower onset
• Primary gaze position → 2 injections above & below globe
Inject ≈5 mL local into superonasal orbit & ≈5 mL inferotemporally between lateral 1⁄³ & medial ²⁄³ of lower orbital margin
Retrobulbar Block (25–27 gauge, 3 cm needle)
• Faster onset; must anesthetize conjunctiva before needle introduction
• Insert needle halfway between lateral canthus & lateral limbus in lower conjunctiva
• Direct needle straight back until the tip is beyond globe, → then direct needle toward apex of orbit to enter space behind globe between inferior & lateral rectus muscles
• Insert to depth of 25–35 cm; inject 4 mL local
Subtenon’s Block (25 gauge needle)
• Injection of local anesthetic directly into posterior aspect of subtenon’s space
• Insert needle to contact conjunctiva between eyeball & semilunaris fold (depth <1 mm)
Advance needle anteroposteriorly with globe directly slightly medially by needle until “click” is felt, at a depth of 15–20 mm (episcleral location)
• Return globe to primary position; aspirate → inject local
• Stop at sign of chemosis (conjunctival edema) & apply ocular compression
< div class='tao-gold-member'>









