ANESTHETIC CONSIDERATIONS IN ABDOMINAL SURGERY
Preoperative Evaluation
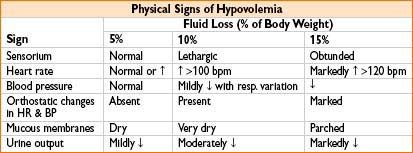
• Fluid status: Patients often hypovolemic
• Inadequate fluid intake (fasting, anorexia)
• Fluid loss (emesis, bowel preps, GI bleeding, fevers = insensible loss)
• Sequestration of fluid from intravascular space (3rd spacing)
Anesthetic Management
Technique
• Abdominal procedures usually require muscle relaxation
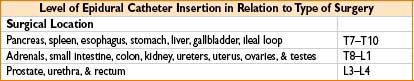
• Epidural analgesia may be beneficial (↓ anesthetic requirements, blunt surgical stress response, ↑ postop pain relief, ↓ postop atelectasis, ↑ postop mobility)
Fluid Management (See Chapter 9 on Fluids, Electrolytes, and Transfusion Therapy)
• General strategies
• Body wt-based formulas: Rough guidelines for fluid replacement
• Goal-directed strategies: Aimed at optimizing stroke volume, cardiac output, & tissue perfusion. Use mechanical ventilation or fluid bolus induced variations in pulse pressure (dPP), stroke volume (SV), or cardiac output (CO) to assess fluid responsiveness
• A more than 13% change in dPP, SV, or CO predicts fluid responsiveness
• Restrictive management: 4–8 mL/kg/hr—some evidence for ↓ postop morbidity compared with “liberal” strategies (10–15 mL/kg/hr)
• Replacement ratio: 3 mL crystalloid per 1 mL fluid loss 1 mL colloid per 1 mL fluid loss
• Only 1/3 of crystalloid remains intravascular, 2/3 goes into interstitium
• Colloids remain intravascular longer than crystalloids & exert oncotic pressure
• Blood products—should be given based on clinical eval of blood loss (surgical suction canister, sponges) & lab values (hematocrit)
Muscle Relaxation
• Usually required for intra-abdominal procedures & abdominal closure
• Secondary to intraop bowel edema & abdominal distention
• Inhalational agents may potentiate effects of muscle relaxants
• Neuraxial blockade with local anesthetics can provide good muscle relaxation
Use of Nitrous Oxide (N2O)
• N2O diffuses into bowel lumen faster than nitrogen can diffuse out
• Degree of bowel distention is a function of
• N2O conc, blood flow to the bowel, duration of admin
• Avoid N2O (relative contraindication) in bowel obstruction
• May have large initial volume of bowel gas and/or difficult surgical closure
• Causes an obligatory reduction in FiO2
• However, ↑ FiO2 may reduce incidence of surgical wound infection
• May ↑ pulmonary artery pressure (esp in pts with pulmonary HTN)
• Possible ↑ incidence of PONV (data is mixed)
Common Intraop Problems
• ↓ FRC, atelectasis, & hypoxemia because of
• Surgical retraction of abd viscera to improve exposure
• Insufflation of gas during laparoscopy
• Trendlenburg position
(Application of PEEP may reverse those effects)
• Hypothermia 2° to heat loss: Radiation > convection > conduction > evaporation
• Most heat loss occurs during 1st hr of anesthesia (1–1½°C)
(treat by ↑ OR temp, apply convective warming blankets, warm IV fluids)
• Hypotension, tachycardia, & facial flushing during bowel manipulation
• 2° to mediator release (prostaglandin F1-α, aprostanoid)
• Opioid-induced biliary tract spasm
• May interfere with interpretation of intraop cholangiograms
(Reversed by naloxone, nitroglycerin, & glucagon)
• Hiccups are episodic diaphragmatic spasms relieved by
↑ anesthetic depth, ↑ neuromuscular blockade, drainage of stomach to relieve gastric distention
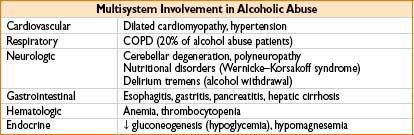
ALCOHOL ABUSE
Preop Evaluation
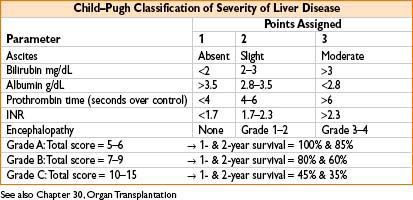
• Alcoholic cirrhosis characterized by AST/ALT ratio >2
Anesthetic Considerations
• Acute intoxication: ↓ anesthetic requirements (2° to EtOH depressant effects)
• Chronic intoxication: ↑ anesthetic requirements (2° to tolerance)
• Head & cervical spine injury must be considered in intoxicated pts
Postop Considerations
• Unrecognized alcohol abuse may present with delirium tremens
• Often occurs 72 hrs after last drink (postop day 3)
• Signs: Autonomic hyperactivity, tremors, hallucinations, seizures
• Treatment: Benzodiazepines
ANESTHETIC MANAGEMENT: LIVER SURGERY
General Considerations
• Liver resections often done for metastasis to liver or 1° hepatocellular carcinoma
• Hypoxemia → 2° hepatopulmonary shunting, atelectasis, ↓ FRC from ascites
• Prior portosystemic shunt ↑ surgical complexity & risk of surgical bleeding
Management of Portal Hypertension
• Pharmacologic: β-blockers
• Endoscopic: Sclerotherapy & esophageal banding for bleeding varices
• Transjugular intrahepatic portosystemic shunt (TIPS) have replaced surgical shunts, done percutaneously under fluoroscopy
• Surgery: ↑ risk of encephalopathy, no evidence of better outcome
Monitoring
• A-line & CVP
Anesthetic Technique
• General endotracheal anesthesia
• Thoracic epidural for postop pain control (provided no coagulopathy)
• Aspiration precautions (nonparticulate antacids, rapid-sequence induction)
• Avoid N2O (risk of bowel expansion & potential ↑ pulm artery pressure)
• Avoid histamine releasing muscle relaxants (atracurium, mivacurium) to avoid further ↓ blood pressure
• Hyperdynamic circulation in pts with end-stage liver disease may require vasopressor therapy to ↑ systemic afterload
• Concomitant pulmonary HTN in pts with ESLD → avoid hypoxemia, hypercarbia, & metabolic acidosis (worsen pulmonary HTN)
• Careful NG tube placement (concern for coagulopathy + esophageal varices)
• Fluid replacement with isotonic fluids & colloids (pts have ↓ intravascular oncotic pressure)
• Prolonged hepatic “inflow” occlusion (Pringle maneuver: Occlusion of portal vein & hepatic artery) → may lead to coagulopathy & metabolic acidosis
Postop Care
• Bleeding: Surgical vs. coagulopathy
• Small for size syndrome in extensive hepatic resections (remaining liver unable to support metabolic functions → ↑ lactate, ↑ liver enzymes, worsening metabolic acidosis)
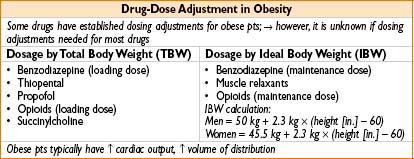
ANESTHETIC MANAGEMENT: BARIATRIC SURGERY
General Considerations
• Body mass index (BMI) = body weight in kg/(height in meters)2
• Overweight = BMI > 25; Obesity = BMI > 30; Morbid obesity = BMI > 35
Types of Bariatric Surgery
• Vertical band gastroplasty
• Creation of small pouch → restricts volume of food that can be ingested
• Open Roux-en-Y gastric bypass
• Formation of small gastric pouch anastomosed to proximal jejunum
• Dumping synd.: Ingestion of energy-dense-food → nausea, diarrhea abd pain
• Pts at risk for Fe and B12 deficiency
• Laparoscopic Roux-en-Y gastric bypass
• Smaller incision, ↓ postop pulm complications/pain, earlier ambulation
Preanesthetic Considerations
• Obesity-associated comorbidities
• HTN, hyperlipidemia, obstructive sleep apnea (OSA), GERD, type II diabetes
• ↑ circulating blood volume, ↑ cardiac output → ↑ in O2 consumption
• ↓ lung compliance, ↑ ventilation/perfusion mismatch & ↓ FRC → hypoxemia
• Long-standing hypoxemia → pulmonary HTN, & rt-sided heart failure
Anesthetic Technique
• General endotracheal anesthesia
• Epidural analgesia for pts undergoing open Roux-en-Y bypass
• Reduces need for systemic opioids & oversedation in pts with OSA
Airway Management
• Specific considerations
• Predictors of difficult intubation: ↑ neck circumference (>42 cm) & Mallampati score III & IV
• Obesity = risk factor for difficult mask ventilation
• Rapid desaturation following induction 2° to ↓ FRC, ↑ O2 consumption, & ↑ incidence of airway obstruction
• Management strategies
• Preoxygenation for 3 min in a 25° head-up position
• Consider ramped position (horizontal alignment between auditory meatus & sternal notch) to improve laryngeal view
• Consider awake intubation if airway exam concerning
• Consider aspiration precautions (antacids + rapid-sequence induction)
• Consider use of insoluble gases (desflurane, sevoflurane)
• Consider short-acting narcotics & sedatives (↓ risk postop resp. depression)
Monitoring
• Indications for A-line: Hypoxemia, ↓ systolic fx, moderate & severely ↑ pulm artery press, & inability to measure bp noninvasively
• ECG: May show RBBB 2° to pulmonary HTN
• DVT risk: ↓ risk with pneumatic compression devices and/or SC heparin
• Equip: OR table must accommodate pt weight, capacities vary widely
Postop Complications
• ↑ Incidence of atelectasis & hypoxemia (consider semirecumbent position, CPAP or BIPAP)
• ↑ Postop. hypercarbia esp in pts with baseline retention and periop opioid use → CO2 narcosis → hypercapnic resp. failure
• Negative-pressure pulmonary edema 2° to inspiration against closed glottis
• Accidental stapling of NG tube to pt stomach (prevent by keeping close communication with surgical team)
• DVT prophylaxis & early ambulation ↓ risk of thromboembolism
ANESTHESTIC MANAGEMENT: LAPAROSCOPIC SURGERY
General Considerations
• Advantages include smaller incision, ↓ surgical trauma, ↓ postop pain, ↓ pulmonary dysfx, ↓ postop ileus, faster recovery, & ↓ hospital stay
• 3 ports typically inserted into abdomen: (subumbilical port used for CO2 insufflation to 12–15 mm Hg)
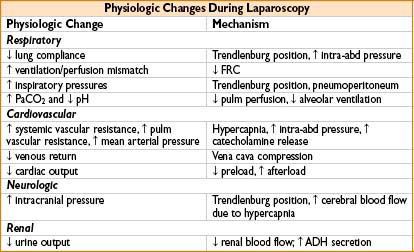
Anesthetic Technique: Laparoscopic Surgery
• General anesthesia with endotracheal intubation and controlled ventilation
• Muscle relaxation to avoid further increase in intrathoracic pressure
• Rapid-sequence induction for antireflux procedures and patients with full stomach
• Persistent ↑ ETCO2 despite adequate minute volume may signal subcutaneous emphysema
• Attenuation of hemodynamic changes to peritoneal insufflation:
• Bradycardia → glycopyrrolate or atropine
• Decreased CO & hypertension → use volume loading and/or vasopressor
• Hypertension → use vasodilators
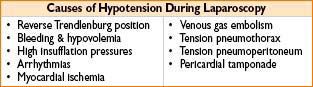
Monitoring
• Large-bore peripheral IV access (limited access to tucked arms during case)
• Orogastric tube to aspirate gas from stomach prior to trocar placement
• Acute ↑ in peak airway pressure may signal:
• Endobronchial migration of tube (esp. with bed change to Trendlenburg)
• Pneumothorax (usually accompanied by ↓ SpO2)
• Avoid ↑ peak airway pressure: Use pressure-control ventilation and ↓ exp time (e.g., I/E ratio 1:1.5)
• Minute volume usually must be ↑ by 20% to maintain normocarbia
• Bradycardia following CO2 insufflation likely vagally mediated
• May also be 2° to hypercarbia & respiratory acidosis
• Avoid ↑ in insufflation pressure that can compromise venous return (max 12–15 mm Hg)
Postop Care
• Shoulder pain (suprascapular nerve irritation)—treat with NSAIDs
• Unrecognized intra-abdominal visceral/vascular injury → progressive hypotension, ↑ abdominal girth, ↓ hematocrit
• ↑ incidence of PONV
• Extensive subcutaneous emphysema may require mechanical ventilation
LARGE INTESTINAL SURGERY
Indications
• Colon cancer, diverticulitis, ulcerative colitis, Crohn’s dz, ischemic colitis, reversal of colostomy
Preop Evaluation
• Preop fasting + bowel prep = large fluid deficit
• Bowel obstruction can ↑ risk for gastric aspiration during induction
• Thoracic epidural analgesia (T8–12) ↓ atelectasis, ↑ early ambulation (may contribute to hypotension in presence of hypovolemia)
Anesthetic Management: Large Intestinal Surgery
• Consider aspiration precautions if pt is obstructed
• Consider stress dose steroids if pt on preop steroids
• Fluid replacement must account for evaporative losses of exposed viscera
• Mesenteric traction syndrome: Hypotension during bowel surgery from bowel-associated mediator release (vasoactive intestinal peptide)
→ Hypovolemia, surgical bleeding, sepsis 2° to peritoneal fecal spillage
Postop Complications
• Prokinetic agents (metoclopramide) can cause anastomotic dehiscence after colonic surgery
• Postop ileus caused by bowel manipulation, opioids, immobility, lack of enteral feeding, & bowel edema from fluid overload (epidural analgesia may ↓ incidence of ileus)
• Prolonged NG tube placement can lead to ischemic necrosis of nasal septum
SMALL INTESTINAL SURGERY
Indications
• Small bowel obstruction, neoplasms, intussusception, intestinal bleed, resection of carcinoid tumor, Crohn’s dz
Carcinoid Tumors/Carcinoid Syndrome
• Carcinoid tumors typically asymptomatic
→ May present with abd pain, diarrhea, & intermittent obstruction
• Metastatic carcinoid tumors (hepatic, pulm metastases) systemic symptoms
→ Carcinoid syndrome: Cutaneous flushing, bronchoconstriction, hypotension, diarrhea, & rt-sided valvular lesions
↑ 5-hydroxy-indole-acetic acid (>30 mg in 24-hr urine)
• Epidural analgesia may exacerbate intraop hypotension (consider use of dilute local anesthetics/narcotics + volume loading)
Monitoring
• Consider TEE for carcinoid (eval rt-sided heart lesions & guide fluid therapy)
Anesthetic Management
• Consider aspiration precautions/rapid-sequence induction for obstruction
• Carcinoid tumors
• Avoid agents that release histamine (thiopental, succinylcholine, atracurium, morphine)
• Octreotide (synthetic somatostatin) effective in relieving hypotension (subcutaneous dose 50–500 mcg—half-life of 2.5 hrs)
Postop Care
• 50% of carcinoid deaths result from cardiac involvement
• Similar considerations as in large intestine surgery
PANCREATIC SURGERY
Indications
• Pancreatic adenocarcinoma resection (Whipple: Pancreatojejunostomy with gastrojejunostomy & choledochojejunostomy)
• Treatment of complications of pancreatitis: Infected pancreatic necrosis, hemorrhagic pancreatitis, drainage of pancreatic pseudocyst
Monitoring
• Pancreatic surgery can be assoc with significant blood loss & fluid shifts (consider A-line, CVP depending on pt comorbidities)
Anesthetic Management
• Consider thoracic epidural analgesia (T6–T10) for postop pain control
• Often feeding tube tip will be adjusted by surgeon during procedure
• Pancreatic surgery for infection may be complicated by sepsis & ARDS
requires aggressive fluid resuscitation, vasopressor support (α-agonist, e.g., norepinephrine) & postop mechanical ventilation
Postop Care
• Significant pancreatic resection → insulin insufficiency & new-onset diabetes
SPLENIC SURGERY
Indications
• Splenic injury (blunt or penetrating trauma)
• Idiopathic thrombocytopenic purpura with splenic sequestration of platelets
Preop Preparation
• Periop platelet transfusion not warranted (unless platelet count is <50,000/μL or clinical evidence of coagulopathy)
Anesthetic Management
• Avoid drugs that interfere with platelet function (NSAIDs)
Postop Care
• Pts should receive pneumococcal, Haemophilus influenzae, & meningococcal vaccines
HEMORRHOIDECTOMY & DRAINAGE OF PERIRECTAL ABSCESS
Anesthetic Management
• Procedures usually short, often in lithotomy/prone position
• Usually general anesthesia (consider LMA for lithotomy cases)
• Spinals may be used (hypobaric soln for prone case, hyperbaric for lithotomy)
• Deep plane of anesthesia provides sphincter relaxation
Postop Care
• Postop pain can be severe → consider use of narcotics & NSAIDs
INGUINAL HERNIORRHAPHY
Anesthetic Management
• Commonly done as an outpatient procedure
• Spermatic cord traction may initiate a vagally mediated bradycardia
• MAC + local anesthesia most common approach
• Paravertebral block (T10–L2) increasingly used
• Spinal or general anesthesia may also be used
VENTRAL HERNIORRHAPHY
Preop Considerations
• Staged ventral hernia repair may ↓ incidence of postop respiratory failure (closure of large abd defects → pulm restriction)
Monitoring
• Obtain large-bore IV access to replace evaporative fluid losses in large cases
Anesthetic Management
• Consider epidural analgesia (T10–T12) or transversus abdominis plane block (bilateral for midline incisions, unilateral for one-sided hernias)
• Usually done with general endotracheal anesthesia + muscle relaxation
• Smooth emergence impt. (no coughing/bucking) to avoid disruption of repair
APPENDECTOMY
Preop Evaluation
• Consider preop IV hydration to replace fluid deficits (vomiting, poor intake)
Anesthetic Management
• Performed via open or laparoscopic approach
• Consider taking aspiration precautions (rapid-sequence induction)
Postop Care
• IV opioids usually sufficient for postop pain management
CHOLECYSTECTOMY
Anesthetic Management
• Performed via open or laparoscopic approach with general endotracheal anesthesia
• Opioid-induced biliary tract spasm
• May interfere with interpretation of intraop cholangiograms
• Can be reversed by naloxone, nitroglycerin, & glucagon
• Minimal blood loss unless abdominal vessel injury occurs
Postop Care
• Lap cholecystectomy → less postop pain & earlier discharge (usually same day)
< div class='tao-gold-member'>









