ANESTHESIA OUTSIDE THE OPERATING ROOM
General Considerations/Safety
• Thorough preoperative evaluation of every pt is essential
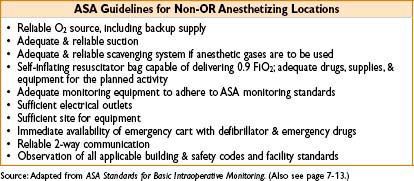
• All patients receiving any form of anesthesia must have ASA monitors during anesthesia care
• Transport equipment should be available (bag-valve-mask with O2 tank)
• Emergency drugs should be available & IV access assessed
• Postop care & standards are the same as for OR-based anesthesia
• Pay attention to possible allergies to contrast dye
CT/MRI/INTERVENTIONAL NEURORADIOLOGY
CT: General Considerations
• Pt should wear lead with thyroid shield at all times while in CT scanner
CT: Monitors
• Regular OR anesthesia monitors may be used
• Standard ASA monitors required if any anesthesia given
CT: Anesthetic Considerations
• Anesthetic options range from mild sedation to general anesthesia
• Patient factors to consider: Pt cooperation, claustrophobia, comorbidities, age, mental status, length of scan
• Ensure adequate length of IV lines, anesthesia circuit, monitoring wires
Special Procedures in the CT Suite
Stereotactic Brain Biopsy
• Metal frame placed to perform procedure (usu with local + benzodiazepine)
• Technique: MAC, titrate sedation carefully to avoid airway compromise if GA necessary, awake fiberoptic intubation may be the safest technique
Percutaneous Vertebroplasty
• Indication: Reverse vertebral collapse in osteoporotic patients
• Technique: Usually MAC (or GA if pt in excessive pain)
• Patient is in prone position → consider pelvic/chest support to avoid impinging on abdomen and interfering with ventilation
MRI: General Considerations
• Indications for anesthesia care: Children, mentally challenged, claustrophobic pts, pts with resp difficulty, hemodynamically unstable pts, chronic pain pts
• Distinct features of anesthesia in MRI:
• Powerful magnet
• Remove ferromagnetic equipment: Stethoscopes, credit cards, USB drives, pens, keys, IDs, beepers, cell phones
• Metals safe: Beryllium, nickel, stainless steel, tantalum, & titanium
• Difficulty accessing airway
• Carefully titrate sedatives & have monitors facing clinician at all times
MRI: Monitors
• Nonferrous monitoring equipment needed
• Nonmagnetic laryngoscopes for emergencies
• Ensure adequate length of IV lines, anesthesia circuit, monitoring wires
Interventional Neuroradiology
General Considerations
• Standard ASA monitors; if arterial line necessary, can be radial or through femoral sheath
• Femoral sheath a-lines → only MAP is useful
• Technique: GA if motionless state required; sedation if rapid neurologic testing essential or for most diagnostic scans
Deliberate Hypertension
• May be necessary to help radiology catheters flow to desired location
• Usually 20–40% above baseline; phenylephrine infusion may be useful
Deliberate Hypotension
• May be required in carotid endarterectomy/arteriovenous malformation (AVM) procedures
• Various approaches may be used (↑ anesthesia, labetalol, vasodilators—nitroprusside/nitroglycerin/hydralazine)
Embolization of Arteriovenous Malformation (AVM)
• Polyvinyl alcohol (PVA) injected into feeding vessels of AVM
• Approach: MAC (can continuously monitor neuro status) or GA
• Systemic heparinization may be required
• Complications: Hemorrhage 2° to anticoagulation (can reverse with protamine), hemorrhage 2° to thrombus (can ↑ BP by 20–40 mm Hg); ↑ ICP (treat with hyperventilation, head ↑, mannitol, furosemide)
Cerebral Aneurysms
• Uses balloons, coils, or liquid polymer solution to endovascularly treat the aneurysm
• Usually performed under general anesthesia, a-line should be placed
• Important to have OR available in case of rupture & urgent need for surgical repair
Central Intraarterial Thrombolysis
• Treatment of stroke if <6 hrs from onset of symptoms
• Usually performed under MAC (neurologic assessment is desirable)
Endoscopy & ERCP (Endoscopic Retrograde Cholangiopancreatography)
General Considerations
• Most upper and lower endoscopies are performed without an anesthesiologist
• Lateral position for lower endoscopy; lateral/supine for upper endoscopy
• Important to have access to airway at all times
Technique
• Anesthetic options range from mild sedation to general anesthesia
• For anesthesia sedation cases: Midazolam/fentanyl/propofol combination often used
• Patient factors to consider: Pt cooperation, comorbidities, age, mental status, length of procedure
• Upper endoscopy: Consider pharyngeal topical anesthesia (lidocaine, benzocaine) prior to endoscope insertion
• Postop pain: Relatively low, usually from air used for inflation
• ERCP: May be performed in supine, lateral, or prone position; pt can have significant pain during bile duct dilatation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








