CHAPTER 50
Fluoroscopy and Ultrasound-Guided Joint Injections
IMAGE-GUIDED PERIPHERAL JOINT INJECTION INDICATIONS
The most common clinical indication for an image-guided interventional procedure is pain in the targeted anatomic location, which has either failed other conservative treatments or as an adjunctive treatment. The primary advantage of image-guided interventional procedures over blind injections includes needle placement confirmation and the ability to view the targeted area and relevant anatomy.
Corticosteroid injections are frequently used as conservative treatments in the management of various conditions, including osteoarthritis, tendonitis, bursitis, and impingement conditions. Injectate mixtures typically comprise a local anesthetic and a corticosteroid (triamcinolone or methylprednisolone). In addition, patients at higher risk for developing nonsteroidal anti-inflammatory drug (NSAID)–induced renal dysfunction or gastric and duodenal ulcers are candidates for intra-articular steroid injections to avoid the potential systemic effects that occur with oral anti-inflammatory medications. However, the detrimental effects of repeated steroid injections on soft tissue structures like articular cartilage and tendons have not yet been determined.
The advantages of ultrasound-guided percutaneous interventional procedures are as follows:
• Real-time assessment
• Guidance, and continuous needle visualization
• Lack of radiation exposure
• Technological portability
• Relatively low cost
• Improved accessibility
Fluoroscopic guidance also allows real-time needle visualization and the acquisition of imaging frames throughout the injection course. The visualization occurs at different C-arm angles. The primary disadvantage of fluoroscopy is radiation exposure to both the patient and physician.
BASIC CONCERNS AND CONTRAINDICATIONS
With therapeutic interventions, the benefits and risks of the procedure must be considered. Generally, peripheral joint corticosteroid injections are considered to be safe and conservative treatments. However, each patient’s risk factors for complications must be carefully considered prior to undergoing the procedure.
Some basic concerns for injection are following:
• Patients with primary or metastatic tumors in the target area
• Immunocompromised patients, who are at increased risk for infection
• Patients with thrombocytopenia
• Patients who may be unable to tolerate positioning
• Patients with allodynia or complex regional pain syndrome (CRPS), who will be unable to tolerate the procedure
• Patients on anticoagulant medications, who have been unable to stop these medications at an appropriate time interval
• For fluoroscopically guided procedures with the use of contrast dye, patients with allergies to contrast, shellfish, or iodine may be considered for interventional procedures without contrast
Contraindications for injection include:
• Infection, systemic or localized
• Coagulopathy
• Distorted or complicated anatomy
• Pregnancy for fluoroscopically guided procedures
• Patient refusal
GENERAL IMAGE-GUIDED INTERVENTIONAL PROCEDURE PREOPERATIVE CONSIDERATIONS
• Informed consent must be obtained and the risks and benefits of the procedure should be properly explained to the patient or consenting individual.
• The area must be examined for infection, skin lesions, and disease extent.
• Proper exposure of the targeted area is necessary. If clothing is restrictive, the patient should be requested to change into a gown.
• Ideally, the patient should be able to remain in the appropriate position throughout the procedure.
• Intravenous access is not necessary, but may be considered if the patient has a history of postprocedural vasovagal or hypotension responses.
• The patient must be asked whether he or she takes any anticoagulant medications (ie, aspirin, NSAIDs, etc) and, if applicable, when these medications were stopped prior to the procedure. If stopping the anticoagulant medications increases cardiac risks, it is highly recommended to obtain medical clearance from the patient’s cardiologist.
• The physician performing the procedure should have access to fluoroscopy or ultrasound.
• For fluoroscopically guided procedures, female patients in reproductive age should be asked about potential pregnancy and may require a urine pregnancy test.
• For fluoroscopically guided shoulder injections, the patient must be asked about prior allergic reactions to contrast, shellfish, and iodine.
BASIC ULTRASONOGRAPHY
Depending on the ultrasound probe and machine used, the shoulder, hip, and elbow regions may be examined with high-frequency (>10 MHz) linear array transducers. If the patient has a large body habitus, a mid-range frequency transducer (6-10 MHz) may need to be used to optimize image resolution and facilitate proper examination. An appropriate initial depth is 3 cm. Also, the frequency may be adjusted to visualize deeper structures (ie, glenoid labrum or labrum of the hip) or shallower ones (ie, acromioclavicular joint [AC] joint).
For ultrasound examination, tissues are described by their properties of echogenicity, echotexture, degree of anisotropy, compressibility, and blood flow on Doppler examination. Blood vessels are not susceptible to anisotropy, but exhibit compressibility and presence of blood flow on Doppler examination. In the shoulder, rotator cuff tendons display a high degree of anisotropy, which is particularly pronounced at the musculotendinous junction.
Tissue echogenicity is characterized as hyperechoic, hypoechoic, anechoic, or isoechoic. Due to lack of echoes, anechoic structures have a black appearance. Isoechogenic tissues have similar brightness in comparison with surrounding tissues. Hyperechoic structures (ie, normal tendons and ligaments) appear brighter than adjacent tissues. In contrast, hypoechoic structures appear darker than surrounding structures. Both muscles and nerves have mixed echogenicity patterns. Blood vessels either appear to be hypoechoic or anechoic.
Echotexture refers to the internal pattern of echoes and may vary based on the axis used to assess the structure. Both tendons and ligaments have “broom end” appearance when viewed in the transverse axis and a fibrillar pattern when viewed in the longitudinal axis. Nerves have a “honeycomb” appearance on transverse imaging and a fascicular pattern on longitudinal imaging. Muscles have a “starry night” appearance on a transverse axis and a pennate or “feather like” pattern on a longitudinal axis [7, 9].
BASIC POSTPROCEDURE FOLLOW-UP
The patient should be contacted via telephone on the day following the interventional procedure to determine pain relief achieved from the local anesthetic and if there were any complications. If the patient received a corticosteroid injection, the patient should be reminded that the anti-inflammatory property has a variable onset and may take up to 2 to 3 weeks to achieve symptomatic improvement. The primary postinjection concern is infection. Therefore, the patient should monitor the injection site for erythema, warmth, increased swelling or systemic features of an infection, including fever and chills. If the patient develops any complications, he or she should be advised to contact the injectionist for further guidance. For severe procedurally related adverse events, ie, fever >101°F, weakness, dyspnea, severe pain exacerbation, etc, the patient should be recommended to seek immediate emergency medical services and to notify the injectionist. All adverse reactions should be properly documented in the patient’s chart.
Clinical Pearls
• Image-guided interventional procedures are powerful diagnostic and therapeutic tools to aid in the diagnosis and management of various musculoskeletal disorders.
• The duration of benefit is variable, but steroid injections tend to produce substantial short-term relief of symptoms (eg, pain, swelling) with variable duration of relief (1-3 months).
• Body habitus may influence the image-guided approach used. In obese patients, fluoroscopy may be used to improve visualization of deeper anatomic structures that would be more difficult to visualize under ultrasound guidance. Conversely, in leaner patients, use of ultrasound guidance eliminates radiation exposure and usually most anatomic structures can be easily identified.
• Success of image-guided procedures is dependent on numerous factors, which include target localization through use of anatomic landmarks, patient cooperation, and the experience of the physician with image-guided interventions.
• Image-guided injections are well tolerated and have an excellent safety profile.
• These procedures can be repeated to manage recurrent symptoms, but patients should be cautioned that the detrimental effects of repeated steroid injections on soft tissue structures, ie, articular cartilage and tendons have not yet been determined.
THE GLENOHUMERAL (GH) JOINT OF THE SHOULDER
Indications
The glenohumeral joint of the shoulder is susceptible to premature arthritic development from various conditions that may damage the joint cartilage. Of these conditions, glenohumeral osteoarthritis is the most common form of arthritis that results in shoulder joint pain. The indications include:
• Glenohumeral osteoarthritis
• Rotator cuff arthropathy
• Post-traumatic osteoarthritis
• Acute and chronic adhesive capsulitis
• Rheumatoid arthritis
• Collagen vascular diseases
Oftentimes, patients present with generalized shoulder and upper arm pain and it may be difficult to localize the primary pain generator intra-articular glenohumeral joint injections are excellent diagnostic tools, which can aid in elucidating the primary pain generator. Therapeutically, intra-articular glenohumeral joint corticosteroid injections are relatively safe interventional procedures. These procedures may be performed if shoulder pain remains refractory to more conservative measures such as occupational therapy, pharmacologic intervention, and activity modification. Accuracy of blind glenohumeral joint injections has been found to be extremely variable, ranging from 25% to 95% accuracy. Image-guided intra-articular glenohumeral joint injection enables dynamic real-time visualization of the process, improves needle visualization, augments target accuracy, reduces damage to surrounding structures, ie, glenoid labrum, and decreases the risk of neurovascular injury, particularly to the brachial plexus.
Relevant Anatomy
The large and round head of the humerus articulates with the relatively flat glenoid fossa of the scapula to form the glenohumeral (GH) joint. The articular surface is covered with hyaline cartilage. Due to the relative incongruence of these surfaces, the glenohumeral joint is susceptible to degenerative changes and instability. The glenoid labrum is a fibrocarti-laginous layer, which envelops the rim of the glenoid fossa. With humeral dislocation and subluxation, the glenoid labrum is exposed and has an increased risk for trauma. The glenohumeral joint is encompassed by a lax capsule that permits a wide range of motion of the joint. However, this laxity compromises joint stability. The glenohumeral joint is lined by a synovial membrane, which attaches to the articular cartilage and forms synovial tendon sheaths and bursae. These synovial structures are particularly vulnerable to inflammation. The glenohumeral joint are innervated by the axillary and suprascapular nerves.
The glenohumeral, transverse humeral, and cora-cohumeral ligaments are the major ligaments of the shoulder joint. The rotator cuff muscles that surround the shoulder joint are the supraspinatus, infraspinatus, teres minor, and subscapularis muscles. The rotator cuff musculature and ligaments provide strength to the joint. However, due to misuse and overuse injuries, the rotator cuff muscles and their tendons are susceptible to trauma and inflammation.
The key to successfully locating the glenohumeral joint from a posterior approach is identifying the following structures (Figure 50-1):
• Humeral head, which is the primary bony landmark for locating the GH joint
• Posterior labrum
• Infraspinatus muscle and tendon
• Tendon sheath of the bicipital tendon
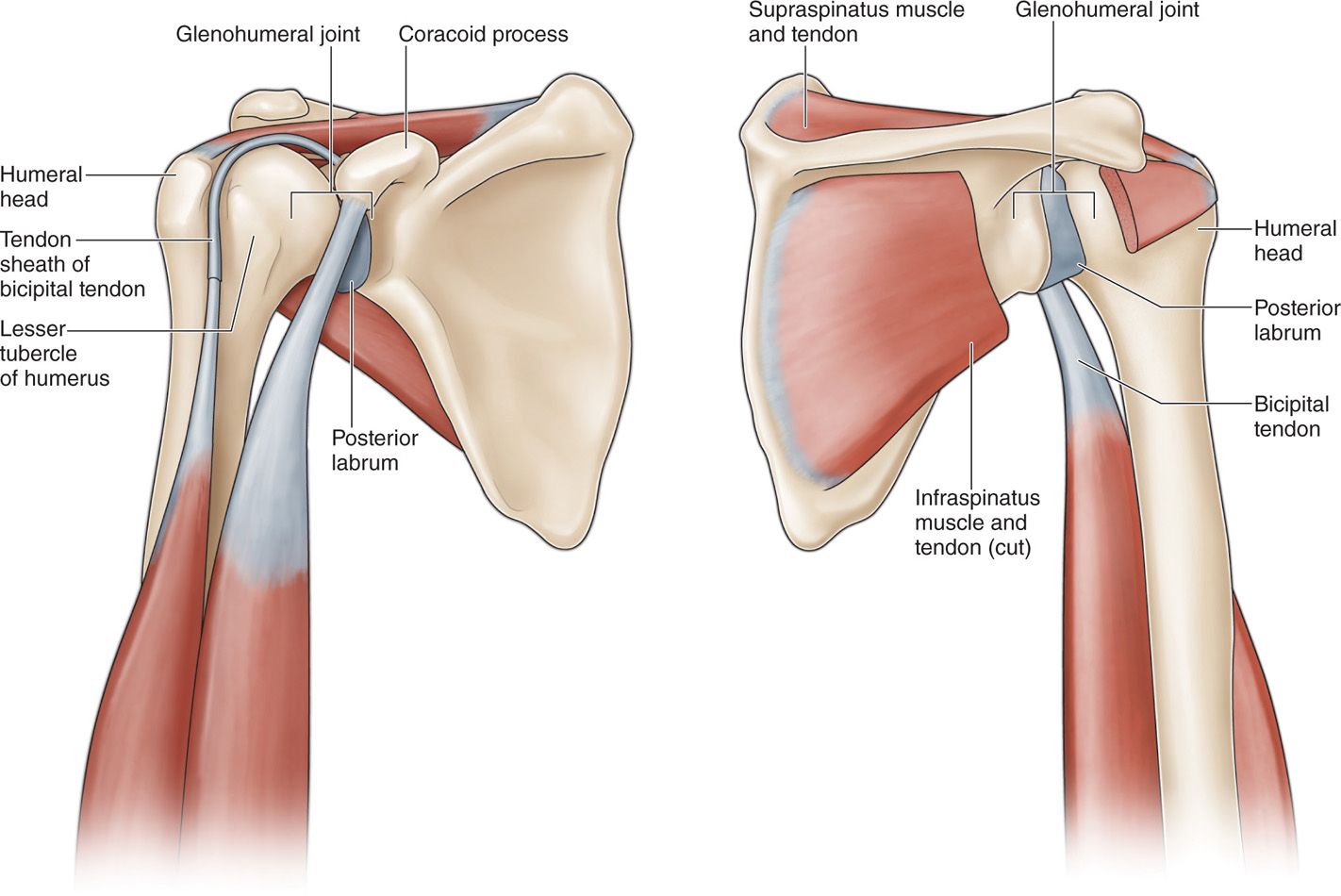
Figure 50-1. Illustrations of the posterior (left) and anterior (right) views of the right glenohumeral joint with relation to nearby anatomical structures.
From an anterior approach, the following structures should be identified (Figure 50-1):
• Lesser tubercle of the humerus
• Coracoid process
• Tendon sheath of the bicipital tendon
Other relevant anatomy that should be taken into consideration while performing these injections is:
• Brachial plexus, which is at increased risk for neurovascular injury from the anterior approach
• Calcifications of the rotator cuff muscle and bicipital tendons
Preoperative Considerations for GH Joint Injections
• For the ultrasound-guided approaches to the glenohumeral joint, the patient must be able to sit upright for the procedure duration. Preferably, the patient will be able to sit upright on a stool with a rotating seat, but without wheels.
• Alternatively, the patient may lie prone or supine on the examination table for, respectively, ultrasound-guided posterior and anterior approaches to the glenohumeral joint. However, assessment and procedural efficiency would likely be sacrificed.
• For most fluoroscopic interventional procedures, the patient should be able to maintain his or her position for the length of the procedure. For glenohumeral joint injections utilizing the posterior approach, the patient must be able to lie prone. For the anterior approach, the patient must be able to supine.
Selection of Needles, Medication, and Equipment
Needles
• 22-gauge 3.5-in spinal needle or, for ultrasound-guided injections, a 22-gauge echogenic needle, which will be connected to extension tubing
• 22-gauge 1.5-in needle to prepare the injectate medication
• 25-gauge 1.5-in needle for local anesthetic
• 6-cc syringe for local anesthetic
• 6-cc syringe for medications
• 3-cc syringe for fluoroscopically guided procedures with contrast
• 6-cc syringe for GH effusion aspiration (if applicable)
• Ultrasound machine or fluoroscope
• Extension connector tubing
Medications
• 1% lidocaine: 4 to 5 cc for local analgesia
• Injectate mixture
![]() 1% lidocaine or 0.25% bupivacaine or 0.5% bupivacaine: 2 to 4 cc
1% lidocaine or 0.25% bupivacaine or 0.5% bupivacaine: 2 to 4 cc
![]() Triamcinolone or methylprednisolone 40 to 80 mg (40 mg/mL)
Triamcinolone or methylprednisolone 40 to 80 mg (40 mg/mL)
![]() Please note that medication doses are dependent on factors including patient body habitus and condition severity
Please note that medication doses are dependent on factors including patient body habitus and condition severity
• Iohexol 180 (nonionic water-soluble contrast) for fluoroscopically guided procedures
• Total injectate volume: 5 to 8 cc
Ultrasound Views
• Ideally, a brief ultrasound-guided examination of the shoulder should be performed to assess the glenohumeral joint and periarticular structures. Performance of a routine ultrasound-guided examination of the targeted area ensures that errors of omission are evaded.
• Initially, the ultrasound probe is aligned in the long axis of the myotendinous junction of the infraspinatus muscle. The humeral head is the critical bony landmark to visualize. Due to the curved geometry of the rotator cuff tendons, anisotropy is usually present at this area.
• Transducer repositioning may be used to differentiate anisotropy from other pathological conditions. Great care should be taken to identify the other primary landmark, the glenoid labrum.
• The infraspinatus muscle and glenoid labrum are located superior to the glenohumeral joint. Whereas, the humeral head is located slightly inferolateral to the glenohumeral joint. Prior to needle entry site demarcation, the intended target should be viewed in 2 orthogonal planes, which are the long and short axes.
• Scan the area for the presence of a glenohumeral joint effusion to aspirate. The bicipital tendon sheath directly communicates with the glenohumeral joint and may have fluid due to either an extension of the glenohumeral joint effusion or a local tenosynovitis.
• Orient the ultrasound probe in the long axis view of the glenohumeral joint with the glenohumeral joint centered on the screen.
Ultrasound-Guided Injection Techniques
Primarily, the anterior and posterior approaches have been described for needle passage to gain access to the glenohumeral joint. Due to the increased risk of neurovascular injury to the brachial plexus with the anterior approach, we advocate the posterior approach to the glenohumeral joint. Contributing to this preference, other rationales include heightened patient anxiety with direct needle visualization and enhanced sensitivity of flexor surfaces compared with extensor surfaces.
Our Preferred US-Guided Technique: The Posterior Approach to the GH Joint
• The patient is seated on a stool and is positioned facing away from the injectionist.
• For the shoulder, a high-frequency (17-5 MHz) ultrasound transducer should be selected and ultrasound gel should be applied to the transducer.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






