Chapter 6 Fire Prevention in the Perioperative Setting
Perioperative Fires Can Occur Everywhere
Fire can start whenever heat, fuel, and oxygen converge together. During a surgical procedure, whether it is in a medical center, ambulatory surgery center, clinic, or physician’s office, all three of these components are usually present. This potentially places every surgical patient at risk for a surgical fire. A surgical fire is defined as a fire that is located on or in the patient (ECRI, 2006).
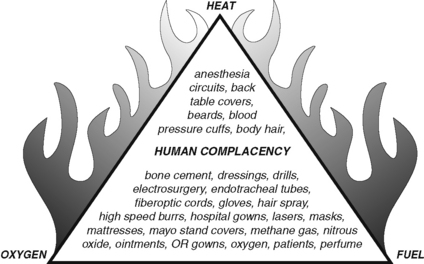
A fire triangle is frequently described when discussing elements necessary for the occurrence of a fire. A triangle is a geometric figure formed of three sides and three angles. The angles do not need to be the same degree and the sides do not need to be equal; they just all need to be present for the triangle to exist. The same can be said of surgical fires. All three elements of the fire triangle must be present for a surgical fire to occur. These three elements are heat, fuel, and oxygen (Figure 6-1). The elements do not need to be equal; they just need to be present and in close proximity. It is essential for the perioperative nurse to be familiar with each component as it relates to prevention and patient safety.
The surgical fire is not a new problem or one specific to modern medicine and anesthesia. Woodbridge (1939) stated, “Although statistically their importance is minute, they are of great emotional importance. The dramatic nature of the accident and of the death that may occur leads to publicity. The noise, the dramatic suddenness and the publicity all tend to produce a wave of fear and under the emotional tension of fear it is felt that something must be done, and done quickly.” Turner (2000) provides a review of the history of surgical fires and explosions, including events from as early as 1745 to the introduction and acceptance of the first nonflammable anesthetic agent, halothane, in 1956. Many of these historical fires were caused by the fire triangle that involved an ignition/heat source of static electricity, inspired oxygen (or room air) mixed with a flammable anesthetic agent, and fuel. Of note was a 1930 statement by the American Medical Association Council on Physical Therapy, “A certain carelessness regarding this matter has developed” (William, 1930). Later that year, the American Medical Association Committee on Anesthesia Accidents stated, “care does not now completely forestall this hazard” and discussed the importance of “weighing the potential advantages and disadvantages of each anesthetic technique” (Henderson, 1930).
On June 24, 2003, The Joint Commission (2003) issued a Sentinel Event Alert titled “Preventing Surgical Fires.” In the Sentinel Event Alert there is concern for underreporting of surgical fires. Estimates in 2003 from the U.S. Food and Drug Administration (FDA) and the ECRI Institute, a nonprofit health services research agency, suggested approximately 100 surgical fires. With the advent of mandatory state reporting of surgical fires, data are available that the ECRI Institute has used to better estimate occurrences of surgical fires in the United States. More than 50 million surgeries are now performed annually in the United States; the current estimate is that 550 to 650 surgical fires occur annually (ECRI, 2009).
At the time of the 2003 Joint Commission Sentinel Event Alert, the ECRI Institute’s analysis of case reports revealed that the most common ignition sources were electrosurgical equipment (68%) and lasers (13%); the most common fire locations were the airway (34%), head or face (28%), and elsewhere on or inside the patient (38%). An oxygen-enriched atmosphere was a contributing factor in 74% of all cases (ECRI, 2003). When these three elements of the triangle—an ignition source, an oxidizer, and a fuel source—come together in the wrong way at the wrong moment, a fire may occur (Box 6-1).
BOX 6-1 The Fire Triangle (and the Affiliated Surgical Team Member)
HEAT SOURCES (SURGEON OR ASSISTANT)
FUEL SOURCES (SCRUB PERSON, CIRCULATING REGISTERED NURSE, SURGICAL TECHNOLOGIST)
Flammable prepping agents including tinctures (chlorhexidine gluconate [Hibitane], thimerosal [Merthiolate]), iodophor [DuraPrep])
Ointments, petrolatum (petroleum jelly)
Tincture of benzoin (74% to 80% alcohol)
Patient’s hair (face, scalp, body)
Gastrointestinal tract gases (mostly methane)
Alcohol (also in suture packets)
Instrument and equipment drapes and covers
Adhesive tape (cloth, plastic, paper)
Collodion (mixture of pyroxylin, ether, and alcohol)
Disposable packaging materials (paper, plastic, cardboard)
OXYGEN SOURCES (ANESTHESIA PROVIDER)
PREVENTION
Oxygen-Enriched Atmosphere
When the patient receives oxygen and anesthetic gases through a face mask or nasal cannula, there is a potential for the creation of an oxygen-enriched atmosphere as the oxygen and nitrous oxide vents into the atmosphere and accumulates under the surgical drapes. This accumulation is of particular concern for surgeries performed in the head and neck region. The proximity of the surgical site to the oxygen-enriched atmosphere increases the potential for a spark from the electrosurgery unit (ESU), electrocautery unit (ECU), or laser to ignite the surrounding oxygen-enriched atmosphere. Seventy-four percent of reported surgical fires occur in an oxygen-enriched atmosphere (ECRI, 2003). Therefore a patient’s need for increased supplemental oxygen should always be communicated to the surgeon and the perioperative team members by the anesthesia provider or, in the case of procedure sedation, by the monitoring registered nurse (RN).
Heat Source
Keeping the active electrode of the ESU or ECU in a nonconductive holder when not in use is a simple step that can be taken to prevent surgical fires. Traditionally a “holster” is close to the scrub person, but a surgeon may prefer the active electrode to be close at hand. Health care facilities should consider the availability of an additional holster to encourage safe practice. Providing a second holster could end the debate over using the holster versus keeping the active electrode conveniently close at hand. The risk of accidental activation by placing instrumentation or supplies (or by simply leaning) on it is also mitigated by using the holster. Mark Bruley from the ECRI Institute recommends that if the active electrode is not in immediate use (defined as 5 to10 seconds), then it should be holstered or placed on the back table if it is a battery-operated device (Association of periOperative Registered Nurses [AORN], 2006).
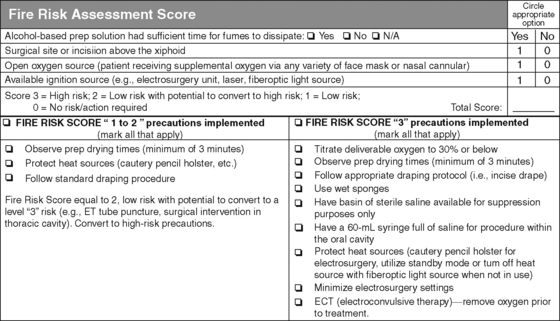
Several facilities are including fire risk assessment as part of the universal protocol process. The most frequently applied fire risk tool was developed by the Christiana Care Health System (Mathias, 2006). The patient is assigned a fire risk score of 1 to 3. A score of 1 is low risk, a score of 2 is low risk with the potential to convert to high risk, and a score of 3 is high risk (see Figure 6-2). After verifying the patient’s name and surgical site, marking the presence of instrumentation and implants needed, noting the location of the surgical site in proximity to the anesthesia gases, and the safe use of heat sources, the monitoring of supplies and fire risk assessment are discussed. This additional communication takes seconds but is a preventive strategy that should be encouraged.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree