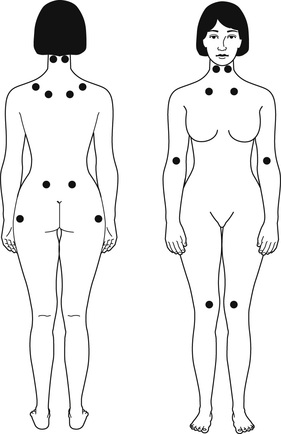
Lin A. Brown Fibromyalgia syndrome (FMS), a disorder usually included with rheumatologic conditions, is characterized by symptoms of widespread musculoskeletal pain, fatigue, nonrestorative sleep, depression, headaches, and gastrointestinal complaints (irritable bowel syndrome). FMS gained acceptance as a disorder in 1990 after the American College of Rheumatology developed classification criteria for the disorder. Fibromyalgia as defined in 1990 included more than 3 months of musculoskeletal pain present above and below the waist bilaterally, associated with pain on palpation of specific tender points (Fig. 175-1). No other source of pain is identified, although there may be so-called drivers of pain such as painful joints from rheumatoid arthritis that can be complicated by fibromyalgia. The pain is usually accompanied by profound fatigue and sleep disturbance (nonrestorative sleep). Most patients with chronic fatigue syndrome also meet diagnostic criteria for FMS. Myofascial pain syndrome is a more limited expression of the same condition (e.g., pain limited to the shoulder and neck, upper back). In 2010, the American College of Rheumatology put forth a new set of classification criteria that eliminated the tender point examination and replaced it with a report of pain surveyed in 19 areas as well as severity of symptoms associated with fibromyalgia (Box 175-1). FMS is diagnosed eight to nine times more often in women than in men of all age groups, with an onset in general at 40 to 50 years of age. FMS rarely begins after the age of 55 years. FMS affects approximately 5 million Americans, accounting for 2% of all primary care visits, 10% of all internal medicine referrals, and up to 20% of rheumatology referrals.1 Symptoms start gradually in adulthood or, rarely, in childhood and wax and wane in intensity.1 Although the cause of FMS is unclear, research has implicated central nervous system dysfunction and not muscle disease, autoimmune disease, or viral disease. Pain beginning in the periphery is processed in the spinal cord and transmitted to the brain. For unclear reasons, some pain becomes “louder” at the level of the spinal cord and brain, a condition called central sensitization. The brain responds with pain recognition at a lower threshold and over a wider area than that originally involved.2,3 In addition, neuroendocrine disturbances at the level of the hypothalamus or pituitary, involving decreased levels of growth hormone (GH), insulin-like growth factor (IGF), and possibly prolactin, have been found in FMS patients.4 These hormones are released during the stages of sleep, specifically GH in stage 3 and stage 4 of non–rapid eye movement (REM) sleep. In sleep studies, patients with FMS have disturbances with non-REM sleep and difficulty in progressing to stage 3 and stage 4 sleep, resulting in morning fatigue. One third of FMS patients have low IGF, an indication of low GH secretion, lending credence to disturbed stage 4 sleep as important in FMS. Treatment with GH increases IGF levels, improves pain and sleep, and reduces overall symptoms, although the cost is prohibitive.2,3 Other neuroendocrine abnormalities include elevation of cerebrospinal fluid substance P levels and dysregulated cortisol production. FMS patients have three times the levels of substance P, which is significant because this neurotransmitter plays a role in enhanced pain perception. This may be the reason for the heightened pain perception experienced by fibromyalgia patients. Alteration in the hypopituitary-adrenal axis with low production of cortisol, perhaps secondary to chronic stress response, contrasts with depression, in which high production of cortisol is found. These results suggest that part of the cause of FMS may be a product of disturbances in the autonomic and endocrine stress response systems.2 In addition, serotonin levels are low in the brain and in the platelets of patients with fibromyalgia. Although these theories explain part of the pathogenesis of FMS, the primary cause of the central dysregulation is unknown. FMS frequently follows physical or mental trauma, viral illness, and stress.
Fibromyalgia and Myofascial Pain Syndrome
Definition and Epidemiology
Pathophysiology
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree