Fever
Sarah A. Sterling and Alan E. Jones
Fever is one of the oldest and most widely recognized signs of disease and accounts for numerous adult and pediatric visits to the emergency department (ED). Although the exact temperature that constitutes a fever is debatable, most consider a rectal temperature of 38°C in children and a temperature of 38.3°C in adults to represent a fever.
Body temperature is regulated by the preoptic area of the anterior hypothalamus. This area acts like a thermostat, continuously balancing heat production versus heat loss. Heat production is controlled by altering the basal metabolic rate by varying the level of circulating thyroxin, which in turn increases cellular metabolism. In addition, body heat is produced by increasing muscle activity (shivering when cold or the shaking chill of a fever), the fastest and most sensitive means of heat production. The principal method of adjusting body heat loss is to vary the volume of blood flowing to the skin’s surface through vasoconstriction and vasodilation, decreasing and increasing heat loss, respectively. The exocrine sweat glands also contribute to heat loss, cooling the body by vaporization.
The hypothalamic thermostat has an inherent set point of about 37°C but ranges from 36° to 37.8°C. This set point is affected by the normal daily circadian rhythm, with temperatures lowest around 4 AM and gradually increasing throughout the day to peak between 6 and 10 PM. This diurnal pattern is often apparent in clinical practice with most fevers lower in the morning and higher in the evening. The phenomenon of night sweats, most commonly related to tuberculosis or lymphoma, represents a nocturnal fluctuation in the hypothalamic set point, causing a slight rise in body temperature that leads to reactive perspiration.
Not all elevations of body temperature necessarily constitute a fever. A true fever is an elevation in body temperature caused by a change in the hypothalamic set point. This new higher set point causes the body to engage its normal heat-generating mechanisms, like shivering or shaking, to raise the body temperature until the new set point is reached. In hyperthermia, however, the body attempts to maintain a normal temperature but its homeostatic mechanisms (i.e., vasodilation, increasing sweat production) are insufficient to reduce body temperature and eventually become overwhelmed. Temperatures >41°C (106°F) almost always represent hyperthermia and not a true fever (1,2).
Elevation of the hypothalamic set point appears to be mediated by cytokines, which are released from lymphocytes, monocytes, and macrophages in response to exogenous and endogenous pyrogens. Exogenous pyrogens include microorganisms and their metabolic by-products, drugs, and other toxins, and endogenous ones include neoplasms and metabolic processes. Cytokines travel via the bloodstream to the hypothalamus, where they act to increase prostaglandin synthesis, primarily prostaglandin E2 (PGE2). This causes an elevated cyclic adenosine monophosphate (cAMP) level, which raises the hypothalamic set point by affecting peripheral vasoconstriction and internal heat production. Fever is maintained until pyrogen levels fall or until prostaglandin production is inhibited. Aspirin, ibuprofen, and acetaminophen exert their antipyretic effects by blocking central hypothalamic prostaglandin synthesis, but have no effect on circulating pyrogens. Corticosteroids can block the release of endogenous pyrogens as well as inhibit prostaglandins but are relatively weak antipyretics, nevertheless.
Other cytokines produced in response to pyrogens include interleukins (ILs), tumor necrosis factor (TNF), and interferons (IFNs). It is generally believed that bacteria and their products of metabolism typically provoke release of IL-1. In contrast, viral proteins appear to stimulate IFN. IL-1 induces the liver to produce acute phase reactants, including C-reactive protein (CRP), which are responsible for the elevated erythrocyte sedimentation rate (ESR) associated with some fevers. Although IFN is a potent pyrogen, it does not enhance production of acute phase reactants. Though not yet clearly supported by data, this is the rationale behind the expectation of an elevated ESR and CRP level with a bacterial fever but not with one of viral etiology. Procalcitonin, the precursor to calcitonin produced in the thyroid, rises from undetectable in well individuals to measurable levels within 2 to 3 hours (peaking in 24 hours) in patients with sepsis. Some studies have suggested this marker, rather than the later rising CRP, may be more specific for infection. Several studies have examined the use of CRP and procalcitonin as potential biomarkers of sepsis, which could be used in clinical practice to differentiate patients with bacterial versus nonbacterial infections; however meta-analyses suggest that procalcitonin is not yet ready to be deployed into routine clinical practice (3). While the use of these biomarkers appears promising, research is ongoing to determine their clinical utilization.
Many metabolic abnormalities are associated with the febrile state. Fever increases both the oxygen tension (PO2) and the carbon dioxide tension (PCO2) and shifts the oxyhemoglobin dissociation curve to the right, resulting in lower oxygen saturation. Fever also seems to lower the seizure threshold, which can result in seizures in children who do not have a predisposition to epilepsy (febrile seizures). Fever can also cause reactivation of latent herpes simplex infections and other chronic viral conditions.
Although higher metabolic demands are placed on the febrile patient, evidence suggests that fever has some physiologic benefits and protective effects as well. Neutrophils, macrophages, and lymphocytes are most active at elevated temperatures. In addition, higher temperatures decrease the level of serum iron, a substrate needed by many bacteria to replicate. Fever also seems to inhibit certain viruses, such as Coxsackievirus and poliovirus (1,4).
Despite this, many patients and parents, as well as practitioners, believe that fever is harmful or likely to cause harm. Many studies have shown that “fever phobia,” initially described in the 1980s, persists. A recent study in a pediatric ED showed that more than 50% of caregivers would define fever at <37.8°C (100°F) and a large majority would treat a fever <37.8°C (5). Despite these beliefs, no studies have shown true fevers to be harmful. In addition, research has shown that the response to antipyretics does not allow the differentiation between serious (e.g., bacterial) and nonserious (e.g., viral) infections (2). Fever anxiety can be greatly reduced when patients and caregivers are educated on the risks and benefits of fever and its proper management.
CLINICAL PRESENTATION
Though most febrile patients present to the ED with a chief complaint of fever, many present with more generalized complaints. Elderly patients, or their caregivers, may complain of generalized weakness, malaise, or a change in mental status. Parents may bring in infants who are eating poorly or appear lethargic. In these patients, fever may be an incidental finding, discovered only on review of systems or review of vital signs.
In children, a fever documented at home should be treated as real, even in the absence of a documented fever in the ED. One study found that while children referred to an ED by a general practitioner were more severely ill, approximately one in four children who self-reported with parents required extensive diagnostic testing, intravenous (IV) or aerosolized medications, or hospital admission (6). Studies have also found parents can correctly detect fever by palpation alone with sensitivities and specificities as high as 91% and 79%, respectively, reported in one study (7). Further, although bundling of infants can affect skin temperature, research has shown it has no effect on the rectal temperature of a healthy infant; so elevated rectal temperatures should not be attributed to bundling (8).
In the elderly, fever may be more difficult to detect and define. Previous studies have shown that while mean rectal temperature was similar to younger patients (37°C), elderly patients had less diurnal variation (9). Another study found that lowering the definition of fever to 37.8°C (100°F) increased the sensitivity of predicting an infection to 70% (vs. 40% if 38.3°C is used), while the specificity remained at 90% (10). Elderly patients may also have an impaired ability to mount a fever response altogether, with 20% to 30% of elderly patients who had a serious bacterial or viral infection having a decreased or absent fever response in some studies. To complicate the evaluation of this patient population more, the elderly may have a delayed fever response as well, which can be delayed more than 12 hours in 12% of patients despite known infection (9).
Similarly, immunocompromised patients with a low-grade fever may suffer from an acute, life-threatening condition, but may be unable to mount a febrile response. These findings highlight the importance of a high index of suspicion for infection in the setting of functional decline in the elderly or immunocompromised patient, and the need for reassessment after initial physical examination and evaluation.
History
Important points to address in the history include the following:
• Duration and magnitude of fever
• Associated symptoms
• Close contacts with similar illness
• Past medical history associated with immunocompromise
• For example, HIV, diabetes, chronic renal failure, blood dyscrasia, alcohol or drug abuse
• Recent hospitalizations
• Presence of medical hardware
• For example, prosthetic valves, ventriculoperitoneal shunts
• Current medications
• Recent antibiotics or chronic steroid use
• Serotonergic or neuroleptic drug
• Last time and dose of antipyretics
• Recent travel
• Areas with endemic malaria, parasitic, or fungal infections
• Prolonged immobility or symptoms concerning for venous thromboembolism
• Occupational exposures
• For example, medical personnel or postal worker/governmental official with possible biologic weapon exposure
Physical Examination
The most important observation during the physical examination is the patient’s overall appearance and mental status. Specifically, does the patient look well or toxic? Does the patient have an altered mental status, which might indicate infection or sepsis, especially in the elderly? The overall impression of the patient and their general well-being is vital in determining pretest probabilities which will guide and direct the patient’s workup.
The importance of reviewing vital signs cannot be overstated. Tachycardia and hypotension should not be ignored or attributed solely to a febrile response or faulty reading. One study found that hypotension, even if it is transient, significantly increases mortality in patients admitted to the hospital with sepsis (11). In the presence of a fever, the pulse can be expected to increase by approximately 18 beats/min for each 1°C increase in temperature. However, some diseases are associated with relative bradycardia for the degree of fever (pulse–temperature dissociation). This dissociation is classically seen with typhoid fever, but may also be seen in Legionnaires’ disease, mycoplasmal infections, drug fever, factitious fever, and some viral syndromes. In addition, patients taking β-blockers may be unable to increase their pulse in response to a fever.
Tachypnea may also be an important indicator of significant infection or acid–base disturbance. Tachypnea and dyspnea are often suggestive of pulmonary disease, whereas tachypnea without dyspnea may indicate sepsis or metabolic acidosis of any cause. In a study of nursing home patients, tachypnea >25 was the highest predictor of disease, with a sensitivity of 90% and a specificity of 95% for pneumonia (12).
The history will usually direct the physician to the most likely source of infection, though this may be challenging in patients with an altered mental status. In the absence of localizing symptoms, a thorough examination should be undertaken. The entire body should be examined for rashes, decubitus ulcers, cellulitis, track marks (needle marks), or lymphadenopathy. Rashes may suggest a viral exanthem, vasculitis, meningococcemia, tick-borne infection (e.g., Rocky Mountain spotted fever or Lyme disease), or toxic shock syndrome (staphylococcal or streptococcal). Lymphadenopathy associated with fever may suggest malignancy, autoimmune disorders, or infection. Tender, localized adenopathy is usually associated with an infection in the region drained by the involved nodes, whereas malignant nodes are usually painless, rubbery, and firm. The most common cause of acute generalized adenopathy is infectious mononucleosis.
The head and neck examination may also offer important clues to the source of infection. Nuchal rigidity or meningismus may indicate meningitis; however, these signs are often absent, particularly in the elderly or children. The eyes should be examined for scleral icterus, which could indicate hepatitis, cholecystitis, or ascending cholangitis. Examination in and around the ears may reveal otitis externa or media or may suggest mastoiditis. The oropharynx may show evidence of pharyngitis, peritonsillar or retropharyngeal abscess, or periodontal infection. Purulent rhinorrhea may suggest sinusitis or, in children, a nasal foreign body. Sore throat, drooling, and fever may suggest epiglottitis. It is important to remember that patients may not present classically, so airway edema, stridor, or hoarseness should be taken seriously as they could indicate significant infection and a potential airway emergency.
The chest should be examined for indications of a pulmonary or cardiac cause of fever. Localized rales or rhonchi suggest pneumonia. As x-ray findings can lag behind physical findings, an early pneumonia may not be visible on x-ray. A pericardial rub is indicative of pericarditis, and a new heart murmur suggests endocarditis, especially in IV drug users. However, functional murmurs may increase because of fever-induced tachycardia.
The abdomen should be examined for signs of peritoneal irritation or ascites. Localized pain may suggest cholecystitis, appendicitis, pancreatitis, or diverticulitis. Suprapubic pain suggests a urinary tract infection (UTI), and should prompt an evaluation for costovertebral angle (CVA) tenderness, which could indicate pyelonephritis. A rectal examination may demonstrate evidence of a perirectal abscess or prostatitis. In male patients with a urethral discharge, a sexually transmitted infection is likely and a swollen or painful testicle suggests epididymoorchitis. In females, a pelvic examination can be performed to evaluate for vaginal and cervical discharges and/or cervical motion tenderness suggestive of pelvic inflammatory disease, tuboovarian abscesses, or a retained vaginal foreign body. In neonates, examination of the periumbilical area is necessary to evaluate for omphalitis.
Examination of the musculoskeletal system is often overlooked in febrile patients, but examination of the spine may reveal tenderness suggestive of osteomyelitis, discitis, or epidural abscess (especially in IV drug users). A detailed examination of the extremities may demonstrate a septic or inflamed joint, or it may suggest osteomyelitis, myositis, or deep vein thrombosis (DVT). In addition, any retained catheters, such as peripherally inserted central catheter (PICC) lines or hemodialysis (HD) ports, should be evaluated for erythema, rubor, or discharge surrounding the catheter and regarded as a potential source of infection.
DIFFERENTIAL DIAGNOSIS
Infection
Infection is the most common cause of fever. Infection may originate in any portion of the body and lead to a febrile response, whether from bacterial or viral etiology. Fever may indicate localized infection, or may indicate a more significant systemic process, like sepsis. One of the more challenging aspects of practicing emergency medicine is determining the significance of infection and identifying patients early in the spectrum of sepsis.
Systemic Inflammatory Response Syndrome and Sepsis
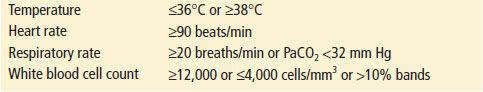
Systemic inflammatory response syndrome (SIRS) indicates that the body has initiated a global inflammatory/immune response. SIRS is associated with a higher likelihood for organ dysfunction and organ failure. Although SIRS can result from noninfectious etiologies, in the setting of suspected or confirmed infection, if a patient has two or more SIRS criteria (Table 10.1), they meet the definition of sepsis (13,14).
TABLE 10.1
SIRS Criteria
Severe Sepsis and Septic Shock
According to consensus definition, severe sepsis is sepsis, or suspected infection with systemic manifestations, and evidence of organ dysfunction. Septic shock is sepsis-induced hypotension (systolic blood pressure [SBP] <90 mm Hg or mean arterial pressure [MAP] <70 mm Hg, or an SBP 40 mm Hg below the patient’s baseline) that does not respond to IV fluids. In addition, patients may have evidence of tissue hypoperfusion as indicated by an elevated blood lactate level, oliguria, renal failure, coagulopathy, or acute lung injury (15). Despite much attention to this area and aggressive treatment strategies, once septic shock occurs, the mortality rate remains high.
Drug-Induced Hyperthermia Syndromes
Drug-induced hyperthermia syndromes include neuroleptic malignant syndrome (NMS), malignant hyperthermia (MH), and serotonin syndrome (SS). Because all three syndromes have similar presentations, with severe muscle contraction and hyperpyrexia, they share common complications of rhabdomyolysis, myoglobinemia, and intravascular hemolysis. Temperatures >42°C cause central nervous system (CNS) damage, initially to the more sensitive cerebellum and eventually to the cerebral cortex, brainstem, and spinal cord. Patients may also develop pulmonary embolism, cardiovascular collapse, myocardial infarction, and acute respiratory failure.
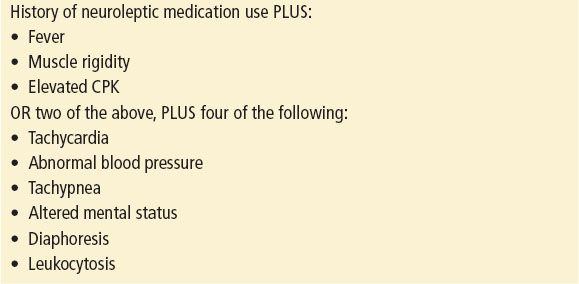
NMS is a rare idiosyncratic reaction to neuroleptic medications. It has also been reported in patients taking lithium. NMS is thought to result from dopamine depletion in the brain, possibly in combination with increased anticholinergic activity. NMS presents with fever (temperature in excess of 41°C has been reported), muscle rigidity, and elevated creatine phosphokinase (CPK). Other findings may include altered mental status and autonomic instability. Symptoms develop rapidly over 1 to 3 days. Muscular rigidity of the thorax may impair breathing. Autonomic dysfunction may cause severe variations of both blood pressure and pulse, and some patients may develop seizures (eTable 10.1).
eTABLE 10.1
Diagnostic Criteria for NMS