![]() Emergency venous access for fluid resuscitation, drug infusion, and renal dialysis
Emergency venous access for fluid resuscitation, drug infusion, and renal dialysis
![]() Infusions requiring central venous administration (vasopressors, calcium chloride, hyperosmolar solutions, hyperalimentation)
Infusions requiring central venous administration (vasopressors, calcium chloride, hyperosmolar solutions, hyperalimentation)
![]() Critically ill patients who cannot be placed flat or in Trendelenburg position due to respiratory distress
Critically ill patients who cannot be placed flat or in Trendelenburg position due to respiratory distress
![]() Access site for transvenous pacemaker
Access site for transvenous pacemaker
![]() Nonemergent venous access due to inadequate peripheral IV sites
Nonemergent venous access due to inadequate peripheral IV sites
CONTRAINDICATIONS
![]() No absolute contraindications
No absolute contraindications
![]() Relative Contraindications
Relative Contraindications
![]() Coagulopathic patients (femoral approach is preferred over the subclavian and internal jugular approaches because it is more easily compressed)
Coagulopathic patients (femoral approach is preferred over the subclavian and internal jugular approaches because it is more easily compressed)
![]() Combative or uncooperative patients
Combative or uncooperative patients
![]() Overlying infection, burn, or skin damage at puncture site
Overlying infection, burn, or skin damage at puncture site
![]() Trauma to the ipsilateral groin or lower extremity
Trauma to the ipsilateral groin or lower extremity
![]() Suspected proximal vascular injury, particularly of inferior vena cava (IVC)
Suspected proximal vascular injury, particularly of inferior vena cava (IVC)
![]() Ipsilateral renal transplant (risk of venous thrombosis)
Ipsilateral renal transplant (risk of venous thrombosis)
RISKS/CONSENT ISSUES
![]() Pain (local anesthesia will be administered)
Pain (local anesthesia will be administered)
![]() Local bleeding and hematoma
Local bleeding and hematoma
![]() Infection (sterile technique will be utilized)
Infection (sterile technique will be utilized)
![]() General Basic Steps
General Basic Steps
![]() Vessel localization
Vessel localization
![]() Analgesia
Analgesia
![]() Insertion
Insertion
![]() Seldinger technique
Seldinger technique
![]() Dilation
Dilation
![]() Catheter placement
Catheter placement
![]() Confirmation
Confirmation
![]() Flush and secure
Flush and secure
LANDMARK TECHNIQUE
Site of insertion is 2 to 3 cm inferior to the midpoint of inguinal ligament and 1 fingerbreadth medial to the femoral artery (FA) pulse (Figure 22.1). Anatomically, the structures underlying the inguinal ligament, from lateral to medial, are recalled by the mnemonic NAVEL.
Femoral Nerve
Common Femoral Artery
Common Femoral Vein
Empty Space
Lymphatics (FIGURE 22.1)
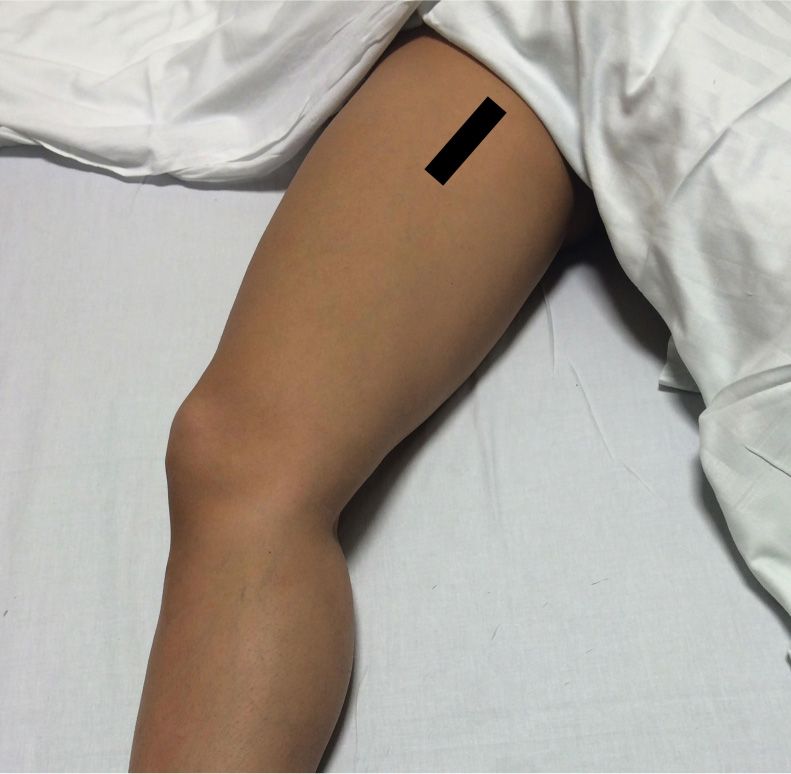
FIGURE 22.1 The thin line represents the pulsatile common femoral artery. The thick line 1 fingerbreadth medial to it represents the common femoral vein.
SUPPLIES
![]() Central Venous Catheter Kit
Central Venous Catheter Kit
![]() Drapes, chlorhexidine prep (2), gauze
Drapes, chlorhexidine prep (2), gauze
![]() Catheter (multiport, cordis, or hemodialysis)
Catheter (multiport, cordis, or hemodialysis)
![]() Guidewire within plastic sheath
Guidewire within plastic sheath
![]() Lidocaine, anesthesia syringe, and small-gauge needle
Lidocaine, anesthesia syringe, and small-gauge needle
![]() Three-inch introducer needle and syringe
Three-inch introducer needle and syringe
![]() Dilator
Dilator
![]() Scalpel
Scalpel
![]() Suture
Suture
![]() Sterile gloves, sterile gown, sterile cap and mask
Sterile gloves, sterile gown, sterile cap and mask
![]() Sterile drapes
Sterile drapes
![]() Sterile saline flushes
Sterile saline flushes
![]() Sterile port caps
Sterile port caps
![]() Ultrasound machine (optional)
Ultrasound machine (optional)
![]() Sterile ultrasound probe cover with sterile gel (optional)
Sterile ultrasound probe cover with sterile gel (optional)
TECHNIQUE
![]() Patient Preparation
Patient Preparation
![]() Cardiac monitoring to detect dysrhythmias triggered by wire advancement into the right ventricle
Cardiac monitoring to detect dysrhythmias triggered by wire advancement into the right ventricle
![]() Supplemental oxygen and continuous pulse oximetry monitoring
Supplemental oxygen and continuous pulse oximetry monitoring
![]() Externally rotate the leg and slightly bend the knee to expose the groin
Externally rotate the leg and slightly bend the knee to expose the groin
![]() If using ultrasound guidance, evaluate the right and left femoral veins (FVs) before prepping to confirm ideal vein location and compressibility
If using ultrasound guidance, evaluate the right and left femoral veins (FVs) before prepping to confirm ideal vein location and compressibility
![]() Sterilize the entire groin with chlorhexidine or povidone–iodine solution
Sterilize the entire groin with chlorhexidine or povidone–iodine solution
![]() Wear surgical cap, eye protection, mask, sterile gown and gloves
Wear surgical cap, eye protection, mask, sterile gown and gloves
![]() Drape with sterile sheets, covering the body liberally
Drape with sterile sheets, covering the body liberally
![]() If using ultrasound guidance, have an assistant place the probe (with gel applied) inside the sterile probe sheath
If using ultrasound guidance, have an assistant place the probe (with gel applied) inside the sterile probe sheath
Note: Unless immediate emergent access is warranted, the physicians attempting the procedure must wear cap, eye protection, and mask, along with sterile gown and gloves.
![]() Vessel Localization
Vessel Localization
![]() If attempting to localize the right FV, use the right hand to hold the introducer needle and syringe. With the left hand, palpate the FA to avoid arterial puncture while guiding needle insertion. If attempting to localize the left FV, reverse hands.
If attempting to localize the right FV, use the right hand to hold the introducer needle and syringe. With the left hand, palpate the FA to avoid arterial puncture while guiding needle insertion. If attempting to localize the left FV, reverse hands.
![]() Analgesia
Analgesia
![]() Use a small-gauge needle to anesthetize skin and subcutaneous tissue with 1% lidocaine
Use a small-gauge needle to anesthetize skin and subcutaneous tissue with 1% lidocaine
![]() Insertion
Insertion
![]() Attach a syringe to the introducer needle
Attach a syringe to the introducer needle
![]() Using the above landmarks, insert the introducer needle at a 30- to 60-degree angle to skin just medial to the palpated FA pulse
Using the above landmarks, insert the introducer needle at a 30- to 60-degree angle to skin just medial to the palpated FA pulse
![]() Apply negative pressure to the syringe plunger while advancing the needle 3 to 5 cm or until a flash of blood is seen in the syringe
Apply negative pressure to the syringe plunger while advancing the needle 3 to 5 cm or until a flash of blood is seen in the syringe
![]() If no flash is obtained, withdraw the needle slowly while continuing to aspirate
If no flash is obtained, withdraw the needle slowly while continuing to aspirate
![]() If redirecting the needle, always withdraw the needle to the level of skin before advancing again
If redirecting the needle, always withdraw the needle to the level of skin before advancing again
![]() Once the needle enters vessel, blood will flow freely into the syringe
Once the needle enters vessel, blood will flow freely into the syringe
![]() Stabilize and hold the introducer needle
Stabilize and hold the introducer needle
![]() Remove the syringe and ensure that venous blood continues to flow easily
Remove the syringe and ensure that venous blood continues to flow easily
![]() Use a finger to occlude the needle hub to prevent air embolism
Use a finger to occlude the needle hub to prevent air embolism
![]() Seldinger Technique
Seldinger Technique
![]() Advance the guidewire through the introducer needle. The wire should pass easily. Do not force it.
Advance the guidewire through the introducer needle. The wire should pass easily. Do not force it.
![]() Always hold on to the guidewire with one hand. Never let go of the guidewire.
Always hold on to the guidewire with one hand. Never let go of the guidewire.
![]() If resistance is met, withdraw the wire and rotate it, adjust the angle of needle entry, or remove the wire and reaspirate with the syringe to ensure the needle is still in the vessel.
If resistance is met, withdraw the wire and rotate it, adjust the angle of needle entry, or remove the wire and reaspirate with the syringe to ensure the needle is still in the vessel.
![]() When at least half of the guidewire is advanced through the needle, remove the needle over wire. Keep one hand holding the wire at all times.
When at least half of the guidewire is advanced through the needle, remove the needle over wire. Keep one hand holding the wire at all times.
![]() Make a superficial skin incision with the bevel of the scalpel blade angled away from wire
Make a superficial skin incision with the bevel of the scalpel blade angled away from wire
![]() Ensure the incision is large enough to allow easy passage for the dilator
Ensure the incision is large enough to allow easy passage for the dilator
![]() Dilation
Dilation
![]() Thread the dilator over the guidewire, always holding on to the wire
Thread the dilator over the guidewire, always holding on to the wire
![]() Advance the dilator through the skin into the vessel with a firm, twisting motion while holding the guidewire with the nondominant hand
Advance the dilator through the skin into the vessel with a firm, twisting motion while holding the guidewire with the nondominant hand
![]() Remove the dilator, leaving the guidewire in place
Remove the dilator, leaving the guidewire in place
![]() Catheter Placement
Catheter Placement
![]() Thread the catheter over the guidewire and retract the guidewire until it emerges from the catheter’s port
Thread the catheter over the guidewire and retract the guidewire until it emerges from the catheter’s port
![]() While holding the guidewire, advance the catheter through the skin into the vessel to the desired length
While holding the guidewire, advance the catheter through the skin into the vessel to the desired length
![]() Withdraw the guidewire through the catheter
Withdraw the guidewire through the catheter
![]() Use a syringe to aspirate blood from the catheter to confirm placement in the vein
Use a syringe to aspirate blood from the catheter to confirm placement in the vein
![]() Confirmation
Confirmation
![]() Manometry
Manometry
![]() Blood gas analysis
Blood gas analysis
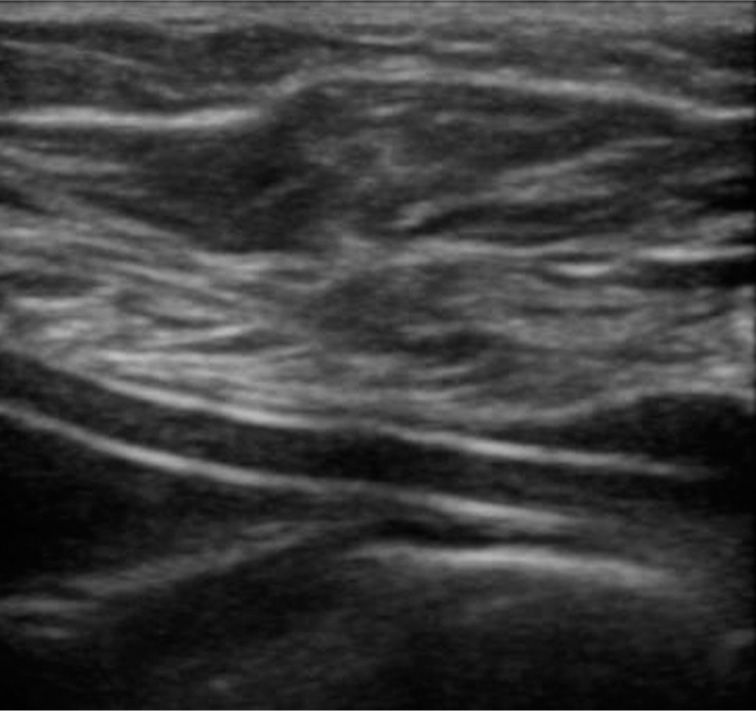
![]() Sonographic confirmation of the catheter in the vein (Figure 22.2)
Sonographic confirmation of the catheter in the vein (Figure 22.2)
![]() Postprocedure chest x-ray (CXR)
Postprocedure chest x-ray (CXR)
![]() Confirm the catheter tip in the superior vena cava just proximal to the right atrium
Confirm the catheter tip in the superior vena cava just proximal to the right atrium
![]() Rule out pneumothorax
Rule out pneumothorax
![]() Flush and Secure
Flush and Secure
![]() Aspirate, flush, and heplock each central line lumen
Aspirate, flush, and heplock each central line lumen
![]() Suture the catheter to the skin using silk or nylon sutures
Suture the catheter to the skin using silk or nylon sutures
![]() Cover the skin insertion site with a sterile dressing (bacteriostatic if available) (FIGURE 22.2)
Cover the skin insertion site with a sterile dressing (bacteriostatic if available) (FIGURE 22.2)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree