Chapter 26 Facial, ENT, and Dental Emergencies
Medical problems of the face, ears, nose, throat, and mouth involve multiple conditions including infections, foreign bodies, and thrombotic or embolic events. Regardless of the patient’s chief complaint, the first priority for these patients is assessment and management of airway, breathing, and circulation. The focus of this chapter is medical emergencies related to the face; see also Chapter 41, Facial, Ocular, ENT, and Dental Trauma.
Facial Emergencies
Bell’s Palsy
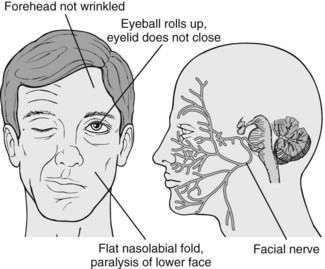
Bell’s palsy is a unilateral facial paralysis caused by damage to the facial nerve (cranial nerve VII), often the result of the herpes simplex virus. Symptoms can take weeks or months to resolve and some individuals will have permanent sequelae. Bell’s palsy is a diagnosis of exclusion. Patients must be fully evaluated to rule out stroke, meningitis, or a tumor affecting the facial nerve.1
Signs and Symptoms
• Unilateral facial paralysis with facial drooping (Fig. 26-1)
• Inability to blink or close the affected eye
• Increased or decreased unilateral tear production
• Ipsilateral loss of taste (one side of the tongue)
• A perception that sound is louder in the ear on the affected side (hyperacusis)
Trigeminal Neuralgia (Tic Douloureux)
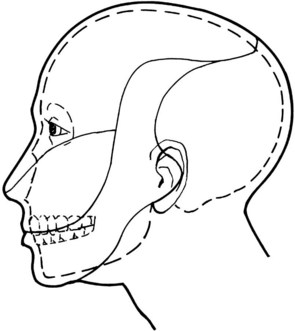
Trigeminal neuralgia, also known as tic douloureux, is defined by the International Association for the Study of Pain as “a sudden, usually unilateral, severe, brief, stabbing, recurrent pain in the distribution of one or more branches of the fifth cranial nerve.”2 The trigeminal nerve (cranial nerve V) divides into three branches: ophthalmic nerve (V1), maxillary nerve (V2), and mandibular nerve (V3). The two branches most often affected are V2 and V3. Trigeminal neuralgia is often accompanied by facial spasm called a tic and occurs most often in females over the age of 60 years. The pain may be precipitated by normal daily activities such as brushing one’s teeth or chewing.3
Signs and Symptoms
• Excruciating, stabbing, electric shock–like pain lasting seconds to several minutes
• Generally unilateral, rarely bilateral
• Usually involves the lips, cheeks, jaw, eyes, forehead, scalp, and nose (Fig. 26-2)
Therapeutic Interventions
• A trial of carbamazepine (Tegretol) can be therapeutic as well as diagnostic. If this drug does not ease the pain, it suggests that trigeminal neuralgia is not the cause of the pain.
• Carbamazepine and baclofen have been suggested as a synergistic combination to decrease pain.4,5
• Inform the patient that exacerbations generally occur in fall and spring months.
Periorbital (Preseptal) and Orbital Cellulitis
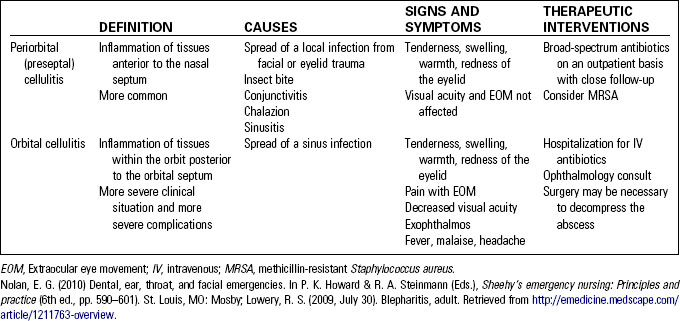
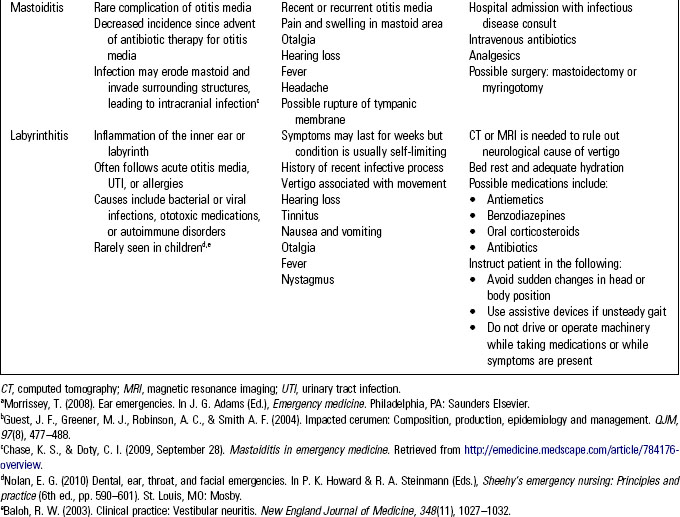
Periorbital and orbital cellulitis are infections caused by common respiratory pathogens such as Streptococcus pneumoniae (most common organism), Staphylococcus aureus, Streptococcus pyogenes, and Haemophilus influenzae. Diagnosis is based on clinical examination; computed tomography (CT) scan and magnetic resonance imaging (MRI) may be obtained nonetheless. One of the greatest concerns with periorbital or orbital cellulitis is the potential for it to lead to meningitis. Table 26-1 compares periorbital and orbital cellulitis.
Cavernous Sinus Thrombosis
Cavernous sinus thrombosis (CST) (Fig. 26-3) is a rare but potentially life-threatening infection of a blood clot in one or both of the cavernous sinuses. The cavernous sinuses are located at the base of the skull and receive venous blood from the facial veins. As a result, infections of the face, tonsils, and orbits can spread to the cavernous sinuses. CST usually follows midfacial cellulitis or paranasal sinus infection. S. aureus (70%) and Streptococcus are the most frequent causative pathogens.6 The mortality rate for CST is 30% in all patients; in those with underlying sphenoid sinusitis, mortality is up to 50%.6 Death occurs from overwhelming sepsis or neurologic infection.
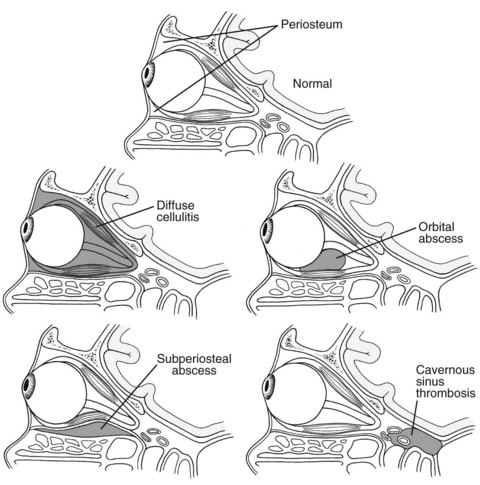
Fig. 26-3 Location of orbital cellulitis and cavernous sinus thrombosis.
(Reprinted with permission of Garrity, J. (2008, September). Preseptal and orbital cellulitis. The Merck manuals online. Retrieved from http://www.merckmanuals.com/professional/eye_disorders/orbital_diseases/preseptal_and_orbital_cellulitis.html?qt=prespetal%20and%20orbital%20cellulitis&alt=sh.)
Signs and Symptoms
• History of sinusitis or midfacial infection
• Symptoms of CST are similar to those of periorbital and orbital cellulitis
• Headache is the most common symptom
• Chemosis—edema of the conjunctiva and mucous membrane of the eyelid
• Decreased visual acuity resulting from increased intraocular pressure
• Ptosis and impaired eye movement resulting from dysfunction of cranial nerves III, IV, V, and VI
• Meningeal signs such as nuchal rigidity and Kernig and Brudzinski signs
Therapeutic Interventions
• Immediate intravenous administration of broad-spectrum antibiotics.
• Administration of anticoagulants and steroids is questionable.6 Steroids may be considered to prevent adrenal crisis if the course of CST leads to pituitary insufficiency.
• Infectious disease and surgical consults are recommended.
• Possible admission to intensive care unit if sinus drainage is indicated.
Ear, Nose, and Throat Emergencies
Infections of the Ear
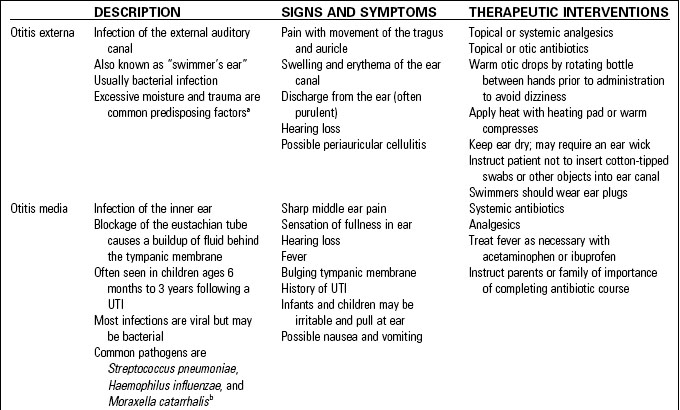
Infections of the ear and their possible complications are compared in Table 26-2.
Cerumen Impaction
Cerumen is produced in the outer ear to repel moisture and trap debris and microorganisms. Cerumen normally moves to the opening of the ear canal, where it can be washed away. Overproduction of cerumen or anatomical narrowing of the external canal may cause an impaction of the cerumen. Impaction may also occur if cotton-tipped swabs push the cerumen deep into the inner ear canal, where it can obstruct the tympanic membrane.7