CHAPTER 23
Facet Joint Interventions: Intra-Articular Injections, Medial Branch Blocks, and Radiofrequency Ablations
INTRODUCTION
• The prevalence of persistent low back pain secondary to involvement of lumbosacral facet joints has been described in controlled studies as varying from 15% to 45% based on types of populations and setting studies. Lumbar facet joint interventions are used to diagnose as well as treat facet joint–related pain.
• Prevalence of thoracic facet joint pain has been shown to be 34% to 48% in patients with chronic thoracic back pain.
• Prevalence of cervical facet joint pain has been shown to be 36% to 67% in patients with chronic neck pain.
INTRA-ARTICULAR FACET JOINT INJECTIONS AND MEDIAL BRANCH BLOCKS
Indications
Common indications for diagnostic facet joint interventions include the following:
• Lumbar spine
![]() Traumatic or arthritic nonradicular low back pain.
Traumatic or arthritic nonradicular low back pain.
![]() Patients can experience pain radiating in to the buttock but rarely radiating beyond the level of the knee.
Patients can experience pain radiating in to the buttock but rarely radiating beyond the level of the knee.
![]() Pain on palpation is worse with extension of the lumbar spine and rotation or twisting of spine.
Pain on palpation is worse with extension of the lumbar spine and rotation or twisting of spine.
• Thoracic spine
![]() Traumatic or arthritic nonradicular upper back or posterior chest wall pain.
Traumatic or arthritic nonradicular upper back or posterior chest wall pain.
![]() Typically the patient experiences pain on palpation and extension and rotation or twisting of thoracic spine.
Typically the patient experiences pain on palpation and extension and rotation or twisting of thoracic spine.
• Cervical spine
![]() Traumatic or arthritic neck pain, suboccipital headache, persistent and disabling axial neck and/or upper thoracic pain or suspected cervicogenic headache
Traumatic or arthritic neck pain, suboccipital headache, persistent and disabling axial neck and/or upper thoracic pain or suspected cervicogenic headache
![]() Typically pain and/or headache with neck movements in flexion, extension, and rotations
Typically pain and/or headache with neck movements in flexion, extension, and rotations
• Duration of pain of at least 3 months
• Average pain level of >5 on a scale of 0 to 10
• Intermittent or continuous pain causing functional disability
• Failure to respond to more conservative management including physical therapy modalities with exercises and nonsteroidal anti-inflammatory agents
• Lack of evidence either for discogenic or sacroiliac joint pain
• Lack of disk herniation or evidence of radiculitis
CONTRAINDICATIONS
Common contraindications for facet joint interventions include the following:
• Suspected or proven discogenic, sacroiliac joint or myofascial pain in case of lumbar facet interventions
• Allergies to drugs being considered for the procedure
• Inability of patient to understand consent, nature of the procedure, needle placement, or sedation
• Localized or generalized infection
• Anticoagulation therapy
• Nonaspirin combination antiplatelet therapy
• Pregnancy
• Bleeding diathesis
• Needle phobia
• Psychogenic pain
RELEVANT ANATOMY
Lumbar Spine
• Facet joints (Figure 23-1)
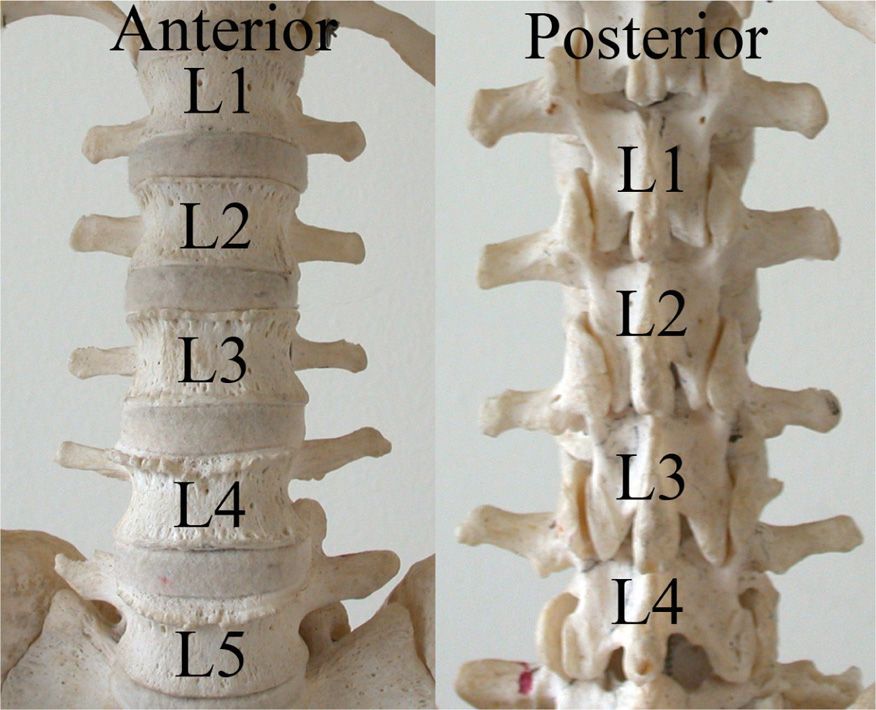
Figure 23-1. Lumbar spine and facet joints. Note the varying angles of the facets from top to bottom.
![]() Lumbar facet joints are formed by the articulation of the inferior articular process of the superior lumbar vertebra with the superior articular process of the inferior vertebra.
Lumbar facet joints are formed by the articulation of the inferior articular process of the superior lumbar vertebra with the superior articular process of the inferior vertebra.
![]() The lumbar joints exhibit features of typical synovial joints.
The lumbar joints exhibit features of typical synovial joints.
![]() The articular facets are covered by articular cartilage, and the synovial membrane bridges the margins of the articular cartilage of the two facets in each joint.
The articular facets are covered by articular cartilage, and the synovial membrane bridges the margins of the articular cartilage of the two facets in each joint.
![]() Surrounding the synovial membrane is a joint capsule that attaches to the articular process, a short distance beyond the margins of the articular cartilage.
Surrounding the synovial membrane is a joint capsule that attaches to the articular process, a short distance beyond the margins of the articular cartilage.
• Ligaments
![]() Ligaments connect spinous process, lamina, and bodies of the adjacent vertebrae.
Ligaments connect spinous process, lamina, and bodies of the adjacent vertebrae.
![]() Anterior and posterior longitudinal ligaments help stabilize the joints.
Anterior and posterior longitudinal ligaments help stabilize the joints.
![]() The articular capsule surrounds facets and allows gliding motions.
The articular capsule surrounds facets and allows gliding motions.
![]() In the lumbar spine, L4-L5 permits most flexion.
In the lumbar spine, L4-L5 permits most flexion.
![]() The anterior longitudinal ligament attaches to the anterior bodies and the intervertebral disk. It is strong and prevents hyperextension.
The anterior longitudinal ligament attaches to the anterior bodies and the intervertebral disk. It is strong and prevents hyperextension.
![]() The posterior longitudinal ligaments attaches to the posterior aspect of the vertebral bodies and intervertebral disks. It is weaker than the anterior longitudinal ligament and permits hyperflexion.
The posterior longitudinal ligaments attaches to the posterior aspect of the vertebral bodies and intervertebral disks. It is weaker than the anterior longitudinal ligament and permits hyperflexion.
![]() Ligamentum flavum connects adjacent laminae of vertebrae and limits flexion. Interspinous ligaments connect the spinous processes. These are weak ligaments. Intertransverse ligaments connect the transverse process and are also weak ligaments.
Ligamentum flavum connects adjacent laminae of vertebrae and limits flexion. Interspinous ligaments connect the spinous processes. These are weak ligaments. Intertransverse ligaments connect the transverse process and are also weak ligaments.
• Innervation (Figure 23-2D)
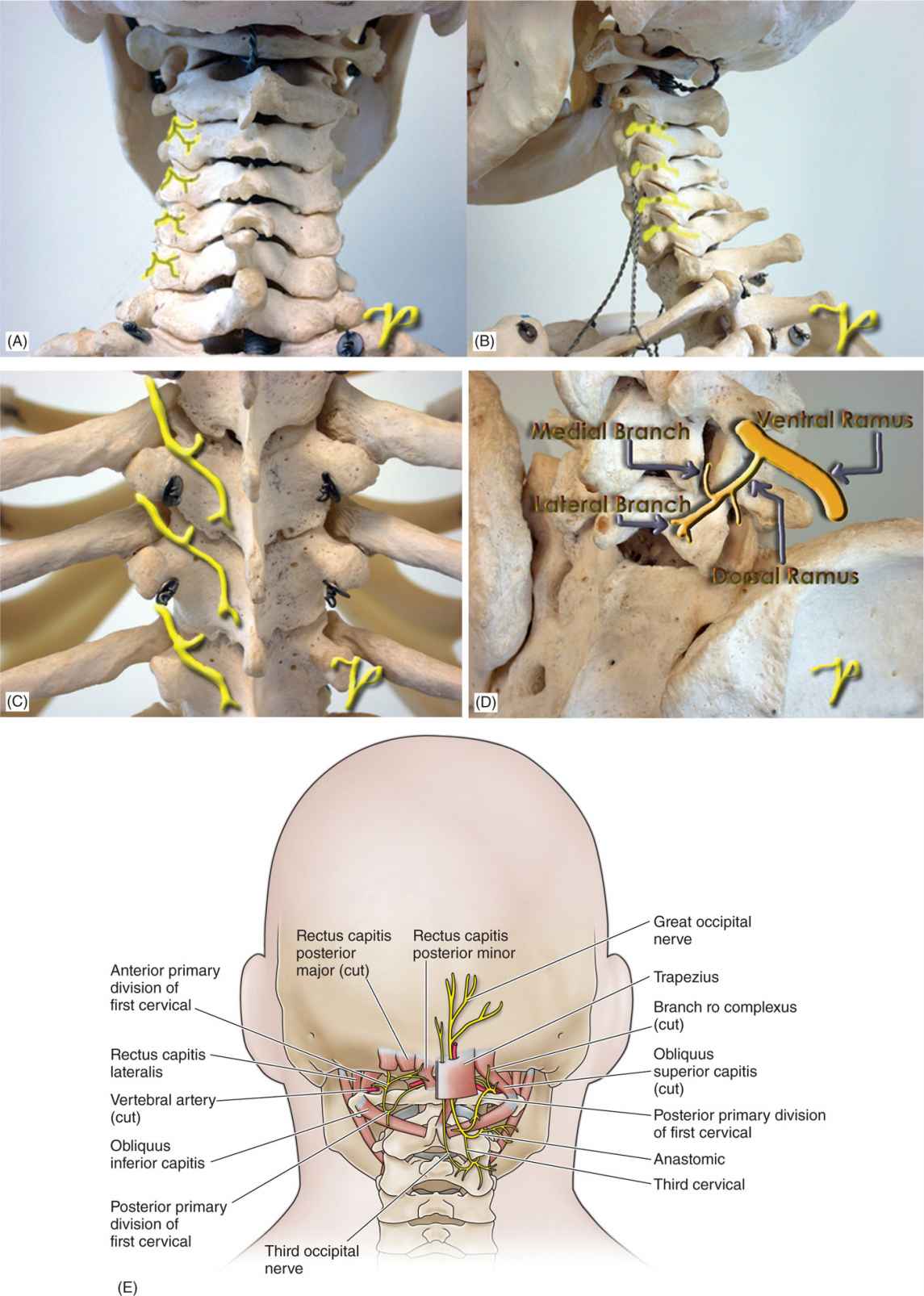
Figure 23-2. (A-E) Cervical, thoracic, and lumbar medial branches.
![]() The capsules of the lumbar facet joints are richly innervated with encapsulated and unencapsulated free nerve endings.
The capsules of the lumbar facet joints are richly innervated with encapsulated and unencapsulated free nerve endings.
![]() Lumbar facet joints are appropriately equipped with sensory apparatus to transmit nociceptive and proprioceptive information.
Lumbar facet joints are appropriately equipped with sensory apparatus to transmit nociceptive and proprioceptive information.
![]() Each lumbar facet joint has dual innervations being supplied by two medial branches of dorsal rami (Figure 23-2D).
Each lumbar facet joint has dual innervations being supplied by two medial branches of dorsal rami (Figure 23-2D).
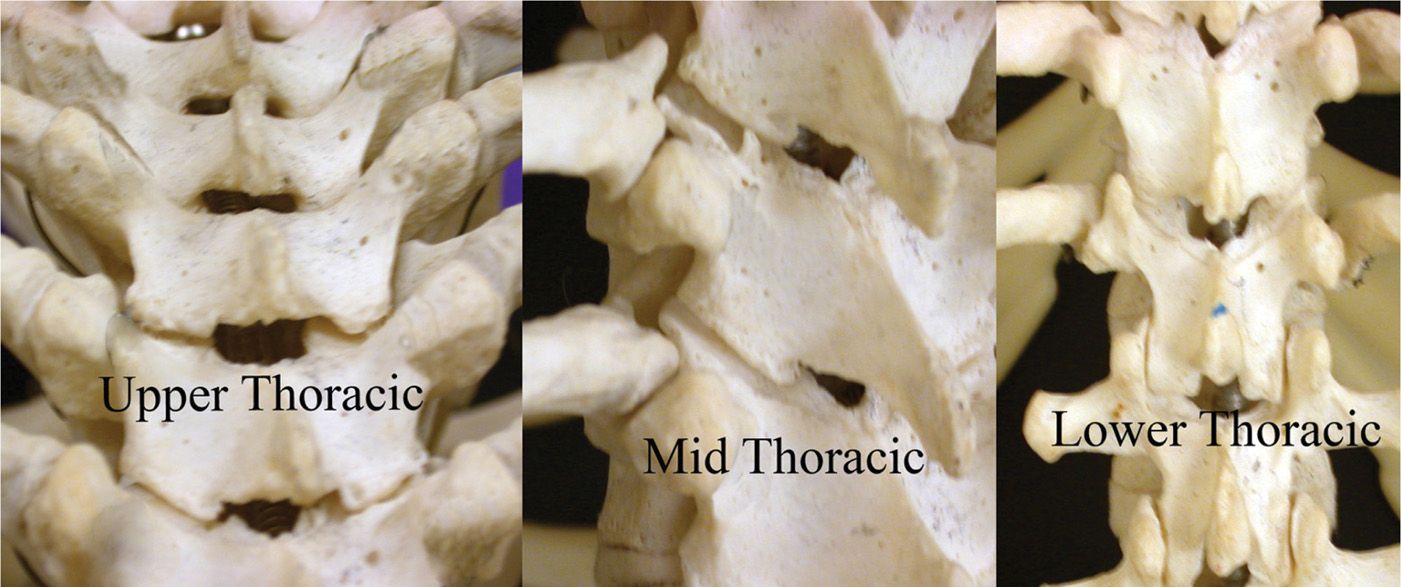
Figure 23-3. Thoracic facet joints: Note the slanted angles at the middle levels and compare with the upper and lower facets. The interspinous opening for epidural access is minimal in the mid thoracic levels where the angles of the facets are most slanted.
![]() The medial brunches of the L1-L4 dorsal rami have a constant and similar course.
The medial brunches of the L1-L4 dorsal rami have a constant and similar course.
![]() Each nerve emerges from its intervertebral foramen and enters the posterior compartment of the back by coursing around the neck of the superior articular process.
Each nerve emerges from its intervertebral foramen and enters the posterior compartment of the back by coursing around the neck of the superior articular process.
![]() Hugging the neck of the superior articular process, the medial branch passes caudally and slightly dorsally covered by mamillo-accessory ligament, hooking medially around the caudal aspect of the root of the superior articular process to enter the multifidus muscle.
Hugging the neck of the superior articular process, the medial branch passes caudally and slightly dorsally covered by mamillo-accessory ligament, hooking medially around the caudal aspect of the root of the superior articular process to enter the multifidus muscle.
![]() Intermediate and lateral branches arise from the dorsal ramus at the same point as the medial branch.
Intermediate and lateral branches arise from the dorsal ramus at the same point as the medial branch.
![]() The medial branch finally crosses the vertebral lamina where it divides into multiple branches that supply the multifidus muscle, the intraspinous ligament and muscle, and ligament and the two facet joints.
The medial branch finally crosses the vertebral lamina where it divides into multiple branches that supply the multifidus muscle, the intraspinous ligament and muscle, and ligament and the two facet joints.
![]() The medial branch of the L5 dorsal ramus has a different course and distribution than those of the L1-L4 dorsal rami. Instead of crossing a transverse process, the L5 dorsal ramus crosses the ala of the sacrum.
The medial branch of the L5 dorsal ramus has a different course and distribution than those of the L1-L4 dorsal rami. Instead of crossing a transverse process, the L5 dorsal ramus crosses the ala of the sacrum.
![]() The L5 dorsal ramus is much longer than the typical lumbar levels.
The L5 dorsal ramus is much longer than the typical lumbar levels.
![]() From the L5-S1 intervertebral foramen, the medial branch of the L5 dorsal ramus runs along the groove by the junction of the ala and the root of the superior articular process of the sacrum before hooking medially around the base of the lumbosacral facet joint (Figure 23-2D).
From the L5-S1 intervertebral foramen, the medial branch of the L5 dorsal ramus runs along the groove by the junction of the ala and the root of the superior articular process of the sacrum before hooking medially around the base of the lumbosacral facet joint (Figure 23-2D).
Thoracic Spine (Figure 23-3)
• Facet joints
![]() The thoracic spine has unique features that differentiate it from the lumbar spine.
The thoracic spine has unique features that differentiate it from the lumbar spine.
![]() Each thoracic vertebra is distinguished by costal facets on the side of the body, and all but the last 2 or 3 segments by articular facets on the transverse process, articulating respectively with the heads and tubercles of the ribs.
Each thoracic vertebra is distinguished by costal facets on the side of the body, and all but the last 2 or 3 segments by articular facets on the transverse process, articulating respectively with the heads and tubercles of the ribs.
![]() The laminae are short, thick, broad, and overlap each other like roof tiles from above downward.
The laminae are short, thick, broad, and overlap each other like roof tiles from above downward.
![]() The typical spinous process slants posteriorly and downward overlapping between T5 and T8 and being less oblique above and below this level.
The typical spinous process slants posteriorly and downward overlapping between T5 and T8 and being less oblique above and below this level.
![]() Projecting upward at the junction of the lamina and pedicles are the superior articular processes facing backward, upward, and laterally.
Projecting upward at the junction of the lamina and pedicles are the superior articular processes facing backward, upward, and laterally.
![]() The articular processes of adjoining thoracic vertebrae form synovial joints, which permit a limited degree of movement, primarily facilitating axial rotation.
The articular processes of adjoining thoracic vertebrae form synovial joints, which permit a limited degree of movement, primarily facilitating axial rotation.
![]() The primary axis of rotation for the mid-thoracic segments is located close to the anterior region of the thoracic intervertebral disk.
The primary axis of rotation for the mid-thoracic segments is located close to the anterior region of the thoracic intervertebral disk.
![]() The lower thoracic zygapophysial joints (facets) provide specialized features with the characteristics of this region. There is greater developmental of the mamillary processes, which originate as extension of the superior articular process.
The lower thoracic zygapophysial joints (facets) provide specialized features with the characteristics of this region. There is greater developmental of the mamillary processes, which originate as extension of the superior articular process.
![]() The mamillary process provides attachment for the multifidus muscle as it covers this medially to attach onto the spinous process of the segments above.
The mamillary process provides attachment for the multifidus muscle as it covers this medially to attach onto the spinous process of the segments above.
![]() Small intra-articular synovial folds may be found within the thoracic facet joints. Intra-articular synovial folds originate medially from tissues adjacent to the ligamentum flavum and extend varying distances into the medial joint cavity filling spaces within the joint with fibrofatty tissue.
Small intra-articular synovial folds may be found within the thoracic facet joints. Intra-articular synovial folds originate medially from tissues adjacent to the ligamentum flavum and extend varying distances into the medial joint cavity filling spaces within the joint with fibrofatty tissue.
![]() The articular surface of the thoracic facet joint is inclined to 60 degrees from the horizontal to the frontal plane and rotated 20 degrees from the frontal to the sagittal plane in a medial direction.
The articular surface of the thoracic facet joint is inclined to 60 degrees from the horizontal to the frontal plane and rotated 20 degrees from the frontal to the sagittal plane in a medial direction.
![]() The lateral aspect of the thoracic joint is placed anterior and the medial aspect of the joint is placed posterior.
The lateral aspect of the thoracic joint is placed anterior and the medial aspect of the joint is placed posterior.
![]() The superior articular facet from the inferior vertebrae is almost flat and faces posterior, superior, and slightly lateral.
The superior articular facet from the inferior vertebrae is almost flat and faces posterior, superior, and slightly lateral.
![]() The inferior articular facet is oriented in a reciprocal manner. There is variation in the inclination of the joints by region with the mid-thoracic level approximately 60 degrees off the horizontal plane while the upper segment has a more vertical orientation.
The inferior articular facet is oriented in a reciprocal manner. There is variation in the inclination of the joints by region with the mid-thoracic level approximately 60 degrees off the horizontal plane while the upper segment has a more vertical orientation.
![]() In contrast to the lumbar spine, the superior and inferior articular processes of the thoracic spine cannot be identified separately because the joints are mostly in the frontal plane and do not face sideward.
In contrast to the lumbar spine, the superior and inferior articular processes of the thoracic spine cannot be identified separately because the joints are mostly in the frontal plane and do not face sideward.
![]() The articular pillar is wider in the thoracic level, and it extends further laterally in relation to the vertebral bodies.
The articular pillar is wider in the thoracic level, and it extends further laterally in relation to the vertebral bodies.
![]() The articular facets are covered by articular cartilage, and the synovial membrane bridges the margins of the articular cartilage of the 2 facets in each joints.
The articular facets are covered by articular cartilage, and the synovial membrane bridges the margins of the articular cartilage of the 2 facets in each joints.
![]() Fluoroscopic visualization is more difficult.
Fluoroscopic visualization is more difficult.
![]() There is no fibrous capsule on the ventral aspect of the joint. Within interspace, the ligamentum flavum is in direct contact with the synovial membrane.
There is no fibrous capsule on the ventral aspect of the joint. Within interspace, the ligamentum flavum is in direct contact with the synovial membrane.
• Innervation of the thoracic facet joints (Figure 23-2C)
![]() The thoracic facet joints receive bisegmental innervations from the medial branch of the dorsal ramus of the upper segment and one more cephalad level.
The thoracic facet joints receive bisegmental innervations from the medial branch of the dorsal ramus of the upper segment and one more cephalad level.
![]() The medial branches of the thoracic dorsal rami were found to have a reasonably constant course except at mid-thoracic level (T5-T8).
The medial branches of the thoracic dorsal rami were found to have a reasonably constant course except at mid-thoracic level (T5-T8).
![]() The medial branches of the thoracic dorsal rami at mid-thoracic levels do not run on bone. Instead, they are suspended in the intertransverse space.
The medial branches of the thoracic dorsal rami at mid-thoracic levels do not run on bone. Instead, they are suspended in the intertransverse space.
![]() Thoracic medial branches are not that close to the facet joint as they swing laterally to circumvent the multifidus muscle.
Thoracic medial branches are not that close to the facet joint as they swing laterally to circumvent the multifidus muscle.
![]() The dorsal ramus is separated from the ventral ramus (that is, the intercostal nerves) by the anterior part of the superior costotransverse ligament.
The dorsal ramus is separated from the ventral ramus (that is, the intercostal nerves) by the anterior part of the superior costotransverse ligament.
![]() In the thoracic region, the dorsal ramus is short, common trunk of 3 mm to 5 mm, which bifurcates immediately dorsal to the superior costotransverse ligament into a medial and lateral branch.
In the thoracic region, the dorsal ramus is short, common trunk of 3 mm to 5 mm, which bifurcates immediately dorsal to the superior costotransverse ligament into a medial and lateral branch.
![]() The medial branches supply the adjacent intrinsic muscles of the back, the facet joints and skin in the upper thoracic region; the lateral branches supply intrinsic muscles, costotransverse joint, and the skin in the lower thoracic spine.
The medial branches supply the adjacent intrinsic muscles of the back, the facet joints and skin in the upper thoracic region; the lateral branches supply intrinsic muscles, costotransverse joint, and the skin in the lower thoracic spine.
![]() Spinous processes of T1-T3 and T11-T12 are located approximately at the level of the facet joint of adjoining level and the one below; T2 spinous process relates to T2-T3 facet joint level.
Spinous processes of T1-T3 and T11-T12 are located approximately at the level of the facet joint of adjoining level and the one below; T2 spinous process relates to T2-T3 facet joint level.
![]() Spinous processes T4-T10 are located halfway between the adjacent facet joints and the joints below.
Spinous processes T4-T10 are located halfway between the adjacent facet joints and the joints below.
Cervical Spine (Figure 23-4)
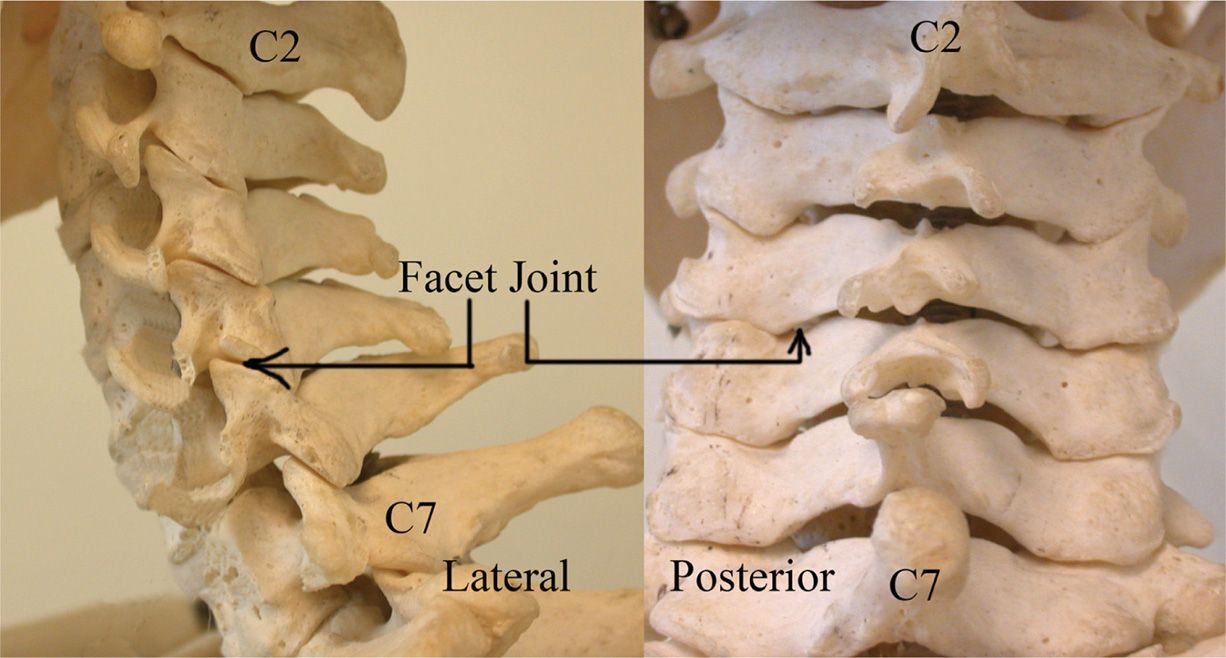
Figure 23-4. Cervical spine and facets.
• Cervical facet joints from C2-C3 to C7-T1
![]() The atlanto-occipital and the atlanto-axial synovial joints are also present in the cervical spine as two paired joints, but are not considered to be facet joints as they are anterior rather than posterior spinal structures. (See Chapters 14 and 15.)
The atlanto-occipital and the atlanto-axial synovial joints are also present in the cervical spine as two paired joints, but are not considered to be facet joints as they are anterior rather than posterior spinal structures. (See Chapters 14 and 15.)
![]() The cervical facet joints are formed by the inferior articular process of the superior vertebral segment and the superior articular process of the inferior vertebral segment.
The cervical facet joints are formed by the inferior articular process of the superior vertebral segment and the superior articular process of the inferior vertebral segment.
![]() The superior aspect of the facet joint faces forward and downward at 45 degrees, whereas the inferior aspect of the facet joint faces backward and upward at 45 degrees.
The superior aspect of the facet joint faces forward and downward at 45 degrees, whereas the inferior aspect of the facet joint faces backward and upward at 45 degrees.
![]() The facet joints in the cervical spine form paired vertebral column or “pillar” which together with a discovertebral unit provides the 3-prong structural support for this cervical segment.
The facet joints in the cervical spine form paired vertebral column or “pillar” which together with a discovertebral unit provides the 3-prong structural support for this cervical segment.
![]() The obliquity of the facet joints allows degrees of flexion, extension, and rotation.
The obliquity of the facet joints allows degrees of flexion, extension, and rotation.
![]() The articular facets are covered by articular cartilage, and a synovial membrane bridges the margins of the articular cartilage of the 2 facets in each joint.
The articular facets are covered by articular cartilage, and a synovial membrane bridges the margins of the articular cartilage of the 2 facets in each joint.
![]() The cervical facet joints may contain a variety of intra-articular inclusions with fibroid-exposed meniscoid being the most common inclusions.
The cervical facet joints may contain a variety of intra-articular inclusions with fibroid-exposed meniscoid being the most common inclusions.
![]() The average joint volume is >1 mL.
The average joint volume is >1 mL.
• Innervation (Figure 23-2A, B, E)
![]() The cervical facet joints are well innervated by the medial branches of the dorsal rami. The fibrous joint capsule is richly innervated with mechanoreceptors as well as nociceptive receptors.
The cervical facet joints are well innervated by the medial branches of the dorsal rami. The fibrous joint capsule is richly innervated with mechanoreceptors as well as nociceptive receptors.
![]() The innervation of the atlanto-occipital and atlanto-axial joints is derived from C1 and C2 root, respectively.
The innervation of the atlanto-occipital and atlanto-axial joints is derived from C1 and C2 root, respectively.
![]() Cervical facet joints below C2-C3 are supplied by the medial branches of the cervical dorsal rami above and below the joint.
Cervical facet joints below C2-C3 are supplied by the medial branches of the cervical dorsal rami above and below the joint.
![]() The C2-C3 joint is also supplied by the third occipital nerve.
The C2-C3 joint is also supplied by the third occipital nerve.
![]() Each C3-C7 dorsal ramus crosses the same segments, transverse process, and divides into lateral and medial branches.
Each C3-C7 dorsal ramus crosses the same segments, transverse process, and divides into lateral and medial branches.
![]() The medial branch crosses around the waist of the articular processes of the same numbered vertebra.
The medial branch crosses around the waist of the articular processes of the same numbered vertebra.
![]() The medial branches are bound by fascia, held against the articular pillar and covered by the tendinous slips of the origin of the semispinalis capitis.
The medial branches are bound by fascia, held against the articular pillar and covered by the tendinous slips of the origin of the semispinalis capitis.
![]() Articular branches arise as the nerve approaches the posterior aspect of the articular pillar within ascending branch innervating the joint above and a descending branch innervating the joint below.
Articular branches arise as the nerve approaches the posterior aspect of the articular pillar within ascending branch innervating the joint above and a descending branch innervating the joint below.
![]() At C7, in contrast to C3-C6, the medial branches are located at the higher level due to the transverse process. At C7, the base of the transverse process occupies most of the lateral aspect of the articular pillar pushing the medial branch higher.
At C7, in contrast to C3-C6, the medial branches are located at the higher level due to the transverse process. At C7, the base of the transverse process occupies most of the lateral aspect of the articular pillar pushing the medial branch higher.
![]() The course of the C4 and C5 medial branch nerves has been shown to be relatively constant crossing the waist of the respective articular pillars.
The course of the C4 and C5 medial branch nerves has been shown to be relatively constant crossing the waist of the respective articular pillars.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






