
Eye Trauma
Kevin J. Knoop and William Dennis
Eye trauma accounts for approximately 1% of annual ED visits, with more than 2 million ocular injuries yearly (1). Of these, 60,000 require admission, and lasting visual impairment results in approximately 50,000. The emergency physician (EP) has an important role in the diagnosis, management, and referral of eye injuries. Thus, the EP must be cognizant of the spectrum of ocular trauma to preserve vision and prevent disability.
CLINICAL PRESENTATION
A rapid, focused history must direct the EP early in the evaluation. Surrounding context and events as well as injury mechanism and presenting symptoms should be elicited. For example, elderly patients frequently present after falls and may have additional systemic injuries and an underlying condition that may have precipitated the fall. There are four mechanisms of ocular trauma: abrasion, blunt force, laceration or penetration with a foreign body (FB), and burn. Prognosis may be linked to mechanism, as lacerations generally have better outcomes than blunt trauma that may contuse or rupture the globe (2).
ED EVALUATION
When evaluating eye trauma, the EP should consider concomitant nonocular injuries. Rapid primary assessment of airway, breathing, circulation, and disability before conducting a systematic and comprehensive eye evaluation will address this possibility. After determining patient stability, ocular trauma is addressed as immediate treatment is imperative in many instances. The chemically burned eye must be irrigated immediately and continuously for at least 30 minutes with 2 L of saline, lactated Ringer, or another neutral solution, until the measured pH reaches physiologic neutrality (7 to 7.4). If the pH is normal after initial irrigation, a recheck of pH every 15 minutes ensures neutral pH. Traumatic endophthalmitis usually presents as pain and inflammation out of proportion to the penetrating injury preceding the infection. It requires immediate ophthalmologic consultation for injection of intravitreal antibiotics.
Visual Acuity
Visual acuity is the single most important predictor of visual outcome and is documented as soon as possible. It is helpful if a baseline acuity can be obtained by history or medical records. The EP should test one eye at a time while covering the opposite eye, beginning with the affected eye. Corrective lenses are worn when possible; if not available, a piece of paper with multiple pinholes (pinhole acuity) can be used. Contact lenses should not be placed in an injured eye. The EP should test routine distant visual acuity at 20 ft from a Snellen chart. Emergent assessment of visual function includes an assessment of light perception, hand motion, finger counting, ability to read print (the distance should be noted), and formal near vision (14 in from a Rosenbaum card). Children require some special consideration. From age 6 months to 3 years, fixing on a moving light source corresponds to 20/40 vision. From age 3 years to 6 years, Allen pictures are used or the “E” chart for those who cannot read. Formal visual acuity should never delay important therapeutic interventions such as eye irrigation (3).
Lids and Other Periorbital Structures
The lids and periorbital structures should be examined for injury (Fig. 25.1). When there is any suspicion of an open globe secondary to blunt or penetrating trauma, no pressure or object is applied to the globe thereafter for any part of the examination. An exception is bedside ultrasonography (no pressure applied) performed by an experienced examiner in selected patients. The EP should inspect for swelling, ecchymosis, proptosis, enophthalmos, ptosis, lacerations, and FB. If the eye is swollen shut, ultrasonography or lid retraction is used to assess the globe and underlying structures. Ptosis suggests contusion or laceration of the levator palpebrae, Horner syndrome, or third nerve palsy. Upper lid lacerations should be explored for penetration of the tarsal plate, the muscle, or the entire structure (through and through). All three indicate significant force and raise concern for globe injury. Any visible surface FBs should be removed. Penetrating FBs should be left for an ophthalmic surgeon to address. The EP should palpate the orbital rim and soft tissues and the zygomatic arch area, noting point tenderness, step-offs, and subcutaneous emphysema.
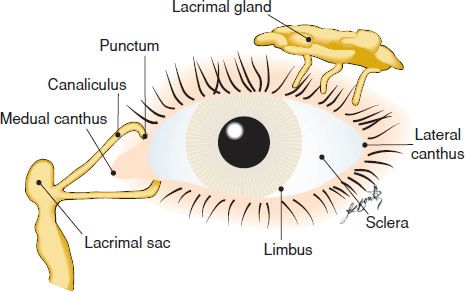
FIGURE 25.1 Periorbital structures.
Anterior Segment
The anterior segment of the eye includes the sclera, conjunctiva, cornea, anterior chamber, iris, and lens (Fig. 25.2). A topical anesthetic is used to examine this part of the eye, generally two drops are adequate, but may be augmented with one to two additional drops. The EP should inspect for globe laceration, FBs, subconjunctival hemorrhage, chemosis, limbal edema, lid laceration, and contact lenses (these should be removed). Nonadherent FBs should be evacuated as soon as they are identified. The EP should perform a slit-lamp examination to evaluate each anterior chamber component separately: globe, lid margins, cornea, anterior chamber, iris, and lens. A cobalt light and fluorescein dye will highlight abrasions on the cornea and are necessary to perform Seidel test for leaking aqueous.
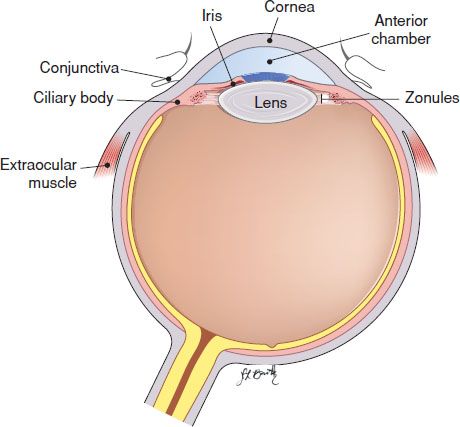
FIGURE 25.2 Cross section of the eye.
Pupils
Pupils provide information via their size, shape, and reaction. The EP should inspect for anisocoria and pupillary distortion. Anisocoria is defined as a disparity in size >0.3 to 1 mm. If pupils react briskly and the degree of anisocoria is unchanged with and without bright light, the anisocoria is physiologic. A distorted pupil suggests globe rupture, iridectomy, or synechiae. In a ruptured globe, the pupil is tear shaped, with the apex of the teardrop pointing toward the rupture. A relative afferent pupillary defect (RAPD) suggests one or more of the following: efferent third nerve damage, glaucoma, iris incarceration, massive internal derangement of the eye (trauma to the eye so severe that light pathways are disrupted), optic chiasm or tract damage, optic nerve damage, retinal detachment, traumatic mydriasis, or vitreous hemorrhage. To test for RAPD, the EP should observe pupil symmetry and size of the unaffected eye while swinging a bright light from eye to eye. When the light strikes the unaffected eye, the pupil constricts. When the light strikes the affected eye, the pupil of the unaffected eye paradoxically dilates.
Extraocular Muscles
Extraocular muscles are tested in the six cardinal positions of gaze. Lateral rectus is innervated by cranial nerve (CN) VI, superior oblique by CN IV (LR6 SO4), and the remainder by CN III. Keys, a light, or toys should be used with infants. Binocular diplopia is seen with an abscess, cellulitis, CN palsy, hematoma compressing the globe or anterior chamber (retro-orbital hematoma or a large external eyelid hematoma), orbital edema, orbital floor or wall fracture with muscle entrapment, or retrobulbar hemorrhage. Monocular diplopia is seen in conditions that distort structures through which light must pass (corneal irregularity, dislocated lens [natural or implant], iridodialysis, or retinal detachment).
Posterior Segment
The posterior segment consists of the optic nerve, retina, and vitreous. Direct ophthalmoscopic examination yields limited but important information. Pupillary dilation is not necessary. Absence of the red reflex or inability to visualize the fundus suggests cataract, hyphema, lens rupture, retinal detachment, or vitreous hemorrhage. Visual field testing by confrontation is sufficient in the ED. Optic nerve function is assessed by testing for RAPD. If the pupils are nonreactive or irregular, red desaturation testing is a suitable substitute. To test red desaturation, the EP should ask the patient to view a bright red object with each eye separately and compare the two images. If the optic nerve is damaged in one eye, the image coming from that eye will appear gray or washed out in comparison to the unaffected eye.
Intraocular Pressure
The intraocular pressure (IOP) may be elevated (>22 mm Hg) in several conditions, including acute glaucoma, globe rupture, hyphema, lens dislocation or swelling, suprachoroidal hemorrhage, and retrobulbar hemorrhage. Normal pressure ranges from 10 to 20 mm Hg (4). IOP measurement is contraindicated if a globe penetration is suspected. When the pressure is <5 mm Hg, penetration of the globe is likely.
Imaging of the Eye
Spiral computed tomographic (CT) scan with axial and coronal cuts is the preferred study when there is suspected injury to the orbit or globe. Plain x-ray has been replaced by CT as the primary radiologic diagnostic tool, as x-ray is unreliable for detecting small (0.2 to 1.5 mm) and nonmetallic FBs (60% false-negative rate), nor is it precise in determining the location of an FB. CT can also identify choroidal detachment, endophthalmitis, fracture, extraocular hemorrhage or hematoma (<3 days old), lens luxation or subluxation, globe rupture, orbital cellulitis, subperiosteal hematoma, vitreous hemorrhage (<3 days old), and retinal detachment. Bedside ultrasound performed by EPs with training and experience has been shown to be highly accurate and useful in diagnosing ocular pathology including FBs (as small as 0.2 mm), retinal detachment, lens dislocation, and vitreous hemorrhage (eFig. 25.1) (5).
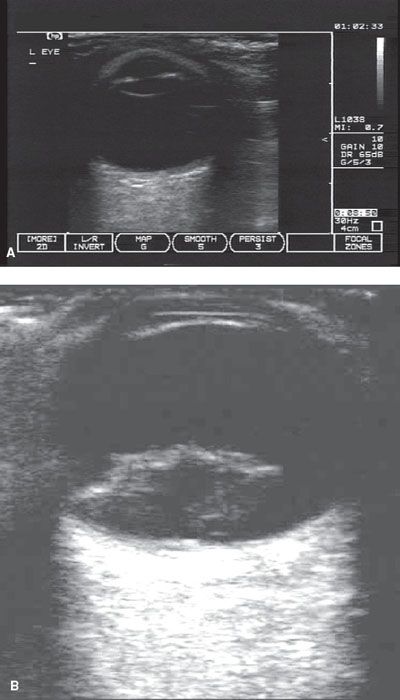
eFIGURE 25.1 Emergency bedside ultrasonography of the eye is obtained with minimal pressure on the eye. A: A normal eye is shown with lid, anterior chamber, iris, lens capsule, and vitreous clearly seen. B: A retinal detachment is seen as a hyperechoic area anterior to the retina.
KEY TESTING
Physical examination
• Visual acuity
• Lids and periorbital structures
• Anterior segment
• Pupils
• Extraocular muscles
• Posterior segment
• IOP
Imaging
• CT for detecting FBs and orbital injuries
• Ultrasound for detecting retinal detachment, lens dislocation, and vitreous hemorrhage
ED MANAGEMENT
Subconjunctival Hemorrhage
Typically, an isolated subconjunctival hemorrhage is flat and involves a small portion of the bulbar conjunctiva without any break in the membrane. The history may reveal a related Valsalva maneuver or rubbing of the eye but often does not explain the event. There may not be a history of anticoagulant use, blood dyscrasia, or recurrent subconjunctival hemorrhage. No treatment is necessary as the condition is not threatening to the orbit or globe and will resolve over approximately 14 days. Bulging circumferential bloody chemosis after trauma should alert the EP to the possibility of a ruptured globe.
Simple Eyelid Lacerations and Periorbital Contusion
Eyelid laceration or periorbital contusion mandates a thorough evaluation to rule out involvement of the globe or associated structures. Periorbital contusion is generally managed with ice packs. Concurrent intracranial injury must be ruled out based on history and examination. Instructions for head injury and visual changes are given. Resolution of a simple contusion can take 2 to 3 weeks, whereas hemorrhage into the levator palpebrae may produce ptosis that can last for months. A simple eyelid laceration involves neither underlying structures nor the lid margin and can be repaired by the EP. Contaminated wounds must be irrigated without force against the underlying globe. No tissue should be debrided, owing to the excellent blood supply of the eyelid and desire for cosmetic and functional integrity. Wound closure is accomplished with single interrupted sutures of 6-0 or 7-0 nonabsorbable material, which are removed in 5 days. For contaminated wounds, parenteral antibiotics to cover Staphylococcus and Streptococcus are administered in the ED and oral antibiotics prescribed for 7 to 10 days. Unless trauma was minimal, the patient requires referral to an ophthalmologist for follow-up evaluation.
Complex Eyelid Lacerations and Other Penetrating Trauma
At the first evidence of globe penetration, the EP should document visual acuity, shield the eye, and consult an ophthalmologist. Any protruding penetrating objects are left in place and protected from manipulation until an ophthalmologic surgeon assumes management of the injury. Penetrating wounds near the eye are assumed to have penetrated the globe until proven otherwise.
Isolated lacerations of the conjunctiva are benign; however, laceration of the sclera or full thickness of the cornea is regarded as a penetrating injury. When the cornea is injured, the iris plugs the wound and distorts the pupil into a teardrop shape, with the apex of the drop pointing toward the wound (Fig. 25.3). When there is doubt regarding globe penetration, Seidel test is performed. Fluorescein is instilled onto the eye and observed for a fluid stream leaking from the globe under cobalt light. Parenteral antibiotics should be administered prophylactically to help prevent endophthalmitis. All penetrating eye wounds require an emergent ophthalmologic consultation.
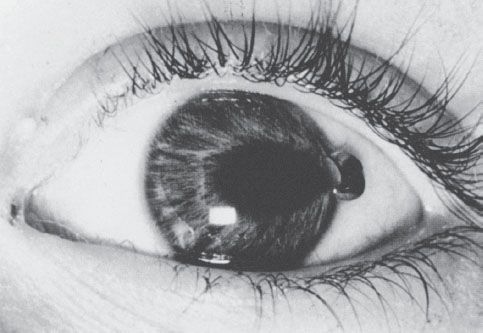
FIGURE 25.3 Penetrating corneal foreign body with entrapment of the iris, forming a teardrop pupil.
Complex eyelid lacerations should be repaired by an ophthalmologic surgeon. These wounds are characterized by exposed orbital fat, globe penetration, muscle laceration, nasolacrimal system damage, tarsal plate laceration, or through-and-through laceration. With any periorbital wound, it is imperative that the lids be retracted to rule out globe penetration. Injury to the nasolacrimal duct system is considered when wounds are in close proximity to the anatomic location in the medial eyelids, extending laterally 5 to 7 mm from the medial canthus. Medial to the canthus, the system runs vertically into the nose. A parenteral antibiotic to cover Staphylococcus and Streptococcus should be administered prophylactically. Wounds should be covered with a sterile saline dressing to keep the tissues moist until the ophthalmologist arrives.
Blowout Fractures and Other Facial Fractures
When a ball, fist, or other object larger than the orbital rim strikes the eye, a blowout or other facial fracture may result. Suggestive complaints and findings are diplopia, enophthalmos, epistaxis, inferior displacement of the globe, ipsilateral numbness of the cheek and the upper lip, point tenderness of the orbital rim or maxilla, palpable step-off, periorbital ecchymosis, swelling, or even subcutaneous emphysema when sinuses are affected. Plain films have been used for diagnosis but can be falsely negative (≥60%) or falsely positive (≥46%) (6). A spiral CT scan with coronal cuts is preferred for diagnosis. Most blowout fractures involve the inferior or medial walls of the orbit. Involvement of the roof of the orbit signals that considerably more force was sustained and suggests violation of the cranial vault with associated injury to the brain.
Facial injuries such as Le Fort, tripod, and nasal fractures may have an associated eye injury. At the minimum, for an apparently uninvolved eye, the EP should document visual acuity, extraocular movement, the absence of any obvious trauma, and absence of visual symptoms. See Chapter 23 for further discussion of facial trauma.
Management consists of oromaxillofacial and ophthalmologic referral, antibiotics (to cover Staphylococcus and Streptococcus) for 10 to 14 days, ice packs, nasal decongestant spray, and avoidance of blowing the nose. Surgical repair may be delayed for up to 14 days. The vast majority of blowout fractures will resolve without surgical intervention (7). Urgent ophthalmology referral is indicated for injuries with entrapment or obvious injury to the globe or anterior chamber. Close ophthalmology follow-up is indicated for all others so that occult injuries can be identified.
Burns
Chemical, electrical, infrared, thermal, and ultraviolet (UV) burns may affect the eye. Chemical burns are irrigated immediately with saline for at least 30 minutes. “Time is sight,” and irrigation at the scene is often inadequate. Triage and registration should not further delay immediate and thorough irrigation upon ED presentation. Copious irrigation should continue uninterrupted for at least 20 minutes in the ED. The local poison control center should be contacted for assistance in characterization of the chemical in question, its pH, and its potential to cause ocular damage. After irrigation is completed (defined as normal serial pH testing of the affected eye for at least 10 minutes after irrigation has stopped), the EP should then examine the eye. Alkali burns are particularly devastating. They destroy tissue via liquefaction necrosis and are classified by four grades of involvement:
1. Corneal epithelial damage similar to a corneal abrasion with a good prognosis.
2. Cornea hazy but the details of the iris are seen and up to one-third of the limbus is ischemic (whitened). The prognosis is still good.
3. Corneal epithelium is destroyed, and the details of the iris are blurred; one-third to one-half of the limbus is ischemic. The prognosis is guarded.
4. Cornea is opaque, and the details of the iris and pupil are obscured; more than half of the limbus is ischemic. The prognosis is poor.
Acid burns are classified with the same severity grades; however, they tend to produce less extensive damage, as strong acids precipitate proteins via coagulation necrosis, which may form a barrier to further spread.
For severe chemical burns, all foreign matter should be removed prior to irrigation by sweeping the fornices with a moistened cotton-tipped applicator. Calcium hydroxide tends to cake and may be easier to remove if the applicator is moistened with 10% ethylenediaminetetraacetic acid (EDTA). Minimal irritation and lack of symptoms after irrigation require no further follow-up. Moderate irritation with persistent symptoms requires instillation of antibiotic ointment and referral to an ophthalmologist in 24 hours. Any injury producing more than moderate irritation and having associated significant changes in vision mandates immediate consultation with an ophthalmologist.
Electrical burns are rare; however, the injury may be indirect. Nine percent of patients experiencing electrical injuries involving the head develop cataracts 6 to 12 months after the injury. Infrared radiation can produce keratitis, macular damage, or “glassblower’s cataract” (a heat injury that damages the anterior lens capsule of unprotected glassblowers) after prolonged exposure to heat. Thermal burns are rare, as the light of a heat flash reaches the eye faster, producing the upward rotation reflex of the globe (Bell phenomenon), which protects the cornea from damage. Thermal corneal injury occurs when hot objects, such as lighted matches, spitting grease, or car radiator steam, are propelled into the eye. These burns rarely involve more than the corneal epithelium and heal in a few days. Treatment involves the application of cold compresses for up to 2 hours. For partial-thickness burns of the lids and surrounding skin, ophthalmic antibiotic ointment is applied. Minor burns of the cornea are managed similarly to a corneal abrasion. For more severe burns, an ophthalmologist is consulted immediately. UV radiation from the sun, tanning salons, or a welder’s arc produces acute, diffuse, superficial punctate keratitis of the corneal epithelium about 6 to 12 hours after exposure. The amount of UV radiation is enhanced by reflection off of water, rocks, or snow and at altitudes above 8,000 ft (2,438 m). Prolonged exposure may damage the retina, particularly the fovea, and visual changes may manifest up to 1 to 2 days later (8). Management is similar to that of a corneal abrasion. A nonsteroidal anti-inflammatory medication and narcotic-containing analgesic are prescribed. Ophthalmologic follow-up for all burns of the eye is essential unless the injury is minimal.
Corneal and Conjunctival Injuries
The corneal epithelium is 4 to 6 cells thick, and abrasions generally heal in 12 to 36 hours, sometimes longer, depending on the injury. Full-thickness injuries require prompt surgical repair. Further examination is deferred. Evidence of full-thickness injuries may include a positive Seidel test, an irregular pupil with or without iris prolapse, shallow anterior chamber, cataract, hyphema, or microhyphema. Infection is a risk with any wound, and a retained FB heightens that risk. Consider tetanus prophylaxis for susceptible wounds. Iron-containing FBs will leave a rust ring deposit after being in place for a couple of hours. Rust rings extrude to the surface over 48 hours, where they are easily removed with an ophthalmic burr.
Corneal abrasions usually present as an FB sensation. Often, there is a history of something striking the eye. Exposure to high-speed particles raises the suspicion for a penetrating eye injury. In addition to an FB sensation, symptoms include blepharospasm, blurred vision, eye pain, halos around lights, photophobia, red eye, and tearing. Visual acuity is mildly decreased. The eye is hyperemic, eyelids mildly swollen, and an anterior chamber reaction (cells or flare) is sometimes noted. Abrasions are highlighted by fluorescein and are best seen on slit-lamp examination. A handheld cobalt light in a darkened room may be used for minor abrasions but will miss more subtle findings such as anterior chamber reaction or corneal microperforation. Soft contact lenses should be removed prior to fluorescein instillation. The EP should evert the upper lid to examine for FBs. Low-mass, low-speed particles largely produce insignificant trauma without anterior chamber reaction; therefore, the IOP does not need to be measured. When larger objects, such as a finger, fist, or ball, strike the eye, the IOP should be measured. After instilling anesthetic ophthalmic drops, removal of an FB is accomplished by either gentle irrigation, a saline-moistened cotton-tipped applicator (brush off ), an ophthalmic burr, or a 25-gauge needle held tangential to the corneal surface (pick off ). Rust ring removal is accomplished with an ophthalmic burr. The EP should consider instilling a short-acting cycloplegic (one to two drops) to reduce ciliary muscle spasm and synechiae formation secondary to inflammation. Patching is not shown to improve healing rates or reduce pain and thus are generally not used (9). Despite a lack of supporting evidence, ophthalmic antibiotics are often prescribed. Analgesics include a nonsteroidal anti- inflammatory medication (daily dosing for 3 days) and a narcotic as needed. Patients who wear contact lenses or those with large or centrally located abrasions are followed up closely by an ophthalmologist, usually at 1-day interval, until healed. EPs can follow up these corneal abrasions, but referral to an ophthalmologist the next day is advisable.
Contact lens usage can lead to a corneal symptom complex similar to corneal abrasions. Contact lens–related corneal abrasions, due to overwear or improper fit, result from hypoxic injury, toxic deposits under the lens, or trauma related to insertion or removal of the lens. Infectious keratitis with gram-negative bacterial organisms, particularly Pseudomonas, and protozoa, specifically Acanthamoeba, may occur as well. Chemical irritation may result from preservatives such as thimerosal and chlorhexidine and inadequate rinsing of lenses after enzyme use. Tight lens syndrome occurs within 2 days of placement of the offending lens. The lens appears “sucked-on,” leaving a conjunctival imprint after lens removal. Other complications of contact lens use include corneal ulceration, superficial punctate keratitis, anterior uveitis, and infrequently, hypopyon. Treatment begins with removal of the contact lens; fluorescein will permanently stain the lens. An antipseudomonal ophthalmic antibiotic preparation should be prescribed. A cycloplegic should be used if needed. The patient should follow up with an ophthalmologist within 24 hours. (See Chapter 57.)
Conjunctival and subconjunctival injuries are minor when the underlying sclera remains intact because the conjunctiva does not provide any structural support to the eye. Visual acuity is usually unaffected. There may be an associated corneal injury, exhibiting the usual corneal symptoms. All conjunctival wounds, with or without an associated FB, must be examined under magnification for scleral penetration. The EP should anesthetize the eye and tease the wound with a cotton-tipped applicator, observing for exposed white scleral tissue. Seidel test can provide additional information. If there is any doubt regarding penetration of the sclera, the injury is managed as though there has been violation of the globe, and an ophthalmologist is consulted immediately. The EP should remove FBs from the fornices by handheld irrigation or forniceal sweeping with a saline-moistened cotton-tipped applicator after anesthetizing the eye. Although commonly practiced, there is no evidence to support empiric antibiotic treatment. The patient should be referred to an ophthalmologist for next day follow-up.
Other Anterior Segment Injuries
Blunt and penetrating forces inflame, contuse, lacerate, rupture, stretch, and tear the tissues of the anterior segment of the eye, resulting in various injuries such as hyphema, glaucoma, lens displacement, and cataracts. When these conditions are suspected, an ophthalmologist should be consulted immediately.
Traumatic iritis occurs in up to 18% of eye trauma (10). Synonyms for this condition are anterior chamber reaction, anterior uveitis, uveitis, and iridocyclitis. Inflammation in the anterior segment of the eye results in symptoms of blurred vision, impaired visual acuity, pain, photophobia, hyperemia, and tearing; symptoms vary from mild to severe. The pain of ciliary spasm is exacerbated by light shining in either eye (photophobia) or with accommodation, which increases ciliary muscle contraction (11). When light strikes the unaffected eye, the consensual response exacerbates the pain (consensual photophobia). Protein and white blood cells are visible by slit lamp in the anterior chamber. The limbus is injected. In severe reactions, there may be hypopyon (a layer of white blood cells seen in the anterior chamber). The IOP may be increased or decreased. Treatment includes a short-acting cycloplegic, a nonsteroidal anti-inflammatory medication (for 3 days), and a narcotic analgesic. The patient should be referred for ophthalmologic follow-up within 36 hours.
Hyphema may be microscopic (cells visualized only by slit lamp) or gross (characterized by the percentage of the anterior chamber that is filled) (Fig. 25.4). If blood fills the chamber entirely, it is commonly called an “eight-ball” hyphema. Symptoms include pain, red eye, and blurred vision. Treatment begins by shielding the eye and elevating the head to 30 degrees. Medications, other than those for pain and nausea, are administered only at the direction of an ophthalmologist. Rebleeding occurs in approximately 30% of cases. Outpatient management may be appropriate for some microhyphemas and in compliant patients with good follow-up and no risk factors for complications (e.g., sickle cell disease or bleeding diathesis). Which patients to hospitalize is controversial and should be discussed with an ophthalmologist. Many ophthalmologists manage uncomplicated small hyphemas (<25% of the anterior chamber) without hospital admission. When there is a history of sickle cell disease or trait and IOP is >25 mm Hg, the anterior chamber may need to be washed out (12).

FIGURE 25.4 Traumatic hyphema (20%) with blood layering in the anterior chamber, subsequent to blunt trauma.









