EYE: STRABISMUS
ATIMA C. DELANEY, MD AND ALEX V. LEVIN, MD, MHSc, FRCSC
Strabismus refers to any misalignment of the eyes such that they are not viewing in the same direction. Esotropia refers to eyes that are turned in (cross-eyed). Exotropia refers to eyes that are turned out (wall eyed). The terms hypertropia and hypotropia refer to a higher or lower eye, respectively. By convention, vertical misalignment of the eyes is always categorized by the higher eye (e.g., right hypertropia), unless it is known that a specific abnormal process is causing one eye to be held in a lower position (e.g., left hypotropia). Many children with strabismus require a formal evaluation by an ophthalmologist for definitive diagnosis and management, but the emergency physician should attempt to answer two questions: (1) “Is the strabismus an emergency?” and, if so, (2) “What is the most likely cause?”
PATHOPHYSIOLOGY
Six muscles surround each eyeball (Fig. 23.1). Although several of these muscles may individually move the eye in more than one direction, knowledge of the primary action of these muscles allows for the definition of diagnostic positions of gaze (Table 23.1). This can be helpful in pinpointing specific muscle dysfunction. For example, if a muscle that primarily governs abduction (e.g., lateral rectus) is impaired, the eye is unable to abduct and will usually lie in a position of adduction (esotropia). Likewise, if a muscle that is involved with downward gaze (e.g., inferior rectus) is impaired, the eye will have a tendency to remain in relative upward gaze (ipsilateral hypertropia).
Strabismus is categorized into misalignment as a result of impaired muscle function or misalignment in the presence of full-normal muscle function. In general, there are only two emergent reasons why the function of a particular muscle might be impaired: Neurogenic palsy or muscle restriction.
Three cranial nerves are responsible for the innervation of the six extraocular muscles (Table 23.1). The sixth cranial nerve innervates the ipsilateral lateral rectus muscle. This nerve exits the ventral pons and then travels on the wall of the middle cranial fossa (clivus), reaching the sphenoid ridge, along which it travels until entering the cavernous sinus. The course of this nerve allows it to be injured by vascular or neoplastic changes in the midbrain, increased intracranial pressure (ICP), large anterior midline craniofacial tumors (e.g., nasopharyngeal carcinoma), otitis media (OM) with involvement of the petrous portion of the sphenoid (Gradenigo syndrome), and any abnormality that involves the cavernous sinus. An abnormality of the sixth cranial nerve will cause a reduction in ipsilateral abduction (Fig. 23.2) resulting in a possible ipsilateral esotropia.
The fourth cranial nerve innervates the superior oblique muscle. It is the only cranial nerve that completely decussates and has a dorsal projection over the midbrain. This position renders the fourth cranial nerve particularly vulnerable to blunt head trauma, one of the most common causes of fourth nerve palsy. The fourth cranial nerve also has a relatively long intracranial course, which makes it particularly susceptible to increased ICP and parenchymal shifts caused by cerebral edema. It also runs through the cavernous sinus. Fourth cranial nerve palsy may be congenital but asymptomatic for several years during childhood until the brain is no longer able to compensate. Acquired or congenital palsy of this cranial nerve causes the eyes to become misaligned vertically (ipsilateral hypertropia). Patients with congenital fourth cranial nerve paresis compensate by tilting their head to the ipsilateral side, which allows for a rebalancing of the eye muscles such that alignment may be achieved. Old photographs may demonstrate this tilt. Facial asymmetry can also be seen after years of this compensatory tilting. Ophthalmic consultation is usually needed to differentiate between congenital and acquired palsy.
The third cranial nerve supplies the remaining four extraocular muscles. It is involved with downgaze, upgaze, and adduction. Parasympathetic innervation to the pupil (see Chapter 24 Eye: Unequal Pupils) and innervation to the eyelid muscle (levator palpebrae) are also carried in the third cranial nerve. A complete third cranial nerve palsy results in an eye that is positioned down (from the remaining action of the unaffected superior oblique muscle) and out (from the remaining action of the unaffected lateral rectus muscle) with ipsilateral ptosis and ipsilateral pupillary dilation (Fig. 23.3). Because the third cranial nerve divides into a superior and an inferior division just as it enters the orbit from the cavernous sinus and because the fibers to individual muscles are segregated within the nerve throughout its course, partial third cranial nerve palsies may occur with or without ptosis and/or pupillary dilation. This may leave the patient with complex strabismus, which is best left to the ophthalmology consultant. The differential diagnosis of third cranial nerve palsies is summarized in Chapter 24 Eye: Unequal Pupils.
The action of a muscle may also be impaired by restriction. The muscle can become infiltrated with substances that might restrict its action or cause fibrosis. Children with hyperthyroid eye disease (e.g., Graves) can have large, tight eye muscles. An eyeball may also be restricted in its movements by tumors or infection in and around the globe. Orbital tumors, cellulitis, or abscesses that cause restriction may be associated with proptosis or a displacement of the entire eyeball, either vertically or horizontally. After blunt trauma to the eyeball, the globe may be translocated posteriorly, causing an increased intraorbital pressure that may result in a “blowout” fracture of the bony orbital wall. When an orbital wall fracture occurs, the muscle or surrounding tissues that run along that wall may become entrapped within that fracture, tethering the eyeball so the eye cannot look in the direction opposite the fracture. Children with orbital floor or medial orbital wall fracture are prone to entrapment of the inferior or medial rectus muscles, respectively. This may not be noticeable until eye movements are attempted. For example, fractures of the orbital floor may entrap the inferior rectus muscle, tethering the eye downward so upgaze is restricted (Fig. 23.4). Less commonly, the eye may have a limitation of movement in the direction of the fracture. Orbital wall fractures may also be associated with enophthalmos, in which the eye appears to be sunken in the orbit, or proptosis caused by orbital hemorrhage. All patients with orbital fractures must receive a complete ophthalmic examination to rule out accompanying ocular injury. The most common fracture involves the inferior and/or medial walls of the orbit. The lateral wall is rarely fractured. Fracture of the superior wall (orbital roof) is particularly worrisome because it may allow communication between the orbit and the subfrontal intracranial space.
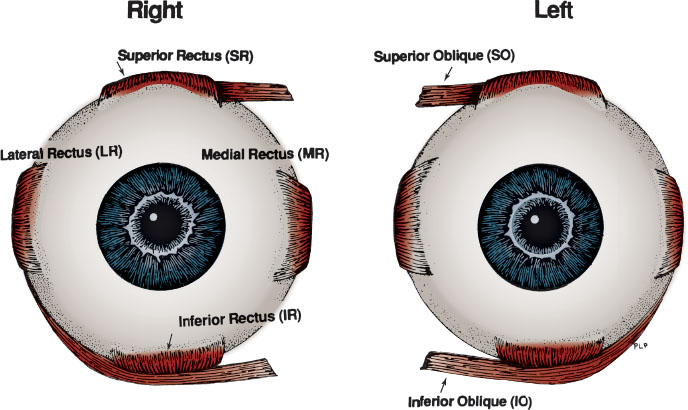
FIGURE 23.1 Normal extraocular muscle anatomy.
The remaining types of strabismus fall into the category where eye muscle function is unimpaired (nonrestrictive and nonparalytic). These problems are not emergent. The eyes may be misaligned as a result of failure of the brain to use both eyes simultaneously in a coordinated fashion (idiopathic), a need for glasses, or the presence of poor vision in one eye. Uncorrected farsightedness (hyperopia) can result in accommodative esotropia, which may have an acute onset, usually between the ages of 2 and 6 years, with the misalignment often worse at near viewing. Uncorrected nearsightedness (myopia) can result in exotropia, especially when the patient views in the far distance. Both types of misalignment may be treated with glasses.
Checking the vision in both eyes (see Chapter 131 Ophthalmic Emergencies
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







